Hand, Foot, and Limb Anomalies
INTRODUCTION
The orthopedic examination of a newborn can at times be intimidating, even to an experienced pediatric orthopedist; just as children are not small adults, neonates are not small children. A thorough, consistent approach and agreed-on nomenclature can help identify musculoskeletal anomalies that may be present in isolation or may be part of a larger syndrome; treatment may vary from observation to casting or bracing to surgery. Being familiar with the most common diagnoses, their treatments, and anticipated outcomes can help ease parental anxiety and avoid unnecessary delays in treatment or overtreatment. Management of parental expectations is often one of the most important roles we as physicians serve.
PHYSIOLOGIC MUSCULOSKELETAL FINDINGS
Familiarity with the range of musculoskeletal findings in a newborn is important in that the line between physiologic and pathologic can be subtle. Often, severity and flexibility can be clues about whether a finding is normal.
Joint contractures, especially of the elbows, hips, and knees, are normal and slowly resolve over time; absence of these normal contractures may be the sign of an abnormality, such as arthrogryposis or congenital knee dislocation. If the contractures are especially severe and very stiff, that may also be a sign of arthrogryposis. Thumb-in-palm positioning is physiologic at birth, but lack of resolution over time may be a sign of neurologic abnormality.
Most infants are born with a bowed appearance of the tibia, which, in conjunction with the common external rotation contracture at the hip, gives the legs a “bowlegged” appearance. In fact, most of the apparent bowing is actually caused by internal tibial torsion; when the patella is placed directly forward, the knee will appear neutral to even slightly valgus. With time, the external rotation contracture at the hip and internal tibial torsion resolve so that by toddlerhood, most legs have “straightened out.” Abnormal tibial alignment in the neonate includes posteromedial and anterolateral bowing. Posteromedial bowing of the tibia is usually distal and often is associated with calcaneovalgus positioning of the foot; both resolve over time without formal treatment, but posteromedial bowing is associated with an ultimate leg length discrepancy of up to 3–4 cm that parents should be informed of at the outset. Anterolateral bowing can be midshaft or distal and is commonly associated with neurofibromatosis type 1 (NF 1); if anterolateral bowing is found on physical examination, it should be further evaluated by x-ray (Figure 64-1), and the patient should be closely examined for café-au-lait spots, axillary freckling, iris hamartomas, and other manifestations of NF 1. Finally, more nonspecific bowing of the tibia or the femur can be a sign of osteogenesis imperfecta.
FIGURE 64-1 Radiographic appearance of anterolateral tibial bowing seen in neurofibromatosis type 1.
Variation in foot alignment is extremely common in newborns and is usually the result of intrauterine packaging. The most common pathologic conditions of the foot include clubfoot and congenital vertical talus (CVT), which are covered further in this chapter. Findings that are more benign include metatarsus adductus and calcaneovalgus. Metatarsus adductus is characterized by a “bean-shape” to the foot: The lateral border is convex, and the forefoot is adducted on the mid- and hindfoot. Occasionally, the forefoot is slightly supinated as well, and the foot can be confused for a clubfoot. If the hindfoot is normal and the deformity is completely passively correctable, it is likely a metatarsus adductus. As long as it is flexible and actively corrects with eversion of the foot, formal treatment is usually not necessary; spontaneous resolution is expected. If the foot is a little stiffer and the foot can only be passively corrected to neutral, occasionally stretching or casting may be recommended; feet in an extremely small subset do not correct and undergo surgical correction after the age of 4 to 6 years.
Calcaneovalgus is common in newborns and is characterized by extreme dorsiflexion of the entire foot with some component of eversion; the foot can be “plastered against the tibia.” It is caused by intrauterine packaging, and its natural history is characterized by reliable resolution, although occasionally stretching exercises will be recommended if it is tight. It is important to distinguish isolated calcaneovalgus from calcaneovalgus associated with a posteromedial bow due to a possible projected leg length discrepancy associated with the latter. The distinguishing feature will be the apex of the deformity, which is in the ankle in the isolated calcaneovalgus foot and in the tibia when associated with posteromedial bowing.
