Hodgkin Lymphoma
Melissa M. Hudson and Tanya M. Trippett
Hodgkin lymphoma is a hematopoietic malignancy with unique epidemiologic features that vary depending on the geographic region of the patient. Genetic and environmental contributions to the pathogenesis of the disease are not completely understood and represent an active area of research. Progression of Hodgkin lymphoma initially occurs along functionally contiguous lymph nodes. If untreated, extranodal involvement eventually results from hematogenous dissemination of neoplastic cells to the liver, lungs, bones, bone marrow, and other tissues. The most common clinical presentation is one of painless lymphadenopathy previously attributed to infectious or inflammatory etiologies. Other signs and symptoms vary based on the involved nodal sites and their compression of adjacent organs and tissues. Cytokine production by malignant cells results in constitutional symptoms including anorexia, pruritus, weight loss, night sweats, and fever in some patients.
Providing care for children with Hodgkin lymphoma challenges the pediatric and radiation oncology team to accomplish the tandem goals of optimizing disease control and limiting long-term morbidity.1 Historically, treatment approaches mirrored those used for adults, but outcome was compromised by unacceptable musculoskeletal hypoplasia resulting from high dosage radiation of large volumes in physically immature children. Pediatric patients are also more likely to experience cardiovascular toxicity associated with anthracycline chemotherapy and thoracic radiation, which may predispose them to early mortality associated with cardiomyopathy and coronary artery disease.2 There are also specific gender-related predispositions to treatment effects. Boys are more vulnerable to gonadal toxicity following cumulative doses of alkylating agent chemotherapy used in primary treatment regimens, whereas girls generally maintain ovarian function unless chemotherapy is combined with infradiaphragmatic radiation. Conversely, girls treated with anthracycline chemotherapy, particularly if younger than age 5 years, are more likely than boys to experience cardiotoxicity. Likewise, young women treated with thoracic radiation during puberty have a substantially increased risk of a breast malignancy that is not observed in their male counterparts.3 Because of these unique developmental and gender-related predispositions to therapy effects, there is no single treatment method that is ideal for all patients. Contemporary treatment uses a risk-adapted approach that considers the prognostic features of the disease presentation in the context of a patient’s predisposition to long-term toxicity related to age and gender.
 ETIOLOGY AND EPIDEMIOLOGY
ETIOLOGY AND EPIDEMIOLOGY
The epidemiologic, clinical, and histologic features of Hodgkin lymphoma are different in economically developed and developing countries.4 Epidemiologic studies support three distinct forms of Hodgkin lymphoma attributable to interactions of environmental and host factors.5 The childhood form (age 14 years or younger) is characterized by a high incidence of the mixed cellularity histologic subtype in children living in poorer socioeconomic environments. The young adult form (ages 15 to 34 years) shows a predominance of the nodular sclerosing histologic subtype in Caucasian adolescents and young adults in developed countries. An older adult form (ages 55 to 74 years) produces the characteristic bimodal distribution of incidence of the disease in industrialized countries. In developing countries, the early peak occurs before adolescence.
Hodgkin lymphoma is more common in males than in females in all parts of the world. The gender ratio varies from 2:1 in Europe and America to over 3.5:1 in Asia. The male predominance is most marked in patients younger than age 10 years. In adolescents, the gender difference in incidence is less conspicuous, particularly for the nodular sclerosing histologic subtype. Beyond age 55, the gender difference in incidence decreases and is similar across histologic subtypes. Hodgkin lymphoma is rarely diagnosed in children younger than age 5 years in economically developed countries.
A genetic predisposition to Hodgkin lymphoma is suggested by the incidence variation among racial and ethnic groups, familial aggregation of the disease, and association with specific human leukocyte antigens.4,6 In some groups, race and ethnicity appear to predict the risk of Hodgkin lymphoma independent of socioeconomic status. For example, Asians consistently have lower incidence rates despite the marked international differences in socioeconomic conditions. Many investigators have observed concordance of Hodgkin lymphoma in first-degree relatives, including sibling and parent–child pairs. In studies of concordant monozygotic twins, the elevated risk of Hodgkin lymphoma ranges from threefold among first-degree relatives to sevenfold in siblings. Hodgkin lymphoma also develops more frequently in individuals with congenital or acquired immunodeficiency, leading to the speculation that an inherited subtle immune abnormality may predispose to the development of Hodgkin lymphoma by increasing the risk of malignant transformation induced by environmental factors.
