Fig. 68.1
a and b Clinical photographs showing a child with hypospadias. Note the dorsal hood of foreskin and a clinical photograph showing hypospadias. Note the ectopic urethral opening and the incomplete prepuce ventrally

Fig. 68.2
A clinical photograph showing hypospadias. Note the ectopic proximally located urethral opening as well as the widened glanular groove
A dorsal hood of foreskin.
An incomplete prepuce ventrally.
A glanular groove.
A proximally suited ectopic position.
Chordee (ventral shortening and curvature) is more likely with more proximal hypospadias.
Rarely, the foreskin may be complete and the hypospadias is discovered at the time of circumcision (Figs. 68.2, 68.3, and 68.4).

Fig. 68.3
A clinical photograph showing a normal intact prepuce with no evidence of hypospadias

Fig. 68.4
A clinical photograph of the same patient in Fig. 68.3 showing hypospadias after retraction of the prepuce (Megameatus intact prepuce variant)
The treatment for hypospadias is surgical repair.
More than 300 different types of repairs have been described in the medical literature.
Hypospadias is generally repaired for functional and cosmetic reasons.
The more proximal the position of the urethral meatus, the more likely the urinary stream is to be deflected downward.
This is exacerbated by the presence of chordee .
Fertility may be affected as the abnormal deflection of ejaculate may preclude effective insemination.
Chordee can be associated with painful erections.
There is potential psychological stress of having abnormal genitalia.
The final outcome of hypospadias repair improved markedly as a result of several factors:
Modern anesthetic techniques
Fine instruments and better surgical techniques
Better sutures and dressing materials
Antibiotics
Embryology
Hypospadias is a congenital defect that is thought to occur during urethral development, from 8 to 20 weeks’ gestation.
Testosterone is the main factor responsible for masculinization of the external genitalias.
As the phallus grows, there is an open urethral groove which extends from the base to the level of the corona.
The urethral folds than fuse in the midline forming a tubularized posterior and middle urethra.
The anterior urethra develops in a proximal direction, with an ectodermal core forming at the tip of the glans penis, which canalizes to join with the more proximal urethra at the level of the corona.
The higher incidence of subcoronal hypospadias supports the vulnerable final step in this theory of development .
Another theory suggests that the urethral folds fuse in the midline to form a seam of epithelium, which is then transformed into mesenchyme and subsequently canalizes by apoptosis or programmed cell resorption. This is also the case for the anterior urethra where the endoderm differentiates to ectoderm with subsequent canalization by apoptosis.
The prepuce normally forms as a ridge of skin from the corona that grows circumferentially, fusing with the glans.
Failure of fusion of the urethral folds in hypospadias impedes this process, and a dorsal hooded prepuce results.
On rare occasions, a glanular cleft with intact prepuce may occur, which is termed the megameatus intact prepuce variant .
Chordee is thought to result from the abnormal attenuated ventral urethra and associated tissues as well as the abortive spongiosal tissue and fascia distal to the urethral meatus which forms a tethering fibrous band .
Classification
In the past hypospadias was classified as follows:
First-degree hypospadias (50–75 %): The urethral meatus opens on the underside of the glans penis.
Second-degree hypospadias (15–20 %): The urethral meatus opens on the shaft of the penis.
Third-degree hypospadias (20–30 %): The urethral meatus opens on the perineum.
The more severe degrees of hypospadias are more likely to be associated with chordee .
The recent classification of hypospadias was proposed by Barcat and modified by Duckett which is based on the site of the abnormal urethral meatus after correction of any associated chordee.
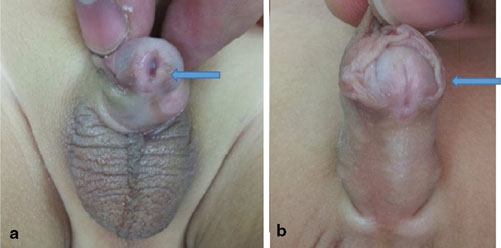
Fig. 68.5
A clinical photograph showing glanular hypospadias (a) and a photograph showing coronal hypospadias (b)

Fig. 68.6
A clinical photograph showing subcoronal hypospadias
◦ Glanular.
◦ Coronal.
◦ Subcoronal. The subcoronal position is the most common type.
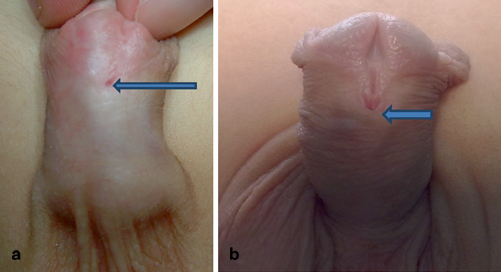
Fig. 68.7
a A clinical photograph showing distal penile hypospadias. Note the shallow glanular groove. b Clinical photograph showing a distal penile hypospadias. Note the deep glanular groove
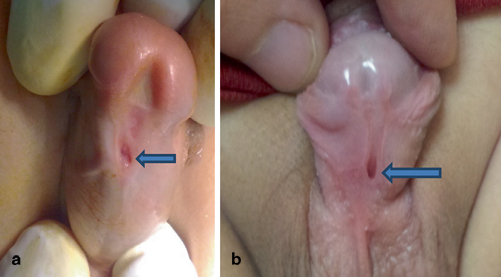
Fig. 68.8
Clinical photographs showing midpenile hypospadias (a) and proximal penile hypospadias (b)
◦ Distal penile
◦ Midshaft (Midpenile)
◦ Proximal penile
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


