Infant of HIV-Positive Mother
INTRODUCTION
Perinatal transmission rates in the United States are at historic lows (<2%) because of the availability of effective interventions to prevent perinatal human immunodeficiency virus (HIV) transmission.1 However, transmission does occur in a small number of infants, primarily because of missed prevention opportunities.2,3 The neonatologist plays a vital role in the prevention of perinatal HIV transmission in early identification of HIV-exposed newborns born to infected mothers who were not tested for HIV during pregnancy and in administering antiretroviral (ARV) prophylaxis to HIV-exposed infants as early as possible after birth.4,5 The primary care physician, in conjunction with a pediatric infectious disease specialist, must ensure appropriate follow-up to confirm or exclude the diagnosis of HIV infection in early infancy and provide ongoing counseling, support, and anticipatory guidance6 (Table 117-1). A comprehensive review of recommendations for evaluation and treatment of the HIV-exposed infant has been published by the American Academy of Pediatrics (AAP) and other experts.4,5,7,8 This chapter discusses the clinical evaluation, laboratory testing, and treatment of HIV-exposed infants, incorporating the recently updated Public Health Service guidelines with a focus on prevention of perinatal HIV transmission.5,6
Table 117-1 Clinical Care of Infants Exposed to Human Immunodeficiency Virus (HIV)
History and physical examination
Infant ARV prophylaxis
Avoidance of breast-feeding
• Infant formula
Determination of HIV status
• Virologic testing at 14–21 days, 1–2 months, and 4–6 months of age
• HIV antibody testing at 12–18 months (for infants in whom serial virologic tests are negative in early infancy) to document HIV seroreversion and definitively exclude infectiona
PCP prophylaxis
• TMP-SMX from 6 weeks and continued until HIV infection is presumptively or definitively excluded
Psychosocial support to mother and other caregivers
Comprehensive well-baby care
• Immunizations
• Growth and development monitoring
• Anticipatory guidance
Abbreviations: ARV, antiretroviral prophylaxis; PCP, Pneumocystis jiroveci pneumonia; TMP-SMX, trimethoprim-sulfamethoxazole.
aExpert recommendation. from references 5 and 14.
DIAGNOSIS/INDICATION
Universal prenatal HIV testing is the gateway to access effective antepartum, intrapartum, and postpartum interventions to prevent perinatal HIV transmission. All pregnant women must be routinely tested for HIV (“opt-out” approach) regardless of potential risk factors.9 Repeat testing during the third trimester of pregnancy is recommended for certain high-risk populations to identify new infections.9 HIV-negative women should receive counseling to maintain HIV-negative status during pregnancy and thereafter. In contrast, women with acute or recent HIV infection must be linked to care and receive a potent combination ARV drug regimen as soon as possible, with the goal of achieving viral load to undetectable levels and preventing perinatal HIV transmission.5 Scheduled cesarean delivery at 38 weeks’ gestation is recommended for HIV-positive women who have received ARV agents but have viral load greater than 1000 copies/mL near delivery.5 Care of the HIV-exposed infant must then focus on reducing the risk of transmission with ARV prophylaxis.
If maternal HIV infection status is unknown at the time of delivery or repeat testing during the third trimester has not been done in certain high-risk women as recommended, rapid HIV testing of the mother or infant is recommended as soon as possible after delivery with immediate initiation of ARV prophylaxis if the rapid test is positive.5 Western blot testing must be done as soon as possible to confirm positive rapid HIV antibody test on the mother or infant, but infant ARV prophylaxis must not be delayed while waiting for the confirmatory results. ARV prophylaxis can be discontinued if the confirmatory test result is negative.5
Clinical Findings
History
The initial assessment of the HIV-exposed infant begins in the delivery room. Prenatal history is critical in the routine evaluation and management of HIV-exposed infants. Identification of perinatal HIV exposure is the first step involved in the delivery of optimal care to the HIV-exposed infant.6 In most cases, the diagnosis of maternal HIV infection would have been established during the antenatal period. Medical and obstetrical history should be reviewed to determine if the risk of perinatal HIV transmission is high or low depending on whether the mother received effective interventions. Details about maternal HIV diagnosis (viral load, CD4 T-lymphocyte cell count, genotypic drug resistance testing); ARV drug regimen (timing of initiation and compliance); and maternal clinical status must be elicited.6,8 Maternal history should include history of sexually transmitted infections (such as syphilis, hepatitis B, or herpes simplex virus) or coinfections such as tuberculosis (TB), toxoplasmosis, or hepatitis C. Infants exposed to 1 or several of these pathogens should undergo further evaluation. In addition, history should include obstetric details (including duration of ruptured membranes, mode of delivery), use of invasive intrapartum monitoring, birth weight, and gestational age.6
Physical Examination
Infants with perinatally acquired HIV infection are often asymptomatic, and physical examination is usually normal in the neonatal period.10 The common features of HIV infection in early infancy are lymphadenopathy, hepatomegaly, and splenomegaly, often noted at around 3 months of age.10 Other commonly encountered findings in the first year of life include failure to thrive and neurodevelopmental delay.10,11 HIV-exposed infants must be closely monitored for signs and symptoms of early HIV infection before definitive virologic tests become available.6
Baseline Tests
A complete blood cell count (CBC) with differential should be obtained on HIV-exposed infants before initiating ARV prophylaxis.5 Some experts recommend virologic testing (HIV DNA or RNA polymerase chain reaction [PCR] assay) at birth for diagnosis of intrauterine HIV infection, especially in HIV-infected women who have suboptimal viral suppression during pregnancy or near delivery or there is a concern about infant follow-up.5
TREATMENT
Neonatal ARV Prophylaxis
All HIV-exposed infants must receive ARV prophylaxis as soon as possible after birth, preferably at 6–12 hours of life, to reduce the risk of perinatal HIV transmission (Table 117-2).5 When the mother has received combination ARV therapy (ART) during pregnancy, neonatal zidovudine (ZDV) at gestational age-appropriate dosing for 6 weeks is the recommended ARV prophylaxis regimen of choice.