Characteristic epidemiologic features, including the bimodal age incidence and socioeconomic influences, prompted the speculation that an infectious agent may contribute to the pathogenesis of some types of Hodgkin lymphoma.4 Epstein-Barr virus (EBV) was indirectly implicated in epidemiologic studies demonstrating an excess risk of Hodgkin lymphoma following infectious mononucleosis and elevated anti-EBV titers in patients with Hodgkin lymphoma compared to healthy controls. Supporting evidence of EBV association with Hodgkin lymphoma includes the localization of viral genomes in the Reed-Sternberg cells, expression of EBV-latent gene products in the tumor specimens, and the demonstration of clonal infection.7 Clear differences exist with the expression of EBV-associated antigens in cases of Hodgkin lymphoma with respect to histologic subtype, geographic region, and age. EBV-associated Hodgkin lymphoma occurs more frequently in children in developing countries who present with mixed cellularity histology. These data suggest that EBV may be a cofactor in the pathogenesis of some cases of Hodgkin lymphoma.
 PATHOLOGY
PATHOLOGY
Hodgkin lymphoma is histologically characterized by the presence of Reed-Sternberg cells within an inflammatory infiltrate of normal lymphocytes, histiocytes, plasma cells, eosinophils, and neutrophils. The neoplasm is unusual because the acknowledged malignant Hodgkin and Reed-Sternberg (HRS) cells usually represent only 0.1 to 10% of the cellular infiltrate of the tumor. Techniques such as microdissection and single-cell polymerase chain reaction (PCR) have confirmed the B-lymphoid origin of the disease through identification of clonal immunoglobulin (Ig) rearrangements in enriched populations of HRS cells removed from their benign polyclonal inflammatory background.8 Rarely, the HRS cells have been found to contain T-cell receptor gene rearrangements, suggesting that some of these tumors may be of T-lymphoid lineage, but these cases remain controversial. Thus, Hodgkin lymphoma is felt to represent a unique type of B-cell neoplasm. Consequently, the currently used World Health Organization (WHO) classification has abandoned the term Hodgkin’s disease, thought to reflect the lack of knowledge regarding the true origin of the HRS cells. Unlike other lymphoid neoplasms, cytogenetic abnormalities characteristic of Hodgkin lymphoma have not been identified.
The current WHO histologic classification of Hodgkin lymphoma is largely based on the Rye modification of the Lukes and Butler classification schema. The WHO classification recognizes two major subtypes of Hodgkin lymphoma, classical Hodgkin lymphoma and nodular lymphocyte predominance Hodgkin lymphoma, based on their biological and clinical features.9 Classical Hodgkin lymphoma includes 4 histologic subtypes that differ by tissue architecture, the presence of fibrosis, and the features of the associated inflammatory infiltrate: nodular sclerosis, mixed cellularity, lymphocyte rich, and lymphocyte depleted. All histologic subtypes are responsive to therapy. Histologic subtyping is valuable because of its association with clinical findings such as sites of involvement, stage at presentation, and systemic symptoms.
 CLINICAL MANIFESTATIONS
CLINICAL MANIFESTATIONS
The most common presentation of Hodgkin lymphoma is asymptomatic cervical or supraclavicular lymphadenopathy. Two thirds of these patients will also have involvement of mediastinal lymph nodes, which may produce a nonproductive cough or other symptoms of tracheal or bronchial compression. Rarely, patients may present with life-threatening cardiovascular or respiratory decompensation as a result of tumor infiltration of the pericardium, obstruction of superior vena cava blood flow, or airway compression by bulky mediastinal lymphadenopathy. Children present less frequently with axillary or inguinal lymphadenopathy. Primary subdiaphragmatic nodal involvement is rare and occurs in less than 10% of patients. In some cases, extension of enlarged retroperitoneal lymph nodes through neural foramina produces pain and para- or quadraparesis from spinal cord compression.
About 30% of children exhibit constitutional symptoms of fever, drenching night sweats, and unexplained weight loss within the previous 6 months, which have a negative impact on prognosis because of their association with more disseminated disease. “Pel-Ebstein” fevers are typically associated with Hodgkin lymphoma and are characterized by periodic febrile episodes (with our without night sweats) lasting for several days, followed by afebrile periods of days or weeks. Less commonly reported systemic symptoms such as pruritus and alcohol-induced pain do not influence outcome.
