Chapter 8
Intrapartum Fetal Assessment and Therapy
Elizabeth G. Livingston MD
Chapter Outline
The value of intrapartum obstetric interventions to assess and maintain fetal well-being has been scrutinized in recent years. Old technologies have been reassessed, and new ones have been introduced. A rising cesarean delivery rate, renewed interest in home birth, persistent cases of fetal/neonatal neurologic injury, and excessive litigation have prompted an ongoing search for methods to identify and intervene on behalf of the fetus at risk during labor and delivery.
Fetal Risk during Labor
Historical epidemiologic data suggest that the fetus is at increased risk for morbidity and mortality during labor and delivery. In 1963, the British Perinatal Mortality Survey reviewed autopsy data for 1400 stillborn infants and concluded that slightly more than 30% of these losses resulted from intrapartum asphyxia.1 Neonatal outcomes in the industrialized world have improved over the past 40 years. A Canadian database identified approximately 80 intrapartum stillbirths per 120,000 live births from 1981 to 2002, a rate of 0.67/1000; some 11 of the infants were considered viable (i.e., not severely preterm or anomalous), which indicated a preventable death rate of 0.09/1000.2 A Scottish study indicated that perinatal deaths due to intrapartum anoxia in term, singleton, cephalic infants declined significantly from 5.7 to 3.0/10,000 births between 1988 and 2007.3 Intrapartum stillbirths are rare in developed countries, constituting less than 10% of all stillbirths. By contrast, in some developing countries, as many as 50% of stillbirths occur intrapartum.4 According to a World Health Organization report, intrapartum-related neonatal deaths account for almost 10% of deaths in children younger than 5 years of age.5,6
Experimental models lend support to the hypothesis that intrapartum events can have long-term neurologic sequelae. Fetal monkeys subjected to hypoxia in utero suffer neurologic injuries similar to those seen in children who presumably suffered asphyxia in utero.7–9 Work with rodent models has shown similar patterns of damage.10 Hankins et al.11 suggested that performance of elective cesarean delivery at 39 weeks’ gestation (and avoidance of a trial of labor) might result in an 83% reduction in risk for moderate or severe neonatal encephalopathy. Altogether, epidemiologic and experimental data suggest that the fetus is at significant risk during labor and delivery.
Some fetuses appear to be at greater risk for adverse intrapartum events than others. Older studies report that high-risk mothers constitute 20% of the pregnant population, but their offspring represent 50% of the cases of perinatal morbidity and mortality.12 Various schemes to identify high-risk pregnancies have been published.13,14 High-risk pregnancies include, but are not limited to, women with (1) medical complications (e.g., hypertension, preeclampsia, diabetes, autoimmune disease, hemoglobinopathy); (2) fetal complications (e.g., fetal growth restriction [also known as intrauterine growth restriction], nonlethal anomalies, prematurity, multiple gestation, postdatism, hydrops); and (3) intrapartum complications (e.g., abnormal vaginal bleeding, maternal fever, meconium-stained amniotic fluid, oxytocin augmentation of labor). Owing to inadequate sensitivity, poor positive predictive values, and the inability to modify outcomes related to risk factors, scoring systems for identifying high-risk fetuses have not been shown to improve pregnancy outcomes.15 Lo et al.16 indicated that more than half of infants with asphyxia had no clinical risk factors. However, for low-risk parturients who wish to avoid continuous monitoring during labor, scoring systems may demonstrate some benefit.15 One strategy used in European centers for identifying high-risk parturients is fetal heart rate (FHR) tracing analysis at the time of admission to the labor and delivery suite; if the FHR tracing is abnormal, patients receive more intensive monitoring.17 A meta-analysis of this approach observed an increase in cesarean delivery rates but failed to demonstrate improvements in fetal and neonatal outcomes.18
The magnitude of risk for intrapartum fetal neurologic injury is a matter of some dispute. In 2003, the American College of Obstetricians and Gynecologists (ACOG) Task Force on Neonatal Encephalopathy and Cerebral Palsy concluded that 70% of these types of fetal neurologic injuries result from events that occur before the onset of labor.19–21 Examples of antepartum events that may cause fetal neurologic injury include congenital anomalies, chemical exposure, infection, and fetal thrombosis/coagulopathy. Only 4% of cases of neonatal encephalopathy result solely from intrapartum hypoxia, an incidence of approximately 1.6/1000.19,20,22 The Task Force identified criteria that define an acute intrapartum hypoxic event sufficient to cause cerebral palsy (Box 8-1).19,20,23 A recent study found that fetuses that underwent a sudden and sustained deterioration of the FHR and that subsequently had a diagnosis of cerebral palsy demonstrated characteristics consistent with the criteria developed by the ACOG Task Force.24 An additional case series of sentinel events during labor (e.g., uterine rupture, cord prolapse, placental abruption, amniotic fluid embolus) resulted in a high rate of hypoxic-ischemic encephalopathy in surviving infants.25 Approximately 25% of fetuses may have antepartum and intrapartum risk factors for neurologic injury.
