KEY POINTS
Background
• Hypertensive disorders are the most common medical complication of pregnancy, occurring in approximately 7% to 10% of all pregnancies.
• Hypertensive disorders are associated with significant maternal and perinatal mortality and have a wide spectrum of presentation, ranging from minimal elevation of blood pressure to severe hypertension with multiple organ dysfunction.
• Preeclampsia is a syndrome that only occurs during pregnancy and is defined by hypertension and end-organ manifestations such as proteinuria, thrombocytopenia, and hepatic or cerebral manifestations.
Definitions for Hypertensive Disorder of Pregnancy
• Gestational hypertension
• The National High Blood Pressure Education Program Working Group has recommended that the term “gestational hypertension” replace the term “pregnancy-induced hypertension” to describe cases in which elevated blood pressure without proteinuria develops in a woman after 20 weeks of gestation and blood pressure levels return to normal postpartum (1).
• According to the criteria established in pregnant women by the Hypertension in Pregnancy Task Force sponsored by the ACOG, gestational hypertension is defined as a persistent systolic blood pressure level of 140 mm Hg or greater or a diastolic blood pressure level of 90 mm Hg or greater that occurs on two occasions 4 hours apart after 20 weeks of gestation in a woman with previously normal blood pressure (2).
• Preeclampsia
• A syndrome of gestational hypertension plus end-organ manifestations including proteinuria with proteinuria defined as urinary excretion of 0.3 g protein or more in a 24-hour urine specimen or a protein/creatinine ratio ≥0.3 mg/dL. In the absence of proteinuria, new-onset hypertension with thrombocytopenia (less than 100,000 platelets/mL) or renal insufficiency (serum creatinine concentration greater than 1.1 mg/dL) or impaired liver functions (transaminases twice the upper limits of normal concentration) constitute diagnostic criteria of preeclampsia (2).
• The previous definition of preeclampsia as hypertension of more than 30 mm Hg systolic or 15 mm Hg diastolic above the patient’s baseline blood pressure is no longer used.
• Eclampsia
• The development of convulsions or coma in patients with signs and symptoms of preeclampsia in the absence of other causes of convulsions
• Chronic hypertension
• Patients with a persistent elevation of blood pressure to at least 140/90 mm Hg on two occasions before 20 weeks’ gestation, and patients with hypertension that persists for more than 6 weeks postpartum
• Superimposed preeclampsia or eclampsia
• The development of either preeclampsia or eclampsia in patients with previously diagnosed chronic hypertension
PREECLAMPSIA
Background
Definition
• Preeclampsia is a syndrome of gestational hypertension as defined above.
• There are only two types of preeclampsia: mild and severe.
Etiology
Preeclampsia is a disorder of unknown etiology that is peculiar to human pregnancy. Many theories regarding its etiology have been suggested, including
• Abnormal placentation
• Immunologic phenomena
• Coagulation abnormalities
• Abnormal cardiovascular adaptation
• Dietary factors
• Genetic factors
• Angiogenesis factors
• Vascular endothelial damage
• Abnormal prostaglandin metabolism
Epidemiology
• Preeclampsia is principally a disease of young, nulliparous women.
• The incidence of gestational hypertension is 6% to 17% for healthy nulliparous women and 2% to 4% for multiparous women.
• The incidence of mild preeclampsia is 2% to 7% in healthy nulliparous women and 14% in twin gestations.
• Seventy-five percent of patients with preeclampsia develop the disorder at ≥37 weeks of gestation.
Risk Factors
Although geographic and racial differences in incidence have been reported, several risk factors have been identified as predisposing to the development of preeclampsia:
• Nulliparity
• Multiple gestation
• Previous pregnancy with preeclampsia
• Family history of preeclampsia or eclampsia
• Preexisting hypertension or renal disease
• Pregestational diabetes
• Use of donor oocytes
• Nonimmune hydrops fetalis
• Molar pregnancy
• Obesity
Diagnosis
Clinical Manifestations
• Preeclampsia traditionally has been described as hypertension and proteinuria. It may, however, present as a spectrum of clinical signs and symptoms, alone or in combination, often making diagnosis difficult.