 LABORATORY FINDINGS
LABORATORY FINDINGS
Nonspecific abnormalities of hematologic parameters may be observed at diagnosis. Peripheral blood changes include neutrophilic leukocytosis, lymphopenia, eosinophilia, and monocytosis. Elevations of erythrocyte sedimentation, serum copper, ferritin, or C-reactive protein levels reflect activation of the reticuloendothelial system and may be used to monitor disease activity if they are abnormal at diagnosis. Anemia usually indicates the presence of advanced disease and most commonly results from impaired mobilization of iron stores. Coombs’ positive hemolytic anemia associated with reticulocytosis and normoblastic hyperplasia of the bone marrow has also been described at presentation of Hodgkin lymphoma. Abnormalities of chemical parameters are infrequent in Hodgkin lymphoma. Occasionally, levels of serum lactate dehydrogenase will be elevated at diagnosis. Elevation of serum alkaline phosphatase levels beyond that expected for age may be associated with the presence of bony metastases. Liver function studies are generally unreliable indicators of hepatic disease.
Hodgkin lymphoma has been described in association with several autoimmune diseases including immune thrombocytopenia purpura (ITP), nephrosis, and hemolytic anemia. Of these, ITP is most frequently observed and its prognosis for response to therapy is related to the status of the underlying Hodgkin lymphoma. ITP presenting during remission of Hodgkin lymphoma lacks prognostic significance. Patients with Hodgkin lymphoma also exhibit immune system abnormalities at diagnosis that may persist after therapy. These include abnormalities of cell-mediated immunity resulting from enhanced sensitivity to suppressor T-lymphocytes and reduction of natural killer cell cytotoxicity. After treatment, humoral immunity may be transiently depressed.
Other inflammatory causes of lymphadenopathy, especially those with an indolent course (eg, atypical mycobacterium or toxoplasma infections), should be considered in the differential diagnosis of lymphadenopathy. Infectious agents producing lymphadenopathy can often be distinguished from Hodgkin lymphoma by their characteristic clinical presentations. Non-Hodgkin lymphoma may have similar presenting signs and symptoms, but is typically associated with a more rapid growth of affected lymph nodes. Also, children with non-Hodgkin lymphoma more frequently exhibit elevations of serum uric acid and lactate dehydrogenase levels. Although lymphadenopathy resulting from bacterial or viral infection is more common than lymph node enlargement from malignant infiltration, lymphadenopathy persisting beyond 3 to 4 weeks should be considered for biopsy. Occasionally the site, for example, in the supraclavicular region and character, for example, firm, fixed painless lymphadenopathy, may indicate the need for immediate biopsy. In such cases, an excisional lymph node biopsy is the preferred procedure to establish a diagnosis as it permits evaluation of the entire nodal architecture.
 DIAGNOSIS AND CLINICAL STAGING
DIAGNOSIS AND CLINICAL STAGING
Biopsy is required to establish the diagnosis of Hodgkin lymphoma. Lymph node excision represents the optimal method of diagnosis because the malignant Hodgkin and Reed-Sternberg (HRS) cells can be evaluated within the context of the nodal architecture unique to individual histologic subtypes. If a noninvasive needle biopsy is planned, multiple tissue passes should be performed to facilitate assessment of nodal architecture.
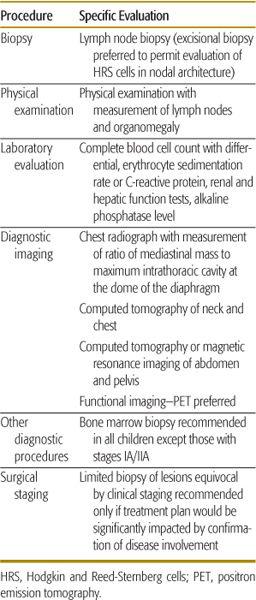
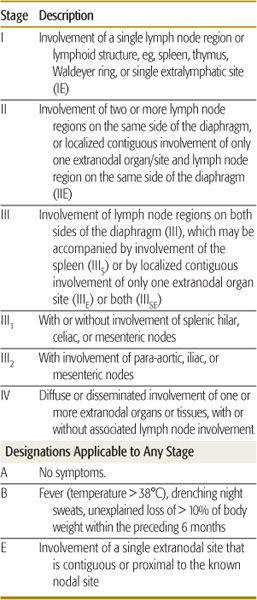
The goal of the staging evaluation is to identify sites and characteristics of disease to permit as accurate a risk assessment as possible for planning treatment. The routine use of systemic chemotherapy, coupled with advances in diagnostic imaging technology that permitted more accurate evaluation of abdominal and pelvic lymph node involvement, made staging laparotomy used during the 1970s obsolete. Currently, surgical staging is recommended in children only if the findings will significantly alter the treatment plan. Table 452-1 summarizes the recommended steps in the diagnostic workup for pediatric Hodgkin lymphoma. Table 452-2 outlines the Ann Arbor staging classification, which has been the internationally accepted staging system for Hodgkin lymphoma since 1971.