ANOMALY BY ANATOMIC LOCATION
Upper Extremity
Neonatal Brachial Plexus Palsy
Brachial plexus injuries are one of the more common orthopedic conditions presenting in the neonatal setting. The incidence of this condition is thought to be between 0.1% and 0.4% of live births,1,2 although the incidence has been slightly decreasing in the United States over the last decade.3 Because the presumed mechanism of injury is a stretch across the brachial plexus, risk is increased by those factors associated with larger infants with wider shoulder girdles and difficult or prolonged labor. Commonly cited risk factors include maternal diabetes; high birth weight (once fetal weight is greater than 3500 g, the shoulder cross-sectional area often exceeds the size of the infant’s head); breech position; prolonged second stage of labor; forceps delivery; prior delivery of an infant with a brachial plexopathy; and shoulder dystocia. In the most recent survey of US births, shoulder dystocia had a 100 times increased risk of brachial plexus palsy; birth weight greater than 4500 g and forceps delivery had 14 times and 9 times greater risk, respectively.3 However, in this study, the majority of patients with neonatal brachial plexus injury had no known risk factors, and other authors have found that although risk factors like maternal diabetes, birth weight greater than 4000 g, and prolonged labor increase the chances of shoulder dystocia, they do not necessarily increase the risk of brachial plexus palsy.4 In summary, like many orthopedic conditions, certain factors may place patients at increased risk of brachial plexus injury, but most patients presenting with the condition have no known risk factors.
As mentioned, the mechanism of injury is a stretch to the brachial plexus, usually during the process of birth. The amount of stretch needed to cause a permanent or severe neurologic injury is not exactly known. The brachial plexus itself is composed of nerve roots C5 to T1, which branch and combine to become the nerves of the arm and shoulder girdle. The most common nerve roots affected are C5 and C6, also known as Erb palsy, which leads to weakness or absence of shoulder abduction, external rotation, elbow flexion, and wrist extension. This leads to the classic “waiter’s tip” position of the upper extremity, so called because the flail arm is held adducted, internally rotated with the elbow extended and the palm turned up, as if the baby were waiting to be slipped a subtle gratuity. C7 may also occasionally be involved. Even less frequent is an injury to the entire plexus (C6 to T1), which affects function of the hand, as does isolated injury to the lower plexus (Klumpke palsy), which results in a clawed appearance of the hand. Lower plexus lesions are thought to be caused by traction on an abducted arm, as when an infant is delivered by being pulled by his or her arm above the head.
In addition to which nerves roots are involved, the level at which they are involved is an important prognostic indicator: The ganglion arises just adjacent to the spinal cord, so that preganglionic lesions are essentially nerve root avulsions directly off the spinal cord and have significantly worse chance for spontaneous motor recovery than postganglionic lesions. The presence of unilateral Horner syndrome, which is characterized by a droopy eyelid with constricted pupil and decreased sweating on one side of the face (ptosis, miosis, and anhydrosis), indicates injury to the sympathetic chain and carries a poor prognosis for spontaneous recovery. Injury to the phrenic nerve, indicated by an elevated hemidiaphragm, and to the long thoracic nerve, indicated by a winged scapula, also raise serious concern about a preganglionic injury.5
The typical presentation of an infant with a brachial plexus injury is a flail arm that is noted to have a lack of movement following delivery; when it is noticed depends on the circumstances surrounding the birth and the severity of the palsy. Bilaterality is extremely rare and should raise the possibility of syringomyelia, arthrogryposis, or arachnoid cyst.6,7 The top 3 differential diagnoses for a nonmoving arm are neonatal brachial plexus injury, fracture (clavicle or humerus), or infection (osteomyelitis or septic arthritis). Less-common possibilities are arthrogrypotic conditions that affect the upper extremities preferentially and intraspinal causes such as syringomyelia or an arachnoid cyst. The perinatal history and physical examination are often all that is needed to make the diagnosis. For example, the history can be helpful in distinguishing infection from a brachial plexus palsy or fracture because in infection the limb was likely normal at birth and subsequently the parents and caregivers may have noticed a progressive or sudden loss of active movement of the arm as the infection manifested. On physical examination, there is no arm movement with Moro reflex testing, whereas in a flail arm caused by infection or fracture, the patient will typically still have some movement with the Moro reflex (the patient is not moving the arm because of pain, not because of a problem with nerve communication to the muscles of the arm—a pseudoparalysis vs a true palsy). It is important to note that a small subset of patients with a fracture may have a concomitant brachial plexus injury, up to 10% of clavicle fractures,8 so the physical examination of a patient with neonatal brachial plexus palsy should include palpation of the clavicle and humerus to look for deformity or crepitus indicative of fracture. After a thorough history and physical examination, if there is still a question of the diagnosis, an x-ray can be helpful in finding a fracture, and ultrasound can be helpful in evaluating for a joint effusion in infection or altered anatomy in a transphyseal separation. The physical examination is also helpful in distinguishing arthrogryposis from neonatal brachial plexus palsy; early on, passive range of motion will be normal to near normal in a brachial plexus palsy as it is a relatively recent injury, whereas joint motion will be limited in arthrogrypotic infants.