The ability of contemporary obstetricians to recognize and treat pregnancies at risk for hypoxia during labor is an evolving science. With the current understanding of pathophysiology and the technology in current clinical use, the extent to which obstetricians can prevent intrapartum injury is unclear.26 It is hoped that the development of standardized, clearer definitions of intrapartum injury, and new strategies and interventions that can correct reversible pathophysiology, will lead to more precise identification and optimization of fetuses at risk.
Efforts to understand placental physiology and pathophysiology are central to the efforts to support the health of the pregnant woman and her fetus, both antepartum and intrapartum. The fetus depends on the placenta for the diffusion of nutrients and for respiratory gas exchange. Many factors affect placental transfer, including concentration gradients, villus surface area, placental permeability, and placental metabolism (see Chapter 4). Maternal hypertensive disease, congenital anomalies, and intrauterine infection are examples of conditions that may impair placental transfer.
One of the most important determinants of placental function is uterine blood flow.27 A uterine contraction results in a transient decrease in uteroplacental blood flow. A placenta with borderline function before labor may be unable to maintain gas exchange adequate to prevent fetal asphyxia during labor. The healthy fetus may compensate for the effects of hypoxia during labor.28,29 The compensatory response includes (1) decreased oxygen consumption, (2) vasoconstriction of nonessential vascular beds, and (3) redistribution of blood flow to the vital organs (e.g., brain, heart, adrenal glands, placenta).30,31 Humoral responses (e.g., release of epinephrine from the adrenal medulla, release of vasopressin and endogenous opioids) may enhance fetal cardiac function during hypoxia.27 Prolonged or severe hypoxia overwhelms these compensatory mechanisms, resulting in fetal injury or death.
Intrapartum Fetal Assessment
Electronic Fetal Heart Rate Monitoring
An optimal, yet practical method for assessing fetal health during labor and delivery has not been developed. Most contemporary methods include assessment of the FHR. The FHR can be monitored intermittently with a simple DeLee stethoscope. Alternatively, either Doppler ultrasonography or a fetal electrocardiographic (ECG) electrode can be used to monitor the FHR intermittently or continuously.
Experimental models have provided insight into the regulation of the FHR. Both neuronal and humoral factors affect the intrinsic FHR. Parasympathetic outflow by means of the vagus nerve decreases the FHR, whereas sympathetic activity increases FHR and cardiac output.27 Baroreceptors respond to increased blood pressure and chemoreceptors respond to decreased PaO2 and increased PaCO2 to modulate the FHR through the autonomic nervous system. Cerebral cortical activity and hypothalamic activity affect the FHR through their effects on integrative centers in the medulla oblongata (Figure 8-1).27 Both animal studies and clinical observations have helped establish a correlation between FHR and perinatal outcome.
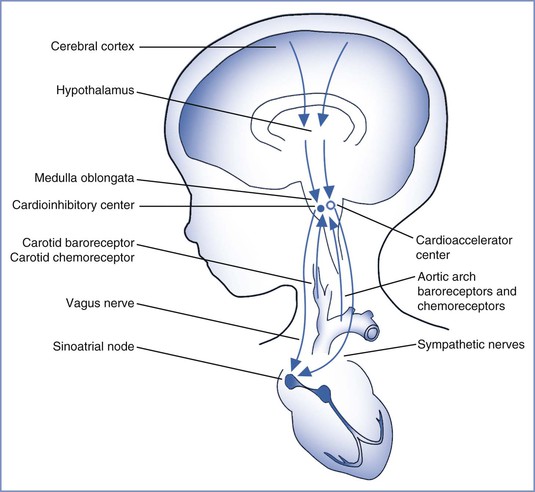
FIGURE 8-1 Regulation of fetal heart rate. (Drawing by Naveen Nathan, MD, Northwestern University Feinberg School of Medicine, Chicago, IL.)
