Fig. 57.1
Clinical photograph of a patient with hepatoblastoma showing a large abdominal mass
Less common symptoms are: decreased appetite, anorexia, weight loss, nausea, vomiting, back pain, early puberty in boys, fever, and abdominal pain.
Rarely, they present with acute abdomen due to tumor rupture .
Investigations
Complete blood count, liver function tests, electrolytes, blood urea, and creatinine .
Alpha-fetoprotein (AFP) test: AFP levels in the blood can be used both to diagnose hepatoblastoma and to monitor its response to treatment and follow-up. AFP levels of less than 100 μg/mL is a poor prognostic factor.
Abdominal and chest x-rays: This reveals a right upper quadrant abdominal soft-tissue mass. Calcification is seen in approximately 6 % of hepatoblastomas (Fig. 57.2) .
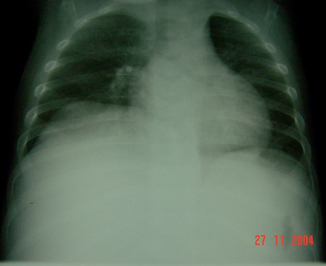
Fig. 57.2
Chest x-ray of a patient with hepatoblastoma showing a large right-sided upper abdominal soft-tissue mass pushing the diaphragm upwards
Abdominal ultrasound: This is valuable in detecting the organ of origin of the tumor, its size, and nature as well as vascular involvement.
Chest and abdominal computed tomography (CT scan): This allows more accurate assessment of site and size of the tumor as well as involvement of nearby structures particularly regional lymph nodes. CT scanning of the chest is important to assess for pulmonary metastases (Fig. 57.3).
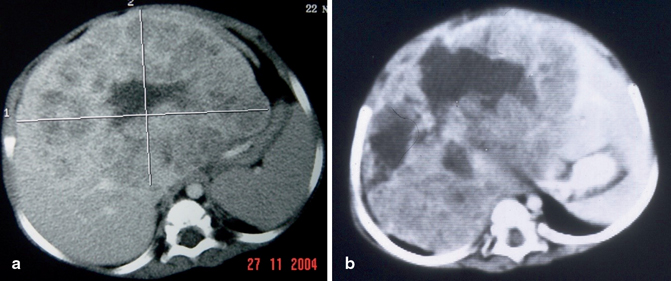
Fig. 57.3
Abdominal CT scans showing a large hepatoblastoma arising from the left lobe of the liver in one (a) and from the right lobe of liver in (b)
Magnetic resonance imaging (MRI): This is superior to CT scan and allows more and accurate outlines of the tumor and feasibility of resection (Fig. 57.4) .
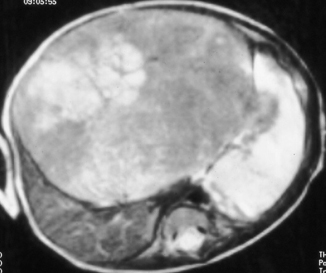
Fig. 57.4
Magnetic resonance imaging (MRI) of the abdomen showing a large hepatoblastoma
Technetium-99 m sulfur-colloid liver scintigraphy (Fig. 57.5): Hepatoblastomas usually demonstrate hypervascularity, with prominent tracer avidity at the site of the tumor within a few seconds of the appearance of the bolus in the abdominal aorta. This increased activity persists into the venous phase. Delayed images typically demonstrate a photopenic defect at the tumor site.
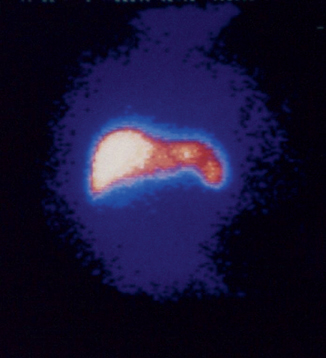
Fig. 57.5
Isotope scan showing a hepatoblastoma arising from the right lobe of the liver
Bone scans: This is recommended to evaluate for bone metastases when the patient is symptomatic.
Positron emission tomography (PET) CT: Most hepatoblastomas are positive on fludeoxyglucose PET before therapy and therefore this nuclear scan may be helpful for detection of metastasis and assessment of tumor viability .
Staging
Stage I: Hepatoblastoma that is completely removed with surgery .
Stage II: Hepatoblastoma that is mostly removed by surgery but very small amounts of the cancer are left in the liver.
Stage III: Hepatoblastoma that cannot be completely removed and the cancer cells are found in the lymph nodes.
Stage IV: Hepatoblastoma that has spread (metastasized) to other parts of the body.
Recurrent: The disease has returned after it has been treated. It may come back in the liver or in another parts of the body.
Metastases at diagnoses occur in 10–20 % of patients, with the lung being the predominant site of metastases both at presentation and relapse. Other sites of distant metastases, including brain and bone, are rare and usually occur in the setting of relapsed disease .
Fig. 57.6
Stage 1: Tumor involves only one quadrant; three adjoining liver quadrants are free of tumor
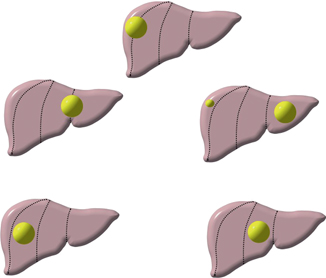
Fig. 57.7
Stage 2: Tumor involves one or two quadrants; two adjoining quadrants are free of tumor
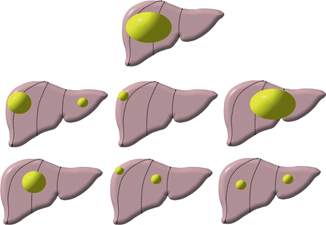
Fig. 57.8
Stage 3: Tumor involves three quadrants and one quadrant is free of tumor or tumor involves two quadrants and two nonadjoining quadrants are free of tumor
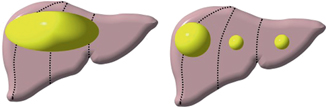
Fig. 57.9
Stage 4: Tumor involves all four quadrants; there is no quadrant free of tumor
Pathology
Histologically, hepatoblastoma is composed of epithelial and mesenchymal elements in varying proportions and at various stages of differentiation (Figs. 57.10 and 57.11 ) .
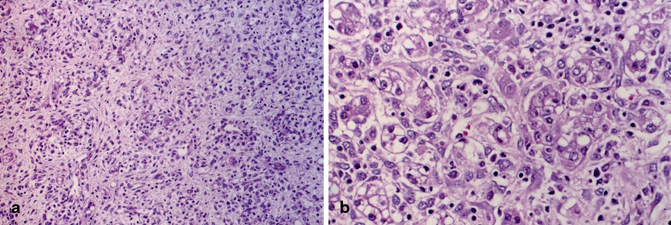
Fig. 57.10
a and b Histological picture of hepatoblastoma. Note the epithelial and mesenchymal components and the large hyperchromatic nuclei
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