Many patients with neonatal brachial plexus palsy will improve over time and will not require surgical intervention; the main goal of early treatment is to maintain passive range of motion while waiting for nerve recovery. Occupational therapy should be utilized along with a supervised home stretching program to maintain motion, but initiation is usually deferred for a week or 2 after birth to allow any associated pain to subside. The prevention of joint contractures is of utmost importance. Because the decision to proceed with surgery is based on the degree of motor function recovery, patients should be referred to, and followed by, a surgical specialist early on so that sequential neurologic examinations can be initiated and documented, preferably by the same provider. The rates of spontaneous, complete recovery vary depending on the study and are mentioned9 as anywhere from 7% to 95%; poor prognostic factors for recovery include total plexopathy, Horner syndrome, and involvement of lower cervical nerve roots.
Surgical treatment consists of early microsurgical reconstruction and later procedures for residual deformities and contractures. Early microsurgical reconstruction is often undertaken at 3 months in patients with global plexopathy and Horner syndrome because of an unfavorable natural history. Otherwise, traditionally, return of antigravity biceps function has been used to help predict recovery and, in its absence, identify patients who will benefit from early surgical intervention. Exactly how long to wait for bicep functional recovery is somewhat controversial; historically, 3 months has been the cutoff as early studies suggested that patients without biceps function by age 3 months eventually gained this function but had poorer shoulder outcomes at 5 years and an increased likelihood of secondary procedures later.10 Later secondary procedures are targeted toward a patient’s residual deficiencies and deformities, most commonly lack of shoulder abduction and internal rotation contracture at the shoulder; they consist of joint releases, tendon transfers, and humeral derotation osteotomies.
Outcomes of patients with neonatal brachial plexus palsy vary widely from complete recovery with normal upper extremity function to profound impairment of the limb. Girth of the affected limb may be smaller, and asymmetry may lead to postural deformities and abnormal gait.10 Despite all of this, however, children with brachial plexus palsy lead full lives; for example, they participate in sports at the same rate as their peers.11
In summary, neonatal brachial plexus palsy incidence appears to be decreasing, potentially because of better understanding of its etiology; however, most patients have no known risk factors. Diagnosis is made by physical examination, and it can be distinguished from other causes of a flail extremity by total lack of movement with reflex testing and normal passive joint motion early on. Initial treatment is supportive and is aimed toward maintaining range of motion; the timing of microsurgical reconstruction is controversial but is generally accepted at age 3 months for those patients who have more severe injuries as evidenced by Horner syndrome or total plexopathy. For the most common presentation, Erb palsy, spontaneous recovery and full return of function can be expected for many patients.
Arm Dysplasias
Longitudinal deficiencies of the upper extremity represent a spectrum of dysplasias and hypoplasias affecting any part of the arm—humerus, radius, ulna, hand, fingers, and thumb—and include phocomelia (proximal longitudinal dysplasias), radial dysplasias (radial club hand), and ulnar dysplasias (ulnar club hand). These are rare deformities, with the more common radial deficiencies occurring in 1 in 30,000 live births and the rarer ulnar deficiencies in 1 in 100,000 births. Thalidomide-related phocomelia is thought to have affected approximately 10,000 living patients worldwide in the 1950s and 1960s.