• Hypertension
 Abnormally elevated blood pressure is the traditional hallmark for the diagnosis of preeclampsia. The blood pressure criteria for gestational hypertension and preeclampsia are presented earlier in the chapter.
Abnormally elevated blood pressure is the traditional hallmark for the diagnosis of preeclampsia. The blood pressure criteria for gestational hypertension and preeclampsia are presented earlier in the chapter.
• Proteinuria
 Protein excretion in the urine increases in normal pregnancy from approximately 5 mg per 100 mL in the first and second trimesters to 15 mg per 100 mL in the third trimester.
Protein excretion in the urine increases in normal pregnancy from approximately 5 mg per 100 mL in the first and second trimesters to 15 mg per 100 mL in the third trimester.
 Significant proteinuria should be defined as greater than 300 mg per 24-hour urine sample or protein/creatinine ratio ≥0.3 mg/dL.
Significant proteinuria should be defined as greater than 300 mg per 24-hour urine sample or protein/creatinine ratio ≥0.3 mg/dL.
 When making a diagnosis of severe preeclampsia, the criterion of proteinuria of greater than 5 g excreted in a 24-hour urine has been discontinued (2).
When making a diagnosis of severe preeclampsia, the criterion of proteinuria of greater than 5 g excreted in a 24-hour urine has been discontinued (2).
• Early recognition of the development of preeclampsia can allow for more timely intervention to improve maternal and perinatal outcome. This reinforces the reason for frequent antenatal visits late in pregnancy to allow early detection of disease.
• Some preeclamptic pregnancies, particularly those with more severe disease, can be associated with reduced uteroplacental blood flow, which may be manifested as poor fetal growth. This can be the primary initial manifestation of preeclampsia and can be seen in both mild and severe forms of the disease.
Management
• Figure 11-1 shows a sample algorithm for the management of a normotensive patient who may be developing subtle signs and symptoms of preeclampsia.
• Once the diagnosis of preeclampsia has been made, definitive therapy in the form of delivery is the desired goal because it is the only cure for the disease.
• The ultimate goals of the therapy must always be first the safety of the mother and then the delivery of a mature newborn that will not require intensive and prolonged neonatal care.
• The decision between expectant management and immediate delivery usually depends on one or more of the following factors:
• Severity of the disease process
• Fetal condition
• Maternal condition
• Fetal gestational age
• Presence of labor or rupture of membranes
MILD PREECLAMPSIA
Evaluation
• At the time of diagnosis, all patients with preeclampsia should be evaluated regarding maternal/fetal condition.
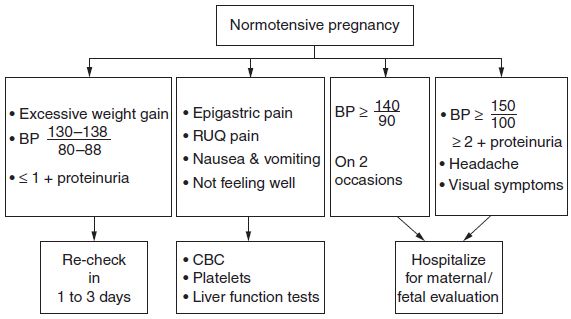
Figure 11-1. A sample algorithm for the management of a normotensive patient who may be developing subtle signs of preeclampsia.
Maternal Evaluation
History
Markers for possible severe preeclampsia:
• Persistent occipital or frontal headaches
• Visual disturbances
• Right upper quadrant abdominal or epigastric pain
Physical Evaluation
• Blood pressure assessment at diagnosis, then twice weekly by the health care provider.
• Urine protein assessment at diagnosis. If significant proteinuria is identified, subsequent proteinuria evaluation is not necessary as the amount or change in the amount of proteinuria will not influence the need for delivery (2).
• Weight daily.
