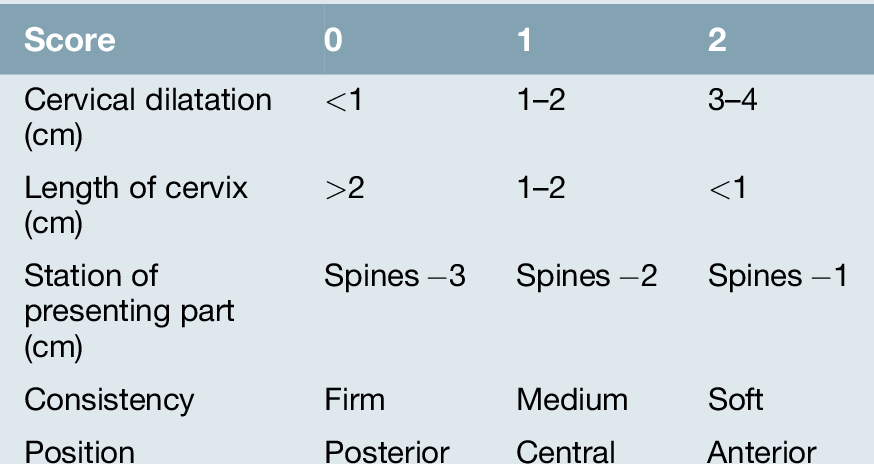
42 Induction of labour is indicated when the risks of continuing the pregnancy are felt to be greater than the risks of ending the pregnancy. Induction is usually carried out in the interest of fetal well-being and less commonly, for maternal reasons. The decision is often difficult, particularly at pre-term gestations, and many factors, including the availability of neonatal facilities, need to be considered. Labour should not be induced until there has been a careful discussion with the mother about the pros and cons of the induction. It should be noted that ‘induction’ is different from ‘augmentation’. Induction refers to the process of starting labour and can only be applied to a mother who is not already in labour. Augmentation describes the process of accelerating labour after it has already started. The decision to induce labour depends on the balance between the risks of continuing fetal surveillance and the risks of induction and pre-term delivery. Induction risks are largely related to the use of ‘oxytocics’, the preparations that are used to stimulate uterine activity. The side-effect of greatest concern is that of uterine hyperstimulation, which carries the risk of fetal compromise. The process of induction may also be associated with increased obstetric intervention, particularly if carried out before 41 + weeks’ gestation. Finally, induction may be unsuccessful and the obstetrician may feel compelled to undertake a caesarean section that would not otherwise have been necessary. Before induction, the gestation should again be confirmed, the presentation checked and any contraindications (e.g. placenta praevia) excluded. It is important to note that real caution is required in those who have had a previous caesarean section or previous uterine surgery, as induction carries an increased risk of uterine scar rupture, and many clinicians would consider these as contraindications, unless the cervix was very favourable. Repeat elective caesarean may be a safer option for mother and baby in this scenario. In addition, grand multiparity and a history of previous precipitate labour also carry increased risks of hyperstimulation. The decision about which technique is the most appropriate depends on the cervix, as assessed by the Bishop’s scoring system (Table 42.1 and Box 42.1):
Induction of labour
Introduction
Fetal indications
![]() Post-dates – usually between 41 and 42 weeks’ gestation
Post-dates – usually between 41 and 42 weeks’ gestation
![]() Fetal growth restriction with risk of fetal compromise (based on estimated growth and fetal monitoring. There may be associated pre-eclampsia
Fetal growth restriction with risk of fetal compromise (based on estimated growth and fetal monitoring. There may be associated pre-eclampsia
![]() Certain diabetic pregnancies
Certain diabetic pregnancies
![]() Deteriorating haemolytic disease of the newborn (rare).
Deteriorating haemolytic disease of the newborn (rare).
Maternal indications
![]() Pre-eclampsia. This is a condition in which both maternal and fetal interests are relevant. While it may, for example, be appropriate to induce for mild pre-eclampsia at term, the pre-eclampsia would need to be severe in a markedly preterm infant
Pre-eclampsia. This is a condition in which both maternal and fetal interests are relevant. While it may, for example, be appropriate to induce for mild pre-eclampsia at term, the pre-eclampsia would need to be severe in a markedly preterm infant
![]() Deteriorating medical conditions (cardiac or renal disease, severe systemic lupus erythematosus, SLE)
Deteriorating medical conditions (cardiac or renal disease, severe systemic lupus erythematosus, SLE)
![]() Antepartum haemorrhage.
Antepartum haemorrhage.
Obgyn Key
Fastest Obstetric, Gynecology and Pediatric Insight Engine