An electronic monitor simultaneously records the FHR and uterine contractions. Use of an electronic monitor allows determination of the baseline rate and patterns of the FHR and their relationship to uterine contractions. External or internal techniques can assess the FHR and uterine contractions (Figure 8-2). Doppler ultrasonography detects the changes in ventricular wall motion and blood flow in major vessels during each cardiac cycle. The monitor calculates the FHR by measuring the intervals between fetal myocardial contractions. Alternatively, an ECG lead attached to the fetal scalp enables the cardiotachometer to calculate the FHR by measuring each successive RR interval. Both external and internal methods allow continuous assessment of the FHR.
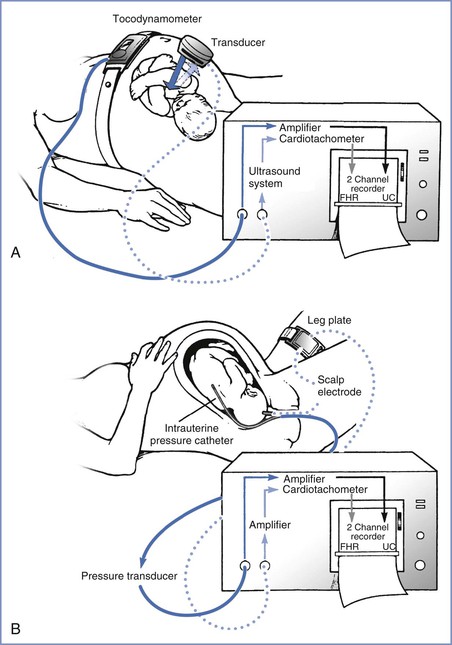
FIGURE 8-2 Electronic fetal monitoring apparatus. A, Instrumentation for external monitoring. Contractions are detected by the pressure-sensitive tocodynamometer, amplified, and then recorded. The fetal heart rate (FHR) is monitored with the Doppler ultrasound transducer, which emits and receives the reflected ultrasound signal that is then counted and recorded. B, Techniques used for direct monitoring of FHR and uterine contractions (UC). Uterine contractions are assessed with an intrauterine pressure catheter connected to a pressure transducer. This signal is then amplified and recorded. The fetal electrocardiogram (ECG) is obtained by direct application of the scalp electrode, which is then attached to a leg plate on the mother’s thigh. The signal is transmitted to the monitor, where it is amplified, counted by the cardiotachometer, and recorded. (Drawing by Naveen Nathan, MD, Northwestern University Feinberg School of Medicine, Chicago, IL.)
The FHR is superimposed over the uterine contraction pattern. Uterine contractions can be monitored externally with a tocodynamometer or internally with an intrauterine pressure catheter. The tocodynamometer allows determination of the approximate onset, duration, and offset of each uterine contraction. A normal pattern of uterine contractions in labor is five or less in a 10-minute period averaged over 30 minutes; tachysystole is defined as more than five uterine contractions within a 10-minute period.32 An intrauterine pressure catheter may be used to measure the strength of uterine contractions. In some cases, an intrauterine pressure catheter is placed to determine the precise onset and offset of each uterine contraction. Such information may be used to distinguish among early, variable, and late FHR decelerations. In a nonblinded, randomized controlled trial, Bakker et al.33 observed no significant differences in adverse neonatal outcomes with internal tocodynamometry as compared with external monitoring of uterine contractions in women in whom oxytocin was used for induction or augmentation of labor.
The following features of the FHR pattern can be assessed: (1) baseline measurements, (2) variability (the extent to which the rate changes both instantaneously and over longer periods), (3) accelerations, and (4) decelerations and their association with uterine contractions.
Baseline Fetal Heart Rate
A normal baseline FHR is defined as 110 to 160 beats per minute (bpm) and is determined by assessing the mean heart rate over a 10-minute period rounded to increments of 5 bpm.32,34 In general, term fetuses have a lower baseline FHR than preterm fetuses because of greater parasympathetic nervous system activity. Laboratory studies suggest that bradycardia (caused by increased vagal activity) is the initial fetal response to acute hypoxemia. After prolonged hypoxemia, the fetus may experience tachycardia as a result of catecholamine secretion and sympathetic nervous system activity.28 Changes in baseline FHR may also be caused by fetal anatomic or functional heart pathology, maternal fever and/or intrauterine infections, or maternally administered medications, such as beta-adrenergic receptor agonists (e.g., terbutaline) or the anticholinergic agent atropine.
