Inguinal Lymphadenectomy
Robert E. Bristow
INTRODUCTION
Inguinal lymphadenectomy is primarily indicated for the diagnostic assessment and/or treatment (resection of gross adenopathy) of squamous carcinoma of the vulva. Inguinal lymphadenectomy is an essential component of therapy for almost all patients undergoing primary surgery for vulvar cancer of squamous histology. With the exception of patients with low-risk Stage IA disease (lateralized lesion, tumor size <2 cm, maximum depth of invasion ≤1 mm, absence of lymphovascular space invasion, clinically negative groins), either unilateral or bilateral inguinal lymphadenectomy is indicated depending on the size, location, and laterality of the primary lesion. Recent data indicate that sentinel lymph node biopsy may be a safe and accurate alternative to inguinal lymphadenectomy for patients with Stage I and II squamous tumors. Inguinal lymphadenectomy is also indicated for patients with invasive adenocarcinoma of the vulva and vulvar melanoma as well as patients with invasive cancer of the lower one-third of the vagina. Rarely, inguinal lymphadenectomy is performed for the purpose of resecting gross lymph node metastases and surrounding subclinical nodal disease as part of the therapeutic approach to selected patients with advanced ovarian or endometrial cancers.
The superficial inguinal lymph nodes are almost always the primary node basin for cancers of the vulva and usually include 8 to 10 lymph nodes. The deep femoral nodes usually consist of three to five nodes, are located beneath the cribriform fascia, and are generally thought to represent the secondary node basin before drainage into the deep pelvic nodes occurs. The most proximal deep femoral node, Cloquet’s node, is located in the femoral canal just beneath the inguinal ligament. Lymphatic drainage of the vulva follows a systematic flow pattern from the posterior vulva to the anterior region on either side, always running medial to the labiocrural fold. The mons pubis and anterior vulva contain drainage pathways to the contralateral groin (Figure 16.1). For lateralized lesions (≥2 cm from the midline) in the mid- to posterior-vulva, a unilateral inguinal lymphadenectomy is sufficient unless there are grossly suspicious or pathologically positive nodes in the ipsilateral groin. For lesions located <2 cm from the midline, lesions on the anterior vulva, and patients with grossly or pathologically positive ipsilateral groin nodes, a bilateral inguinal lymphadenectomy is the procedure of choice. The risk of pelvic node metastasis increases directly with the size and number of inguinal nodes involved by disease. Approximately 25% to 30% of patients with gross inguinal adenopathy and/or pathologic confirmation of disease in less than or equal to three nodes will have positive pelvic nodes. When more than four groin nodes are positive for disease, the risk of pelvic node spread increases to 60%.
PREOPERATIVE CONSIDERATIONS
Most patients undergoing inguinal lymphadenectomy will simultaneously require a radical vulvectomy or wide radical excision of the vulva and should be prepared
accordingly. All patients should undergo a comprehensive history and physical examination focusing on those areas that may indicate a reduced capacity to tolerate surgery. Routine laboratory testing should include a complete blood count, serum electrolytes, age-appropriate health screening studies, and electrocardiogram for women aged 50 years and older. Preoperative computed tomography imaging of the abdomen and pelvis is advisable if the groin nodes are clinically suspicious or the primary lesion is large (>4 cm). A chest radiograph should be obtained, or alternatively computed tomography scanning can be extended to include the chest.
accordingly. All patients should undergo a comprehensive history and physical examination focusing on those areas that may indicate a reduced capacity to tolerate surgery. Routine laboratory testing should include a complete blood count, serum electrolytes, age-appropriate health screening studies, and electrocardiogram for women aged 50 years and older. Preoperative computed tomography imaging of the abdomen and pelvis is advisable if the groin nodes are clinically suspicious or the primary lesion is large (>4 cm). A chest radiograph should be obtained, or alternatively computed tomography scanning can be extended to include the chest.
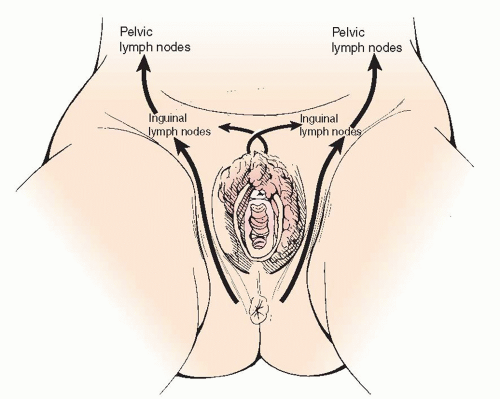 FIGURE 16.1 Inguinal lymphadenectomy: Lpsilateral and contralateral vulvar lymphatic drainage pathways. |
Prophylactic antibiotics (Cephazolin 1 g, Cefotetan 1 to 2 g, or Clindamycin 800 mg) should be administered 30 minutes prior to incision, and thromboembolic prophylaxis (e.g., pneumatic compression devices and subcutaneous heparin) should be initiated prior to surgery. The instrumentation required includes a basic vaginal surgery set and Allen Universal Stirrups (Allen Medical Systems, Cleveland, OH). Enemas should be administered the evening before surgery. Preoperative mechanical bowel preparation is not necessary unless dictated by the extent of resection of the primary lesion.
SURGICAL TECHNIQUE
Either general or regional anesthesia is acceptable. The patient should be positioned in dorsal lithotomy position using Allen-type stirrups with the thighs externally rotated and flexed at 15° or less to optimize exposure to the groin. A Foley catheter is placed as dictated by the operation for the primary lesion.
An 8- to 10-cm incision is drawn with a marking pen in the groin crease, 1 to 2 cm below the inguinal ligament, midway between the anterior superior iliac spine and the ipsilateral pubic tubercle (Figure 16.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