Table 452-1. Diagnostic and Staging Evaluations for Pediatric Hodgkin Lymphoma
 THERAPY
THERAPY
Dramatic progress has been made in the development of curative therapy for children and adolescents with Hodgkin lymphoma over the past 50 years.1,10 Contemporary treatment protocols for pediatric Hodgkin lymphoma produce long-term, disease-free survival in 70% to 90% of patients with advanced stage disease, and 85% to 100% of patients with localized disease. The majority (60–80%) of children with extranodal disease will also be cured of their disease. This therapeutic success has provided the opportunity to evaluate the long-term impact of treatment on morbidity and mortality. Appreciation of treatment sequelae has prompted refinements in therapy designed to reduce growth impairment, infertility, second malignancy, and life-threatening organ dysfunction. Current treatment strategies focus on reducing therapy for patients with favorable disease characteristics and reserve more intensive treatment modalities for patients with relapsed or refractory disease.
Table 452-2. Ann Arbor Staging Classification for Hodgkin Lymphoma
Treatment options for children and adolescents with Hodgkin lymphoma comprise multiagent chemotherapy alone or combined modality therapy with chemotherapy and low-dose radiation therapy. The desire to avoid radiation-induced growth inhibition of bones and soft tissues and the induction of secondary solid tumor malignancies led to the abandonment of the use of radiation therapy as a single modality in children with Hodgkin lymphoma. Concerns about radiation-induced carcinogenesis and cardiopulmonary toxicity, which are more prevalent following standard-dose (35–44 Gy) than low-dose (15–25.5 Gy) levels, continue to significantly influence contemporary treatment approaches.3
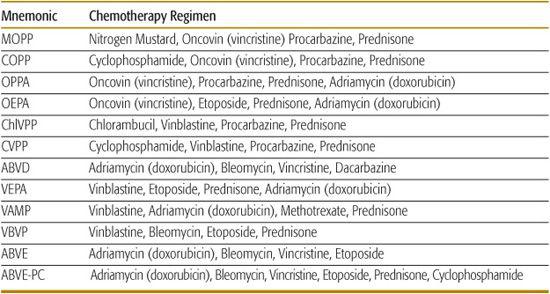
Multiagent chemotherapy is still largely derived from the original non-cross-resistant MOPP (mechlorethamine, vincristine [Oncovin], prednisone, and procarbazine) and ABVD (doxorubicin [Adriamycin], bleomycin, vinblastine, and dacarbazine) regimens.11,12 Treatment sequelae following MOPP comprise an increased risk of acute myelogenous leukemia and infertility, which have been correlated with the cumulative dose of alkylating agents in the combination. The risk of secondary leukemia can be reduced by limiting the total dose of alkylating agents and substituting other less leukemogenic drugs, such as cyclophosphamide, for mechlorethamine.
ABVD is effective therapy for Hodgkin lymphoma that does not produce an excess risk of secondary leukemia or infertility. However, concerns regarding dose-related cardiac and pulmonary toxicity attributable to doxorubicin and bleomycin in the combination have limited its singular use in pediatric regimens. As a result, ABVD and similar derivative combinations are commonly used in treatment regimens prescribing fewer cycles of chemotherapy for patients with favorable disease characteristics at presentation, or alternated with regimens containing alkylating agents, for example, MOPP or COPP (cyclophosphamide vincristine, procarbazine, and prednisone), in patients with advanced or unfavorable disease.13,14
Several trials have established the efficacy of treatment with non-cross-resistant chemotherapy alone in pediatric Hodgkin lymphoma.13 Chemotherapy-alone protocols offer advantages for children managed in centers lacking radiation facilities and trained personnel, as well as diagnostic imaging modalities needed for clinical staging. This treatment option also avoids the potential long-term growth inhibition, organ dysfunction, and solid tumor induction associated with radiation. On the other hand, chemotherapy-alone treatment protocols usually prescribe higher cumulative doses of alkylating agent and anthracycline chemotherapy, which may produce acute and late treatment morbidity from myelosuppression, cardiotoxicity, gonadal injury, and secondary leukemia.