Fetal Heart Rate Variability
Fetal heart rate variability is the fluctuation in the FHR of 2 cycles or greater per minute.32,34 Previously, FHR variability was divided into short term (from one beat, or R wave, to the next) and long term (occurring over the course of 1 minute), but this distinction is no longer made because in clinical practice variability is visually assessed as a unit (Figure 8-3). The presence of normal FHR variability reflects the presence of normal, intact pathways from—and within—the fetal cerebral cortex, midbrain, vagus nerve, and cardiac conduction system (see Figure 8-1).27 Variability is greatly influenced by the parasympathetic tone, by means of the vagus nerve; maternal administration of atropine, which readily crosses the placenta, can eliminate some variability. In humans, the sympathetic nervous system appears to have a lesser role in influencing variability.27 Maternal administration of the beta-adrenergic receptor antagonist propranolol has little effect on FHR variability.27
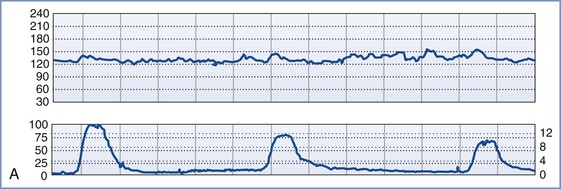
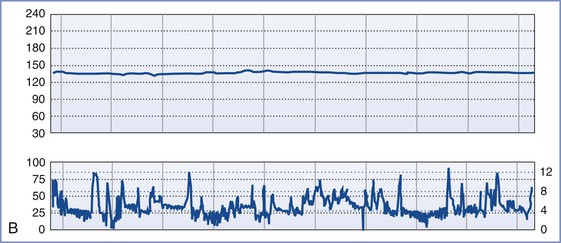
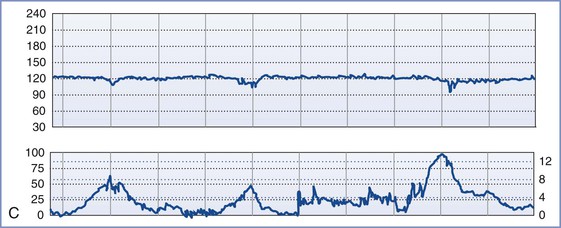
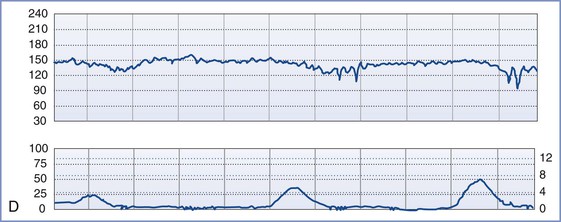
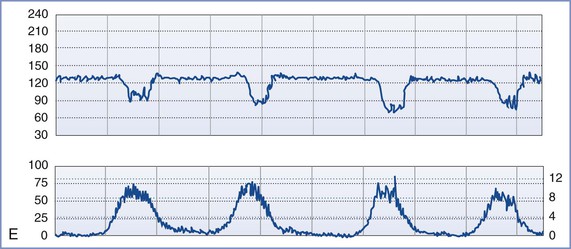
FIGURE 8-3 A, Normal intrapartum fetal heart rate (FHR) tracing. The infant had Apgar scores of 8 and 8 at 1 and 5 minutes, respectively. B, Absence of variability in a FHR tracing. Placental abruption was noted at cesarean delivery. The infant had an umbilical arterial blood pH of 6.75 and Apgar scores of 1 and 4, respectively. C, Early FHR decelerations. After a normal spontaneous vaginal delivery, the infant had Apgar scores of 8 and 8, respectively. D, Late FHR decelerations. The amniotic fluid surrounding this fetus was meconium stained. Despite the late FHR decelerations, the variability remained acceptable. The infant was delivered by cesarean delivery and had an umbilical venous blood pH of 7.30. Apgar scores were 9 and 9, respectively. E, Variable FHR decelerations. A tight nuchal cord was noted at low-forceps vaginal delivery. The infant had Apgar scores of 6 and 9, respectively. Numerical scales: Left upper panel margin, FHR in beats per minute; left lower panel margin, uterine pressure in mm Hg; right lower panel margin, uterine pressure in kilopascal (kPa).
During hypoxemia, myocardial and cerebral blood flows increase to maintain oxygen delivery.35,36 However, in severe hypoxemia, blood flow cannot increase sufficiently to maintain oxygen delivery and a loss of FHR variability is observed.27 The absence of FHR variability in an anencephalic fetus indicates the influence of an intact central nervous system (CNS) in producing these patterns. In animal models, perfusion of the CNS with calcium results in depolarization of electroencephalographic (EEG) activity, which abolishes FHR variability.