Table 117-2 Antiretroviral Interventions to Prevent Perinatal Human Immunodeficiency Virus (HIV) Transmissiona
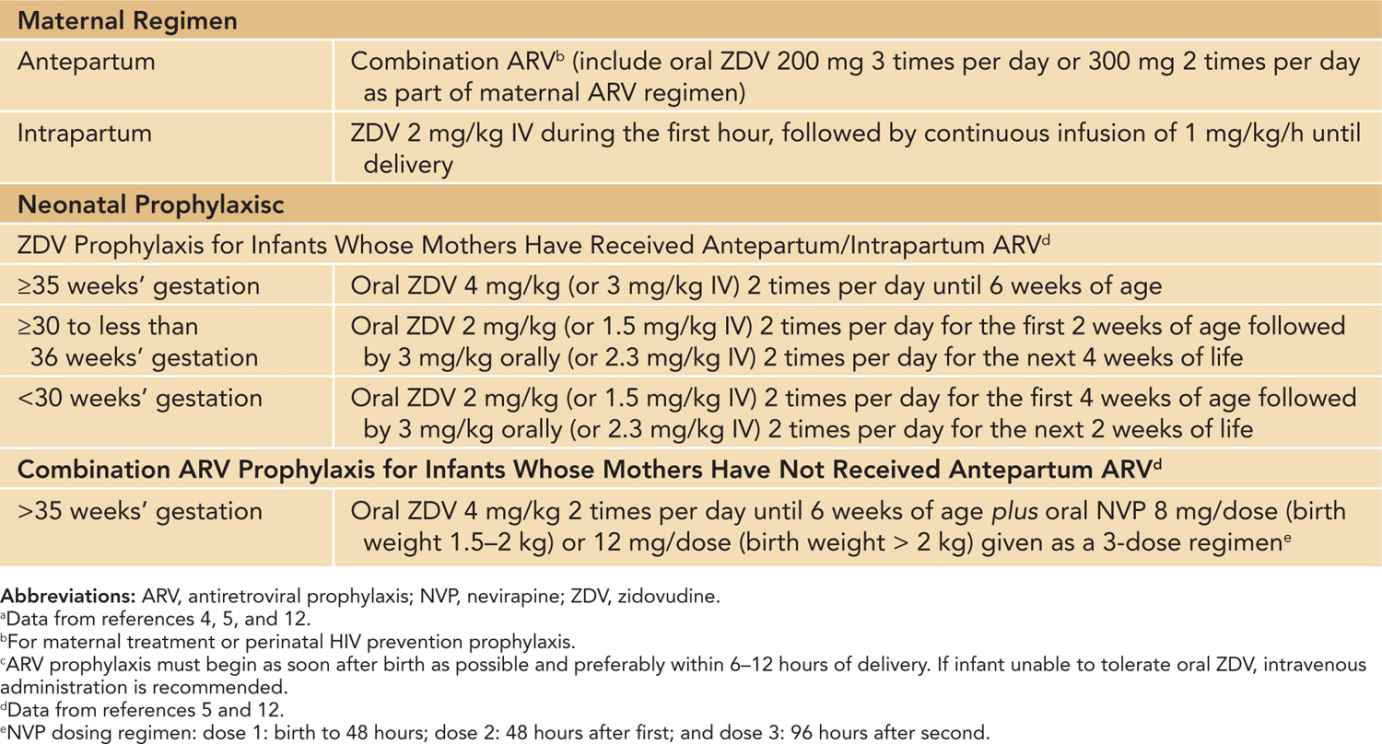
When the mother has not received antepartum ARV during pregnancy, combination ARV prophylaxis, including ZDV for 6 weeks plus 3 doses of nevirapine (NVP) during the first week of life (birth, 48 hours, and 96 hours of life), is recommended for HIV-exposed infant (Tables 117-2 and 117-3).5,12 In these scenarios, a pediatric HIV specialist should be consulted and mothers should be counseled regarding the potential benefits and risks of combination ARV prophylaxis. In premature infants, only ZDV and NVP are recommended for ARV prophylaxis because data on pharmacokinetic, dosing, and safety of alternative ARV drugs are lacking. Infant ARV prophylaxis initiated after 48 hours of birth is not effective.13
Table 117-3 Indications for Combination Antiretroviral (ARV) Prophylaxis to Infants Exposed to Human Immunodefiency Virusa