The desire to reduce the dose-related toxicity of agents in the MOPP and ABVD regimens popularized the use of alternating, hybrid, and derivative multiagent chemotherapy regimens (Table 452-3). Initially, standard-dose (35–44 Gy), extended-volume radiation therapy was added to enhance local tumor control. The efficacy of these regimens led to subsequent trials that demonstrated excellent cure rates using fewer cycles of non-cross-resistant chemotherapy with reduced radiation doses (15–25.5 Gy) and fields.
Table 452-3. Chemotherapy Combinations for Pediatric Hodgkin Lymphoma
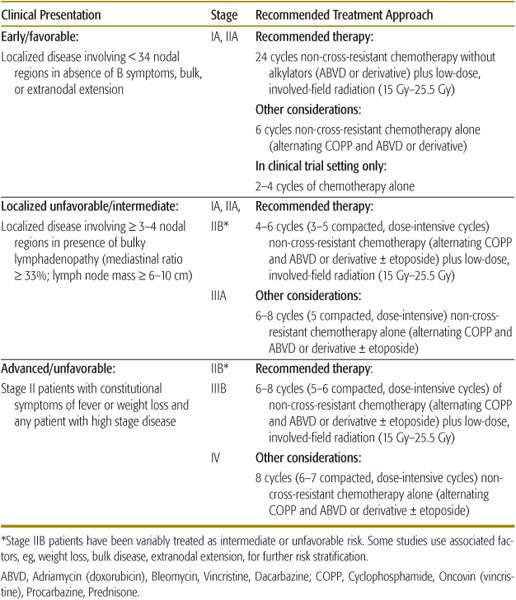
Contemporary therapy planning utilizes a risk-adapted approach based on the presenting features of the disease.1 Ongoing trials for patients with favorable disease presentations are evaluating the effectiveness of treatment with fewer cycles of combination chemotherapy alone that limit doses of anthracyclines and alkylating agents. For patients with unfavorable disease presentations, contemporary trials are testing if chemotherapy and radiotherapy can be limited in patients who achieve a rapid early response to dose-intensive chemotherapy regimens. Table 452-4 provides general risk-adapted treatment recommendations.
Most relapses in patients with Hodgkin lymphoma occur within the first 3 years, although some patients may relapse as long as 10 years after initial diagnosis.15 Treatment and ultimate prognosis after relapse depend on the initial therapy type and time of relapse. Standard multiagent chemotherapy and radiation therapy may salvage 40% to 50% of children who maintained initial remission for 1 or more years, but late treatment complications such as second malignancies and cardiovascular disease may reduce ultimate survival.16 Patients who develop refractory disease during or within 1 year of completing therapy respond poorly to conventional salvage therapy, as do patients with multiple relapses. Consolidation with myeloablative therapy followed by hematopoietic cell transplantation provides these high-risk patients the best opportunity for a durable remission. Autologous hematopoietic stem cell transplantation (HSCT) has been preferred for patients with relapsed Hodgkin lymphoma because of the greater morbidity and mortality associated with allogeneic HSCT. Overall survival after autologous HSCT in pediatric patients with relapsed Hodgkin lymphoma ranges from 30% to 60%. Reduced intensity or nonmyeloablative allogeneic HSCT is under evaluation as a retrieval therapy for children with recurrent/refractory disease after autologous HSCT.17 Nonmyeloablative conditioning regimens most often use a nontoxic immunosuppression with the goal of establishing a graft-versus-lymphoma effect that provides a platform for adoptive cellular immunotherapy.
Table 452-4. Recommended Treatment Approach in Pediatric Hodgkin Lymphoma
 PROGNOSIS
PROGNOSIS
Today, the majority of children and adolescents diagnosed with Hodgkin lymphoma will enjoy long-term, disease-free survival. Consequently, ongoing clinical trials are focusing on two primary objectives: (1) to maintain cure rates and further reduce treatment sequelae in patients with favorable disease presentations; and (2) to identify biologic and clinical characteristics of patients with a high risk of treatment failure, for whom treatment must be further intensified to improve outcome. Because of the paucity of novel anti-neoplastic approaches with safer toxicity profiles, alterations in the currently effective treatment strategies must proceed cautiously to assure that disease-free survival is not compromised.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