Clinically, the presence of normal FHR variability predicts early neonatal health, as defined by an Apgar score of greater than 7 at 5 minutes.37,38 In a case series of monitored fetal deaths, no fetus had normal variability immediately before demise.27 The differential diagnosis of decreased variability includes fetal hypoxia, fetal sleep state, fetal neurologic abnormality, and decreased CNS activity that results from exposure to drugs such as opioids.
Accelerations
Accelerations are abrupt changes in the FHR above the baseline. Beyond 32 weeks’ gestation, an acceleration is defined by a peak of at least 15 bpm above the baseline, lasting at least 15 seconds. (Before 32 weeks’ gestation, a peak of 10 bpm above the baseline, lasting at least 10 seconds, is required.34) A prolonged acceleration extends for at least 2 minutes; however, when greater than 10 minutes in duration, it is considered a change in baseline.34 Antepartum FHR accelerations can occur in response to fetal movement and typically are a sign of fetal well-being; their presence indicates a reactive nonstress test. During the intrapartum period, the significance of FHR accelerations is less clear.28,38 Although the presence of accelerations generally precludes the existence of significant fetal metabolic acidosis, in some cases intrapartum accelerations may indicate a vulnerable umbilical cord.
Decelerations
Decelerations are typically classified as early, late, or variable. Early decelerations occur simultaneously with uterine contractions and usually are less than 20 bpm below baseline. The onset and offset of each deceleration coincides with the onset and offset of the uterine contraction (see Figure 8-3). In animal models, head compression can precipitate early decelerations.28 In humans, early decelerations are believed to result from reflex vagal activity secondary to mild hypoxia. Early decelerations are not ominous.
Late decelerations begin 10 to 30 seconds after the beginning of uterine contractions and end 10 to 30 seconds after the end of uterine contractions. Late decelerations are smooth and repetitive (i.e., they occur with each uterine contraction). Animal studies suggest that late decelerations represent a response to hypoxemia. The delayed onset of the deceleration reflects the time needed for the chemoreceptors to detect decreased oxygen tension and mediate the change in FHR by means of the vagus nerve.28,39 Late decelerations may also result from decompensation of the myocardial circulation and myocardial failure. Unfortunately, clinical and animal studies suggest that late decelerations may be an oversensitive indication of fetal asphyxia.28 However, the combination of late decelerations and decreased or absent FHR variability is an accurate, ominous signal of fetal compromise.29,40,41
Variable decelerations vary in depth, shape, and duration. They often are abrupt in onset and offset. Variable decelerations result from baroreceptor- or chemoreceptor-mediated vagal activity. Experimental models and clinical studies suggest that umbilical cord occlusion, either partial or complete, results in variable decelerations. During the second stage of labor, variable decelerations may result from compression of the fetal head. In this situation, dural stimulation leads to increased vagal discharge.42 The healthy fetus can typically tolerate mild to moderate variable decelerations (not below 80 bpm) without decompensation. With prolonged, severe variable decelerations (< 60 bpm) or persistent fetal bradycardia, it is difficult for the fetus to maintain cardiac output and umbilical blood flow.42
Sinusoidal and saltatory patterns are two unusual FHR tracing results that may indicate fetal compromise. The sinusoidal FHR pattern is a regular, smooth, wavelike pattern that may signal fetal anemia.27 Occasionally, maternal administration of an opioid can lead to a sinusoidal FHR pattern. The saltatory pattern consists of excessive alterations in variability (> 25 bpm) and may signal the occurrence of acute fetal hypoxia; there is a weak association between this pattern and low Apgar scores.27
Limitations of Electronic Fetal Heart Rate Monitoring
Despite laboratory and clinical data suggesting that FHR monitoring accurately reflects fetal health, controversy exists regarding the ability of this assessment tool to improve fetal and neonatal outcomes. First described more than 40 years ago, the use of continuous electronic FHR monitoring increased dramatically to encompass 45% and 85% of the monitored deliveries by 1980 and 2002, respectively.32 Retrospective reports of continuous FHR monitoring associate its use with a lower incidence of intrauterine fetal demise, neonatal seizures, and neonatal death.43–45 By contrast, the only consistent finding from multiple case-control studies and more than a dozen prospective, randomized trials of electronic FHR monitoring (with control arms that employed intermittent FHR auscultation46–48) is an increased rate of operative delivery. In a meta-analysis of these trials, which included more than 50,000 women from several continents, the incidence of 1-minute Apgar scores less than 4 and neonatal seizures was decreased with the use of continuous FHR monitoring.46–49 These results appear to suggest a correlation between abnormal FHR tracings and fetal acidemia.41,50 An evaluation of the 2004 United States birth cohort data suggested that the use of electronic FHR monitoring was associated with a significant decrease in early neonatal and infant mortality, a decreased risk for 5-minute APGAR scores less than 4 in low-risk pregnancies, and a lower rate of neonatal seizures in high-risk pregnancies.51
It remains unclear why prospective studies have not confirmed greater benefit of the use of continuous electronic FHR monitoring during labor; the intensity of intrapartum assessment and care may be partially responsible. In prospective trials, women randomly assigned to receive intermittent FHR auscultation were monitored by dedicated nursing staff who provided intensive intrapartum care. By contrast, the historical cohort studies compared patients who received continuous electronic FHR monitoring and intensive intrapartum care with patients who had intermittent FHR auscultation with nonintensive nursing care. There are no published studies that randomly assigned a group of patients to receive no FHR monitoring; however, the continued high rate of intrapartum stillbirth in unmonitored births in the developing world suggests that FHR assessment may be beneficial.