True isolated phocomelia with a clear intercalary or segmental defect that is otherwise normal above and below the defect with a normal hand is extremely rare; most cases diagnosed as phocomelia in fact represent the proximal extent of a radial or ulnar longitudinal dysplasia12; this chapter therefore focuses on these 2 deficiencies. Although they share nomenclature, radial and ulnar longitudinal deficiencies are very different in their associations, presentations, and severity (Table 64-1).
Table 64-1 Comparison of Radial and Ulnar Dysplasias
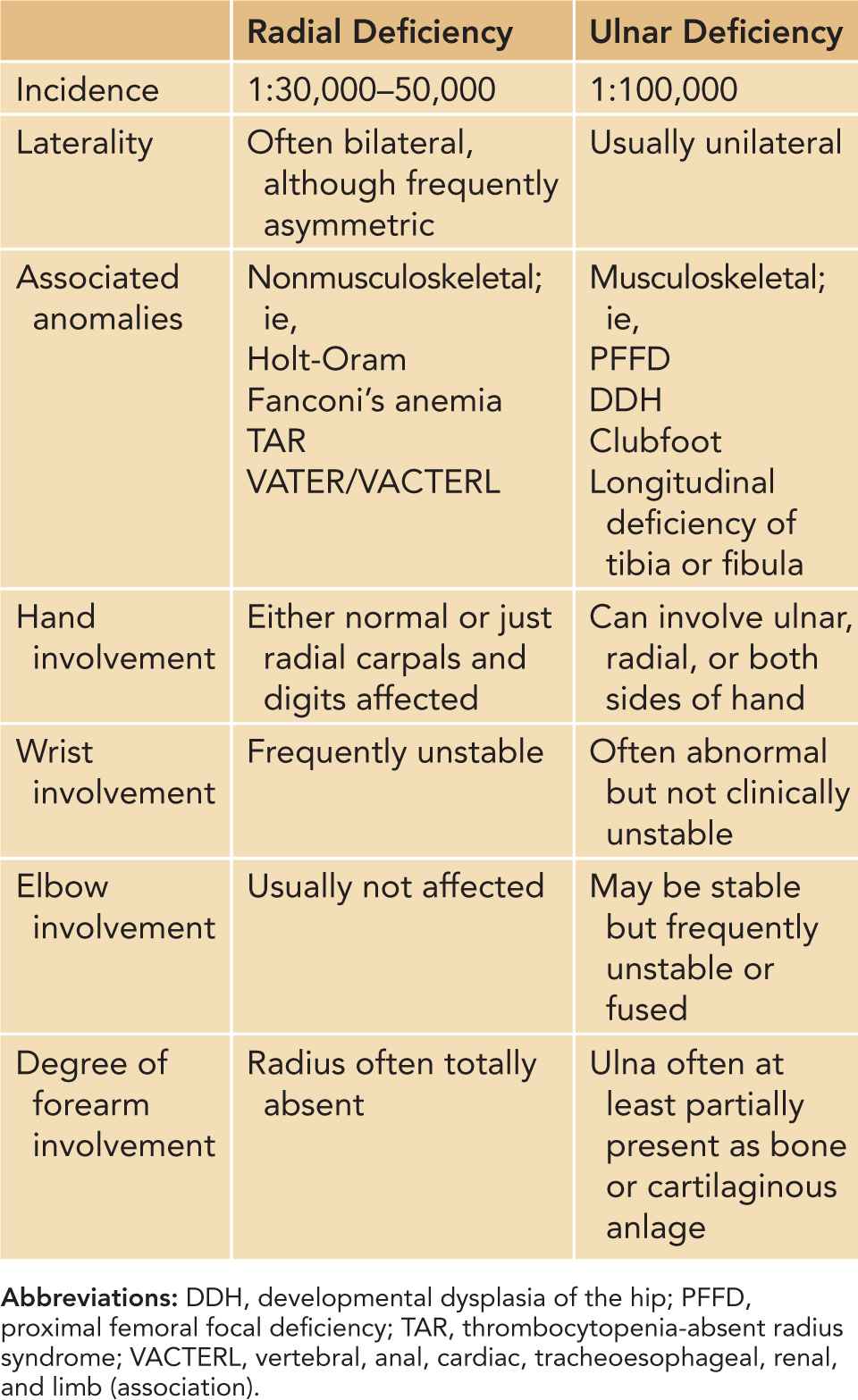
Radial longitudinal deficiency is the more common of the 2 and includes anything from just a slightly hypoplastic thumb on the affected side to a completely absent radius with associated deficiency of the humerus and glenoid. It is frequently bilateral, although often the degree of involvement is asymmetric between sides. When it occurs in isolation, which is only one-third of the time, it is usually a sporadic mutation with no known pattern of inheritance.13 More frequently, radial dysplasia is part of a broader syndrome or condition (Table 64-1), many of whose etiology is slightly better understood.
