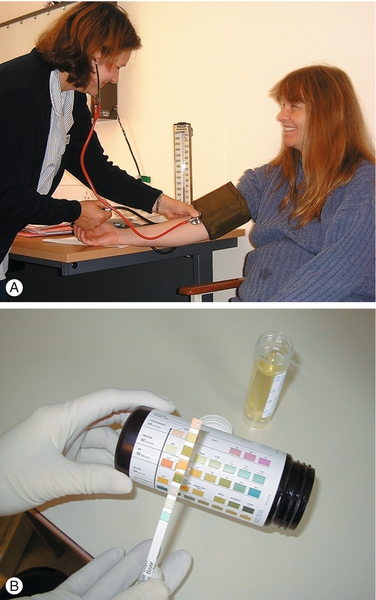
36 The term ‘gestational hypertension’ suggests a disorder of blood pressure that arises because of the presence of pregnancy. Such a simple view detracts from the fundamental pathological process that underlies this condition: gestational hypertension, pre-eclampsia and its variants are part of a multisystem disorder that can affect every organ system in the body and collectively are a major direct cause of maternal deaths in the UK. Although pre-eclampsia is associated with abnormal trophoblast invasion in the first half of pregnancy, it is not until later in the pregnancy that the clinical syndrome of pre-eclampsia is seen. The mechanisms by which the abnormal placentation and subsequent impaired placental perfusion cause the widespread vascular endothelial dysfunction that characterizes pre-eclampsia are not fully understood. Pre-eclampsia is defined as hypertension with proteinuria. It is, however, a very heterogeneous condition such that the timing of onset and the clinical course are unpredictable. In some, hypertension and proteinuria are the only manifestation, while others may present with severe renal or liver impairment, and in yet others the most prominent feature might be fetal growth restriction secondary to placental disease. Eclampsia is a generalized seizure that occurs during pregnancy in association with the features of pre-eclampsia. In a proportion of women with eclampsia, however, the features of pre-eclampsia are not evident at the time of the first seizure. The only cure for these conditions is delivery. Hypertension is the commonest medical problem encountered in pregnancy, complicating 10–15% of pregnancies. Pre-eclampsia affects 3–5% of pregnancies in total and up to 10% of pregnancies in nulliparous women. The incidence of severe pre-eclampsia is approximately 1%. Although in recent years, the rate of eclampsia in the UK appears to have fallen, hypertension in pregnancy remains one of the leading causes of maternal death in the UK, accounting for approximately five or six deaths per year. Severe pre-eclampsia is responsible for 40% of severe obstetric morbidity. Eclampsia occurs in 1 in 3000 pregnancies in the UK (0.03%) but in some developing countries, the incidence of eclampsia is 1%. One-third of the women who die from pre-eclampsia have eclamptic seizures. Hypertensive disorders also carry a risk for the baby including fetal growth restriction and stillbirth. Pre-eclampsia is the commonest cause of iatrogenic prematurity. There are long-term implications for women who suffer from hypertensive conditions in pregnancy: an increased risk of chronic hypertension and increase in lifetime risk of cardiovascular disease. In normal pregnancy, the maternal blood pressure falls slightly during the first trimester, predominantly as a consequence of reduced systemic vascular resistance. Maternal blood pressure continues to fall during the second trimester and reaches a nadir at approximately 22–24 weeks’ gestation. Thereafter, maternal blood pressure steadily increases during the third trimester to reach pre-pregnancy levels. Maternal blood pressure falls immediately after delivery of the baby, but then rises and peaks on the 4th postnatal day. Maternal blood pressure should be measured in the sitting position with an appropriate-sized cuff that is placed on the upper arm at the level of the heart (Fig. 36.1). Phase V Korotkoff sounds (i.e. ‘disappearance’ rather than ‘muffling’) should be used when measuring the diastolic blood pressure. Some automated machines for measuring blood pressure have been found to consistently underestimate true blood pressure and the use of a mercury sphygmomanometer is preferred. It is important to use an appropriate cuff size; a cuff that is too small will give an overestimate of true blood pressure. Fig. 36.1Early detection of pre-eclampsia is important. (A) Measurement of blood pressure (reproduced with permission). (B) Testing for urinary protein. Hypertension in pregnancy may be pre-existing or related to pregnancy (gestational hypertension or pre-eclampsia). An increased maternal blood pressure in early pregnancy (before 20 weeks’ gestation) is usually due to pre-existing hypertension, most commonly essential hypertension. In a young woman with pre-existing hypertension, efforts should be made to identify the rare secondary causes of hypertension such as renal disease, cardiac disease, phaeochromocytoma and endocrine disorders such as Cushing and Conn syndromes. The diagnosis of essential hypertension may be made retrospectively, if the maternal blood pressure has not returned to normal within 3 months of delivery of the baby. Gestational hypertension and pre-eclampsia rarely occur before 20 weeks’ gestation unless associated with trophoblastic