Consistent with the findings of the prospective trials, the ACOG endorses the use of either intermittent auscultation or continuous electronic FHR monitoring during labor. In high-risk patients, the ACOG guidelines recommend that the obstetrician or nurse review the electronic FHR tracing every 15 minutes during the first stage of labor and every 5 minutes during the second stage. For low-risk patients, the intervals may be lengthened to 30 minutes for the first stage and 15 minutes for the second stage.52 The optimal interval for intermittent FHR monitoring has not been studied, but the intervals suggested within the ACOG guidelines have some indirect support.53 Adherence to these standards for intermittent auscultation may be difficult to achieve in the clinical setting; in one study, only 3% of parturients met these standards.54
Several hypotheses to account for the apparent failure of intrapartum FHR monitoring to reduce the incidence of cerebral palsy have been proposed and include (1) a large proportion of the asphyxial damage begins before the onset of labor; (2) catastrophic events (e.g., cord prolapse, placental abruption, uterine rupture) may not allow sufficient time for intervention before neurologic damage occurs; (3) a larger proportion of very low-birth-weight infants survive and thus contribute to the numbers with cerebral palsy; (4) infection is associated with abnormal FHR patterns and the subsequent development of cerebral palsy, and it is unclear that early intervention offers any benefit in such cases; and (5) the amount of asphyxia required to cause permanent neurologic damage approximates the amount that causes fetal death, leaving a narrow window for intervention.55 The number of patients in whom cerebral palsy develops from intrapartum asphyxia is probably quite small.55
Limitations of FHR monitoring include a poor positive predictive value in distinguishing between abnormal FHR tracings and abnormal outcomes. Because of this imprecision, the ACOG recommended that abnormal FHR tracings be described with the term nonreassuring fetal status rather than fetal distress or birth asphyxia.56 In one population-based study of California children with cerebral palsy, FHR tracings were retrospectively reviewed and compared with those of neurologically normal children (i.e., control subjects). A markedly higher incidence of tracings with late decelerations and decreased variability was found in children with cerebral palsy than in the control subjects. However, of the estimated 10,791 monitored infants weighing 2500 g or more who had these FHR abnormalities, only 21 (0.19%) had cerebral palsy, representing a false-positive rate of 99.8%.57 Later case-control studies have yielded similar results.16,58 A 2006 meta-analysis of 12 trials including 37,000 women suggested that electronic FHR monitoring has resulted in a decrease in the occurrence of seizures but no change in the incidence of neonatal mortality or cerebral palsy.49 The authors suggested that electronic FHR monitoring resulted in one cesarean delivery for every 58 women monitored and that 661 women would need to be monitored to prevent one neonatal seizure.49 Therefore, use of electronic FHR monitoring in combination with clinical and laboratory assessments has been proposed to enhance the prediction and perhaps the prevention of severe asphyxia, but with poor specificity.16
Further limitations of continuous FHR monitoring include (1) the poor intra-observer and inter-observer agreement despite the use of trained observers, (2) the required continual presence of a nurse or physician to assess the FHR tracing, (3) the inconvenience for the patient (e.g., confinement to bed and the application of monitor belts or a scalp electrode), and (4) the need to archive the FHR tracings as legal documents.59–61
Despite little evidence for its efficacy, Parer and King62
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


