Initial Management of Metabolic Acidosis
DIAGNOSIS/INDICATION
Metabolic acidosis in the neonate can have several causes, including increased acid intake from an exogenous source, increased endogenous production of an acid such as seen in an inborn error of metabolism (IEM), inadequate excretion of acid by the kidneys or excessive loss of bicarbonate in urine or stool. Presence or absence of an anion gap (AG) can help to distinguish the underlying etiology. The AG can be calculated using the following equation: AG = ([Na+]) − ([Cl−] + [HCO3−]). A normal AG is typically less than 16 mEq/L.1 Common anions that result in an elevated AG include lactate and the ketone bodies β-hydroxybutyrate and acetoacetate, as well as the accumulation of the toxic organic acids typically found in individuals with IEMs.
Clinical Findings
Clues that increase the likelihood of identifying an IEM include a family history of consanguinity or history of a neonatal or sibling death. Occasionally, maternal history of acute fatty liver of pregnancy may be solicited.
Infants with IEMs are usually normal at birth. They develop nonspecific findings similar to those for sepsis, such as poor feeding, vomiting, lethargy, hypotonia, hypothermia, seizures, and coma. Infants will try to correct metabolic acidosis by a reflex respiratory alkalosis using hyperventilation and Kussmaul respirations. More severe uncompensated acidosis can decrease peripheral vascular resistance and cardiac ventricular function, leading to hypotension, pulmonary edema, and tissue hypoxia, which will further complicate the picture by increasing lactate production because of hypoxia and poor perfusion.
Confirmatory Tests
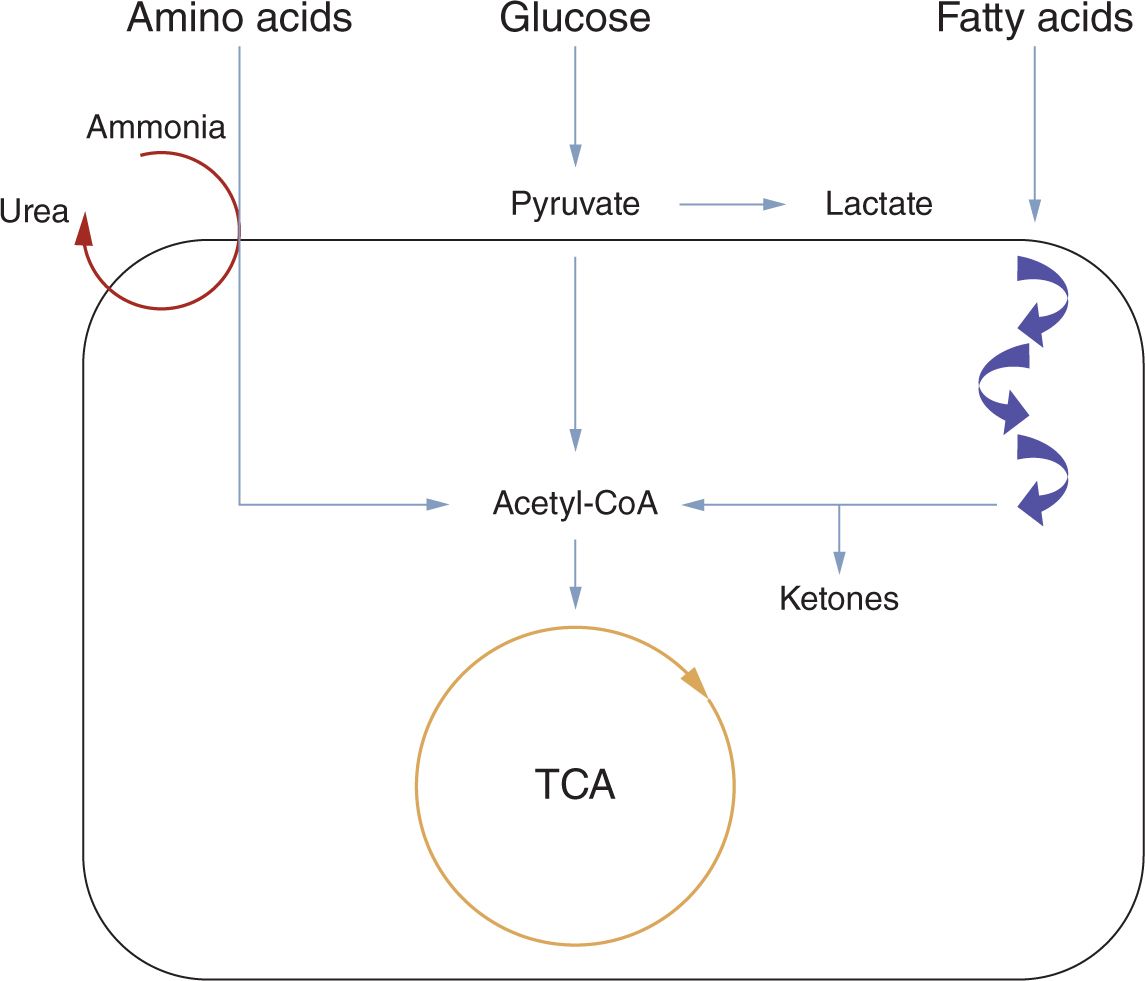
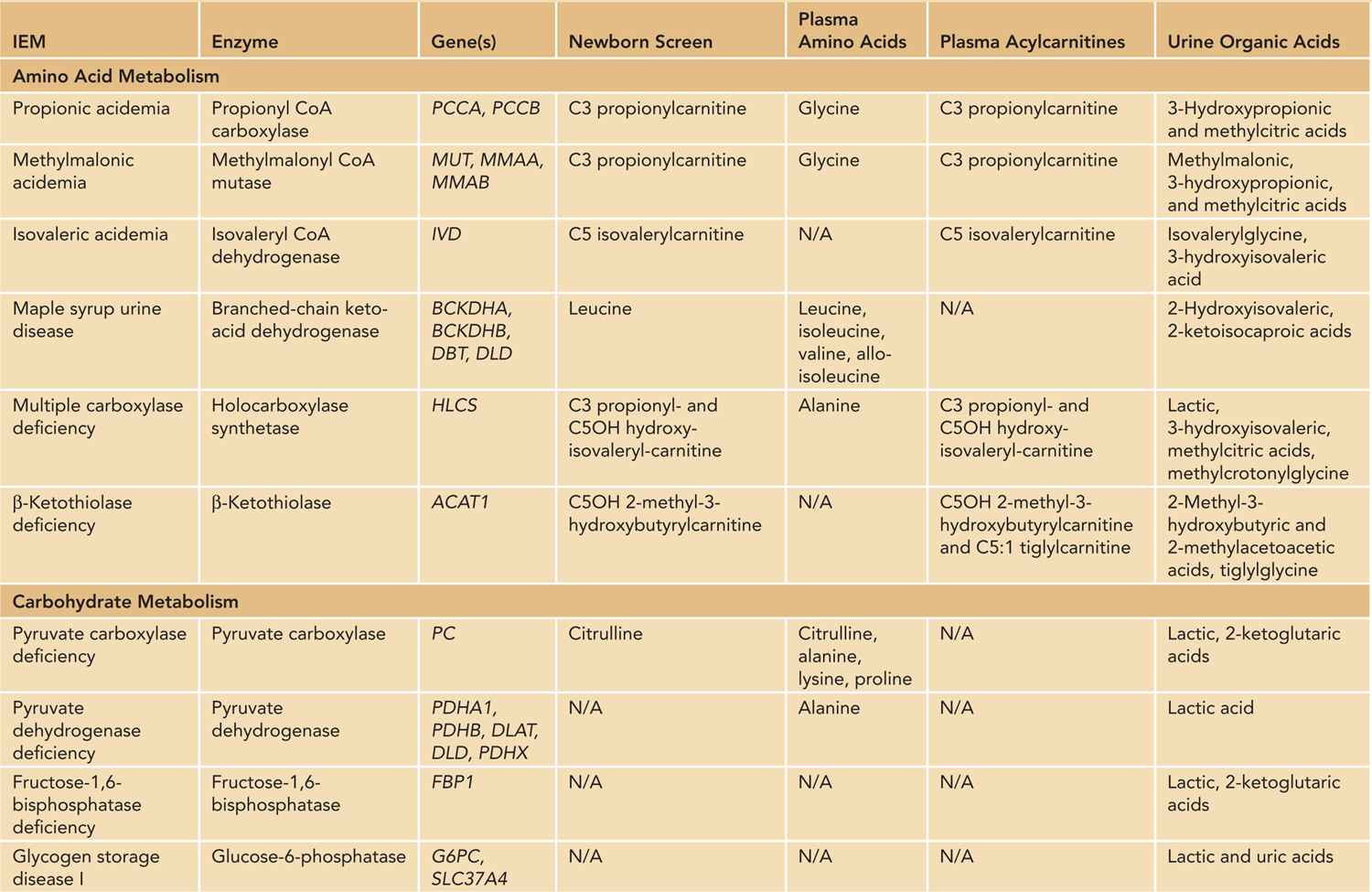
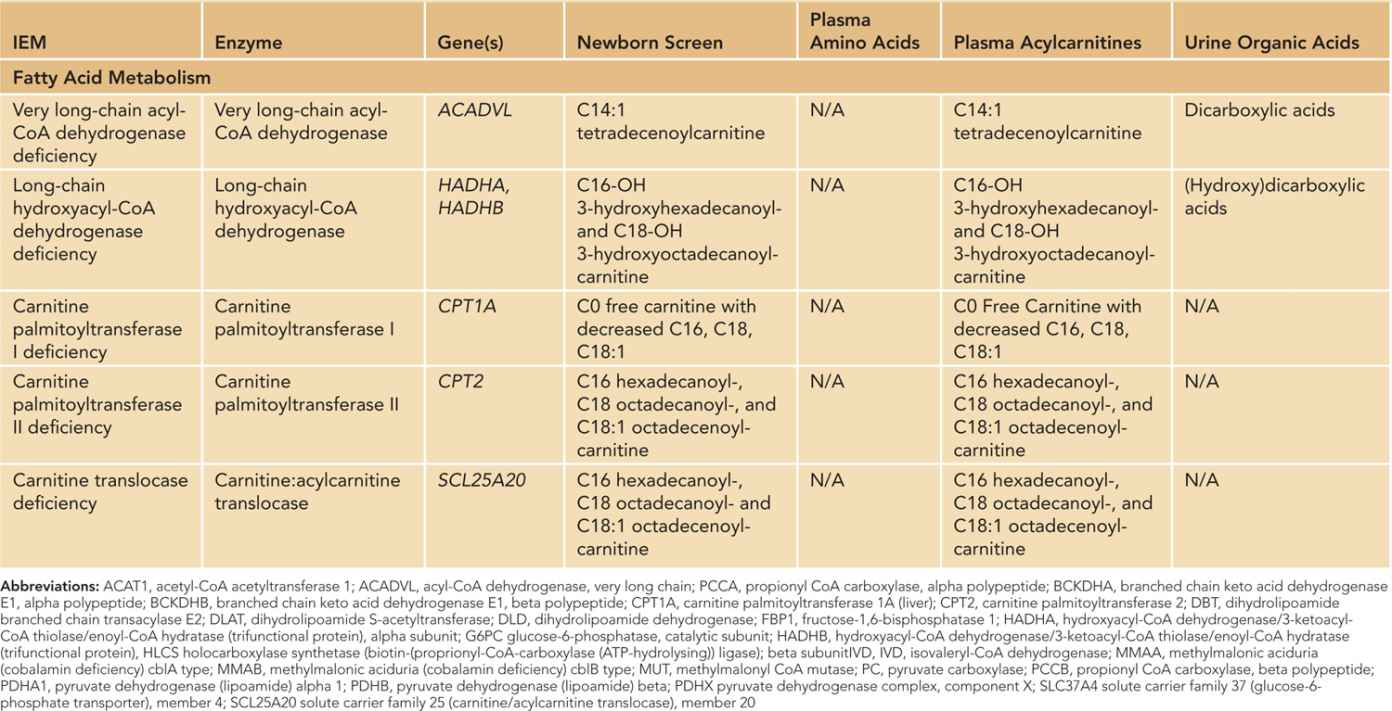
The IEMs are enzyme deficiencies that result from amino acid, carbohydrate, or fatty acid metabolism (Figure 107-1). Most of these disorders can be diagnosed by routine metabolic testing (Table 107-1), including plasma amino acid, plasma acylcarnitine profile, and urine organic acid analyses. Please see Table 107-2 for details about IEMs and the specific abnormalities detected by laboratory evaluations.
FIGURE 107-1 Basic pathways. Amino acids, carbohydrates, and fatty acids all undergo multiple processes to be converted into energy. The final common pathway is the formation of acetyl-CoA (coenzyme A), which can enter the tricarboxylic acid (TCA) cycle. NADH (nicotinamide adenine dinucleotide, reduced form) generated by the TCA cycle can be fed to the electron transport chain to generate ATP (adenosine triphosphate), the main energy source for numerous cellular functions. Defects in amino acid, carbohydrate, or fatty acid metabolism will lead to decreased energy production.
Table 107-1 Laboratory Tests for Any Patient With a Known or Suspected Inborn Error of Metabolism
Venous/arterial blood gas
Glucose
Lactate
Ammonia
Comprehensive metabolic panel
Anion gap ([Na+] − ([Cl−] + [HCO3−]))
Complete blood cell count
Blood culture
Plasma amino acids
Plasma acylcarnitine profile
Urinalysis to assess ketones
Urine organic acids
Urine culture
Table 107-2 Summary of Inborn Errors of Metabolism (IEMs) and Their Findings
TREATMENT
Treatment of the metabolic acidosis depends on the cause. Although sodium bicarbonate can be given to improve the pH, it will not treat the underlying cause of the acidosis, especially if the underlying etiology is an IEM. Episodes of decompensation can be life threatening, so emergent and aggressive treatment is required. Treatment typically includes reversing catabolism by any means possible, often with extra calories provided from dextrose and lipids when allowed and restriction of the toxic metabolite, such as protein in the organic acidemias. Please see Table 107-3 for the acute management protocol and Table 107-4 for discharge planning.
Table 107-3 Acute Management Protocol