disease or fetal triploidy. The hypertension associated with pre-eclampsia usually resolves within 6 weeks of delivery. Significant proteinuria is defined as a urinary protein:creatinine ratio of > 30 mg/mmol or a validated 24-h urine collection result of > 300 mg of protein. An automated reagent-strip reading device or a spot urinary protein:creatinine ratio should be used for estimating proteinuria. If an automated reagent-strip reading for proteinuria gives a result of 1 + or more, a spot urinary protein:creatinine ratio or 24-h urine collection is indicated to quantify proteinuria. Essential hypertension is more common in older women and the prognosis for pregnancy is generally good; the main risk is from superimposed pre-eclampsia. Women with essential hypertension are also at increased risk of placental abruption and fetal growth restriction. Some women taking antihypertensive drugs may be able to discontinue their medication during pregnancy, particularly during the first and second trimesters. Drugs that are commonly used for the treatment of essential hypertension during pregnancy include methyldopa, labetalol and nifedipine. Diuretics and angiotensin-converting enzyme (ACE) inhibitors are contraindicated in pregnancy but may be used for the management of hypertension during the puerperium. Recognized risk factors for gestational hypertension and pre-eclampsia are shown in Box 36.1. The precise aetiology and pathophysiology of gestational hypertension and pre-eclampsia remain unclear. It is established, however, that women who develop pre-eclampsia have a genetic or phenotypic susceptibility and that there are two distinct phases to the condition’s development: first, there is inadequate trophoblast invasion during early pregnancy and second, in later pregnancy, there is reduced placental perfusion and uteroplacental ischaemia, which in turn gives rise to the clinical syndrome. The precise mechanism by which this abnormal placentation causes the multisystem disorder that characterizes pre-eclampsia is not known. It has been suggested that there is a trigger which promotes widespread vascular endothelial dysfunction in response to the reduced placental perfusion. This endothelial dysfunction subsequently causes metabolic changes, an exaggerated maternal inflammatory response and reduced organ perfusion.
Hypertensive disorders in pregnancy
Introduction
The scale of the problem
Definitions
![]() Chronic hypertension – otherwise known as essential hypertension; presents at booking or before 20 weeks’ gestation. The woman may already be taking antihypertensive medication at her booking appointment
Chronic hypertension – otherwise known as essential hypertension; presents at booking or before 20 weeks’ gestation. The woman may already be taking antihypertensive medication at her booking appointment
![]() Gestational hypertension – sometimes also referred to as pregnancy induced hypertension (PIH); new hypertension presenting after 20 weeks (hypertension only, no proteinuria)
Gestational hypertension – sometimes also referred to as pregnancy induced hypertension (PIH); new hypertension presenting after 20 weeks (hypertension only, no proteinuria)
![]() Pre-eclampsia – hypertension and proteinuria (± multisystem involvement)
Pre-eclampsia – hypertension and proteinuria (± multisystem involvement)
![]() Eclampsia – a convulsive condition associated with pre-eclampsia
Eclampsia – a convulsive condition associated with pre-eclampsia
![]() HELLP syndrome – a syndrome of haemolysis, elevated liver enzymes and low platelet count.
HELLP syndrome – a syndrome of haemolysis, elevated liver enzymes and low platelet count.
Hypertension
![]() Hypertension in pregnancy is defined as a blood pressure of ≥ 140/90 mmHg on two occasions more than 4 h apart.
Hypertension in pregnancy is defined as a blood pressure of ≥ 140/90 mmHg on two occasions more than 4 h apart.
![]() A diastolic blood pressure of ≥ 110 mmHg on any one occasion or a systolic blood pressure of ≥ 150 mmHg on any one occasion is also significant hypertension.
A diastolic blood pressure of ≥ 110 mmHg on any one occasion or a systolic blood pressure of ≥ 150 mmHg on any one occasion is also significant hypertension.
![]() Another useful measure is the mean arterial pressure (MAP). This is the diastolic blood pressure +
Another useful measure is the mean arterial pressure (MAP). This is the diastolic blood pressure +  (systolic blood pressure – diastolic blood pressure). MAP should be maintained at < 125 mmHg.
(systolic blood pressure – diastolic blood pressure). MAP should be maintained at < 125 mmHg.
Proteinuria
Chronic hypertension
Gestational hypertension, pre-eclampsia and eclampsia
Pathophysiology
Maternal susceptibility
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