Laboratory Evaluation
• Hematocrit and platelet count once per week
• Liver function tests once per week
• Twenty-four–hour urine collection at diagnosis for total protein excretion and creatinine clearance or a protein/creatinine ratio to confirm the diagnosis
Fetal Evaluation
• Daily fetal movement assessment (kick counts)
• Nonstress test (NST) twice weekly
• Biophysical profile if nonreactive NST
• Amniotic fluid volume assessment weekly
• Ultrasound evaluation of fetal growth every 3 weeks
Management
• Women with mild disease who achieve a gestational age of 37 weeks should undergo delivery.
• Even if conditions for induction of labor are unfavorable, the pregnancy should not continue (beyond 37 weeks’ gestation) because uteroplacental blood flow is suboptimal.
• The optimal management of mild preeclampsia remote from term is controversial. In general, there is considerable controversy regarding the need for hospitalization versus outpatient management. The use of antihypertensive drugs is not recommended nor is the use of sedatives and anticonvulsive prophylaxis.
• For a patient who has mild preeclampsia with an immature fetus, the goal of therapy should be to
 Retard the hypertensive process so as not to endanger the mother or the fetus
Retard the hypertensive process so as not to endanger the mother or the fetus
 Allow time for the fetus to mature and increase the potential for neonatal survival
Allow time for the fetus to mature and increase the potential for neonatal survival
• Therapy for patients with mild disease can be conducted by either outpatient management or hospitalization.
 Outpatient management is acceptable for patients who are compliant, who can have frequent office visits including laboratory assessments, and who can perform some form of adequate blood pressure monitoring at home.
Outpatient management is acceptable for patients who are compliant, who can have frequent office visits including laboratory assessments, and who can perform some form of adequate blood pressure monitoring at home.
 Hospitalization should be required for noncompliant patients and those who show unsatisfactory progress as outpatients.
Hospitalization should be required for noncompliant patients and those who show unsatisfactory progress as outpatients.
• If outpatient management is used, the regimen described below is recommended for mild preeclampsia.
 A patient is considered a candidate for induction of labor if she has reached 37 weeks’ gestation.
A patient is considered a candidate for induction of labor if she has reached 37 weeks’ gestation.
 She is also a candidate for induction if her blood pressure continues to rise despite conservative management.
She is also a candidate for induction if her blood pressure continues to rise despite conservative management.
 Figure 11-2 shows a sample algorithm for the management of a patient with mild preeclampsia.
Figure 11-2 shows a sample algorithm for the management of a patient with mild preeclampsia.
 After 34 weeks’ gestation, rupture of membranes, the spontaneous onset of labor or the development of intrauterine growth retardation with an estimated fetal weight less than 5th percentile, are indications for delivery.
After 34 weeks’ gestation, rupture of membranes, the spontaneous onset of labor or the development of intrauterine growth retardation with an estimated fetal weight less than 5th percentile, are indications for delivery.
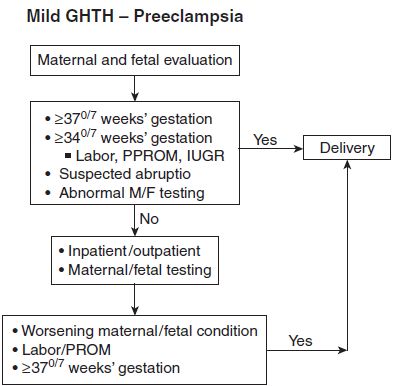
Figure 11-2. A sample algorithm for the management of a patient with mild preeclampsia.
PATIENT EDUCATION
• Close communication between the patient and physician is obligatory for successful outpatient management of mild gestational hypertension and preeclampsia. Patients are instructed to contact their managing physician for one for more of the following symptoms specific to preeclampsia:
• Blood pressure above a chosen target level
• A severe, long-lasting headache
• Epigastric or right upper quadrant abdominal pain
• Visual disturbances
• Nausea and vomiting
• The patient should also be instructed to notify her physician for the following complications of pregnancy, regardless of preeclampsia:
• Vaginal bleeding
• Leakage of fluid from the vagina
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