Holt-Oram syndrome is the association of radial dysplasia and cardiac anomalies, most commonly atrial or ventricular septal defects or conduction abnormalities (which may not present until adulthood); although caused by a spontaneous mutation in TXB5 on chromosome 12 most of the time, it is autosomal dominant with complete penetrance. Fanconi anemia is inherited in an autosomal recessive pattern and is the product of defects in 1 of 11 FANC genes, which code for proteins in a complex involved in DNA repair; patients must have 2 bad copies to be affected, either homozygous for 1 gene or heterozygous for 2. Ninety percent develop pancytopenia at some point, and patients are at risk for malignancy, especially acute myeloid leukemia.
The etiology of thrombocytopenia-absent radius (TAR) syndrome is not well understood, although in some cases it is autosomal recessive. TAR is characterized by an absent radius (as its name would imply) but a relatively normal-appearing thumb and episodic bleeding that often starts in early infancy; it is confirmed by laboratory tests, which demonstrate abnormalities by one week of life in half of patients and by 4 months in almost all.
Finally, VACTERL (vertebral, anal, cardiac, tracheoesophageal, renal, and limb) or VATER (vertebral, anal, tracheoesophageal, and renal anomalies) association is a sporadic cluster of congenital anomalies, including vertebral anomalies, anal atresia, cardiac malformations, tracheoesophageal fistula, renal anomalies, and limb anomalies (most frequently, radial dysplasia); patients must have at least 3 abnormalities to be diagnosed. Although the exact cause is not known, it is thought to be related to a defect in embryonic mesodermal development. Given the frequent association of radial dysplasia with other serious conditions, patients with any sign of radial longitudinal deficiency, including just a hypoplastic thumb, should be thoroughly evaluated for any cardiac, renal, hematopoietic, or other anomalies.
Management of radial longitudinal deficiency depends on the extent of involvement, bilaterality, and so on. Stretching and splinting that begin in early infancy can be helpful in maintaining soft tissue length; surgical correction is focused on not sacrificing function for cosmesis. A patient with a severe-looking wrist deformity but poor elbow motion may rely on his or her significant radial deviation to get his or her hand to mouth so a centralization procedure that improves the appearance of the arm may take away that crucial hand-to-mouth ability.
Ulnar dysplasias are much less common than radial dysplasias by a factor of 3 or more and do not have the same association with other organ system abnormalities. They are, however, more commonly associated with other musculoskeletal anomalies, such as scoliosis, proximal femoral focal deficiency, and fibular deficiency. The exact cause is unknown but likely occurs during the fourth or fifth week of gestation, earlier than for radial deficiencies. Treatment is focused mainly on the hand, as that is where the most function can be gained. Splinting and stretching may be helpful early for maintaining flexibility and motion.
Digit Anomalies
Anomalies of the fingers and thumb are numerous; this chapter touches on polydactyly, syndactyly, and trigger thumb.
Polydactyly (Figure 64-2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



