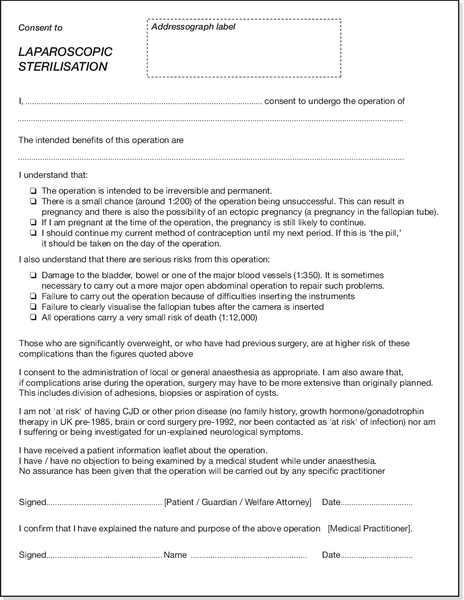
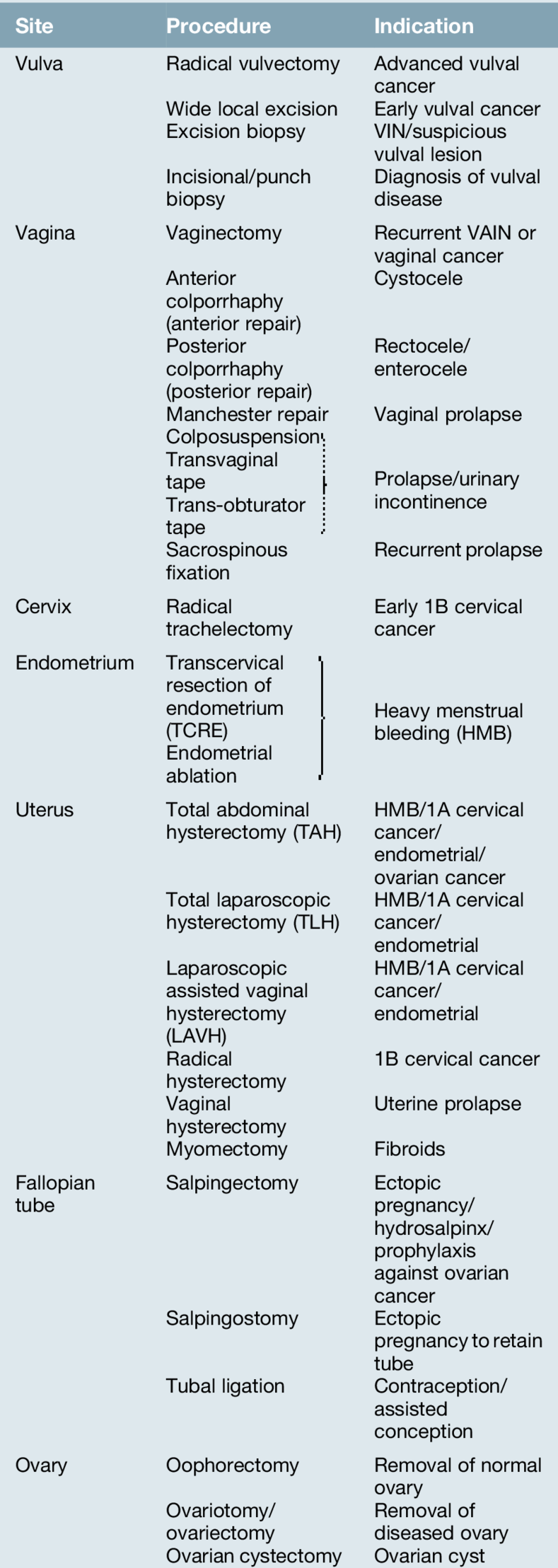
23 The decision to proceed to surgery is one that must be taken with care and responsibility, as life-threatening complications, though rare, can arise after even the most minor of operations. It is therefore essential that the patient has been adequately prepared for the operation, and that consent has been obtained by someone capable of weighing up the risks and the benefits. Careful preoperative counselling will enhance the patient’s experience and, along with good communication, adequate surgical time and continuity of care, maximize the chance of a successful outcome. This chapter will address the issues surrounding good surgical practice in patients undergoing gynaecological procedures. This is usually carried out in an outpatient clinic. The clinical need for surgery may be clear at the outset, but this must be communicated clearly with the patient with adequate time given to ask questions and obtain informed consent. It is good practice to give written information about the intended procedure, as well as contact details to allow the patient to revisit any uncertainties. Ideally, consent forms should be typed for clarity, and should be completed in the clinic and updated on the day of admission. An example of a consent form is shown in Figure 23.1. In the situation where the adult patient’s ability to consent is compromised (e.g. if they have dementia), it is good practice to involve the patient’s family or next of kin; how consent is formally obtained in this situation, will depend on the legal requirements of that country. Risk can be a difficult concept to communicate with a patient, and sensitivity is required to balance a discussion of the serious nature of adverse outcomes in a manner that will not detract from the patient’s confidence in their doctor’s abilities. Trust is the cornerstone of the partnership between doctor and patient, and erosion of this at an early stage, will increase the likelihood of longer-term dissatisfaction. The gynaecologist needs to consider comorbidities of any patient being considered for surgery and general anaesthesia. Are there less invasive and safer alternatives? Examples may include, ring pessaries instead of pelvic floor surgery for prolapse; levo-norgestrel intrauterine system (LNG-IUS) instead of hysterectomy for heavy menstrual bleeding; medical therapy for endometriosis; and implant, vasectomy or LNG-IUS instead of laparoscopic tubal ligation. If surgery is to proceed, comorbidities should be communicated to the anaesthetist to allow satisfactory preparation and to avoid anaesthetic complications. Liaison with other specialties may be helpful to make the postoperative course run smoothly and clear management plans put in place, e.g. with haematology in patients requiring anticoagulation. Gynaecological surgery generally involves removal or repair of the tissues of the female genital tract. In oncological surgery, this will also extend to removal of sites where gynaecological cancer may have spread, for example draining lymph nodes and omentum. Many of the procedures will be discussed in other chapters and therefore, only an overview will be given here. More common gynaecological procedures are listed in Table 23.1. Normal anatomy is shown in Figure 1.11. Recognition of structures at surgery can be quite different from this view, however, as underlying disease processes may disrupt normal anatomy by destroying normal tissue planes (e.g. in endometriosis and malignancy), and make identification of anatomical structures tricky for even the experienced surgeon. Hysterectomy is one operation where the main gynaecological structures are often clearly visible and the principal steps in this procedure will be outlined below. Dissection usually involves a combination of scalpel, scissors and diathermy, but there is increasing use of sealing/cutting devices generated by high frequency oscillation of the instrument’s blade (Harmonic Ace, Ethicon) or bipolar diathermy (Ligasure, Covidien). Options for type of skin incision are as shown in Figure 23.2
Gynaecological surgery
Introduction
Preoperative counselling
Common gynaecological operations
Surgical anatomy
Skin incision
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree