Fig. 4.1
A 4-year-old girl, with posttraumatic tibia valga (Cozen’s phenomenon), treated by stapling. Rigid implants are subject to failure through bending, breakage, or migration, as a result of the inexorable forces of physeal growth. Note the extrusion of her single staple; occurring inexplicably, 9 months following implantation
Frustrated by some of the aforementioned problems with stapling, the concept of using an extra-periosteal, non-locking plate, serving as a tension band, was developed in 2002, and introduced in 2004 [10, 11]. Since then, similar implants have been introduced into the market, worldwide (Fig. 4.2). It is not critical which implant one selects; rather it is the tension band principle that counts. However, one should avoid locking plates because the rigid construct will predispose to implant failure.


Fig. 4.2
Since the introduction of the 8-plate in 2004, many facsimiles have been produced worldwide and used successfully for guided growth. The common denominators for success are low profile and non-locking
In resource-challenged regions of the world, the 8-plate or facsimiles may not be available. In such an environment, an option is to take a 1/3 semi-tubular plate or a pelvic reconstruction plate and cut it into 2-hole segments [12–14]. The potential disadvantages relate to the relative bulkiness or stiffness (will not reverse bend) when compared to the real device. Some favor the use of quad plates (4-hole) in heavy children, particularly with Blount’s disease. Inevitably, a variety of plate shapes have been proposed (step-off, hinge plates, H-plates) and the controversy is unresolved as to whether titanium or stainless steel implants are superior. Unfortunately, there is currently no literature to support or refute these ideas. Suffice it to say that any device that is flexible and permits differential growth can work.
An alternative strategy, popularized by Metaizeau, involves the insertion of large-diameter (6.5 or 7.3 mm) cancellous screws across one or both sides of the physis (percutaneous epiphysiodesis using transphyseal screws, or PETS) [15]. While also minimally invasive, the theoretical objection is the necessity of violating the physis with a large threaded implant. Series reports of PETS are largely confined to the adolescent age group [16]. It has not been described in younger children or in sagittal or oblique plane deformities. Thus, PETS has comparatively narrow ranges of age and applications and its potential reversibility remains in question.
Deformities of the Lower Extremities
General
With the notable exception of physiologic varus and valgus, lower extremity deformities often progress with growth. While angular deformities at the knee are most obvious and perplexing, one must examine the patient for limb length discrepancy, rotational deformities, and ligamentous laxity that represent confounding factors. Also, examine the hip and ankle clinically and, when indicated, radiographically, for coexisting or compensatory angular deformities. If the deformity is unilateral, then the normal leg serves as a comparison. However, oftentimes deformities are bilateral and not necessarily symmetrical. One must be cognizant of remaining growth and the predicted natural history of a given problem. If a deformity is thought to be physiologic or borderline in severity, a follow-up after 6 months may clarify this and affect the timing of intervention. If there is concurrent deformity of the hip and/or ankle, simultaneous guided growth may be employed [17].
Angular: Frontal
Physiologic
It is well recognized that children under the age of two may present with symmetrical and painless bowing of the legs, associated with ligamentous laxity and intoeing. With observation alone, all components of this deformity will spontaneously correct, without treatment. While there is no need for intervention, parental education, reassurance, and periodic follow-up are tantamount to success. Likewise, physiologic genu valgum should be managed expectantly, without bracing, physical therapy, or shoe modification, up until the age of 6. These self-limiting conditions are a contraindication to surgical intervention of any kind [18–20].
Pathologic
In contradistinction to the above-noted problems, the pathologic deformities may be unilateral or bilateral and multilevel. The etiology may be idiopathic, developmental (Blount’s), acquired (Cozen’s), metabolic (rickets), genetic (neurofibromatosis, hereditary multiple exostoses, Schmid dysplasia), or dysplastic (fibrous dysplasia, Ollier’s), to name a few. Deformities may occur in the frontal, sagittal, or oblique plane, compounded by torsion and ligamentous laxity. They are insidious in their progression, and refractory to attempts at orthotic management or physical therapy.
Regardless of the underlying etiology, individually and collectively these deformities constitute the indication for guided growth, as the treatment of choice, instead of osteotomy (salvage procedure). Clinically, genu valgum is often associated with anterior knee pain and a circumduction gait; patellar instability may ensue. It is documented by measuring the intermalleolar distance when standing and prone. Genu varum may also be seen with knee pain and a waddling, Trendelenburg-positive gait, often in association with intoeing, ligamentous laxity, and lateral thrust. Furthermore, when the deformity is unilateral, progressive, relative limb length discrepancy is common.
While knee deformities represent, by far, the most common indication for guided growth, there are specific deformities such as ankle valgus or coxa vara that may also lend themselves to the same principle and technique. Timely guided growth may prevent or forestall the need for distal tibial or proximal femoral osteotomies. In some patients, multilevel guided growth, to simultaneously address concomitant deformities, is efficient and well tolerated [17] (Fig. 4.3).
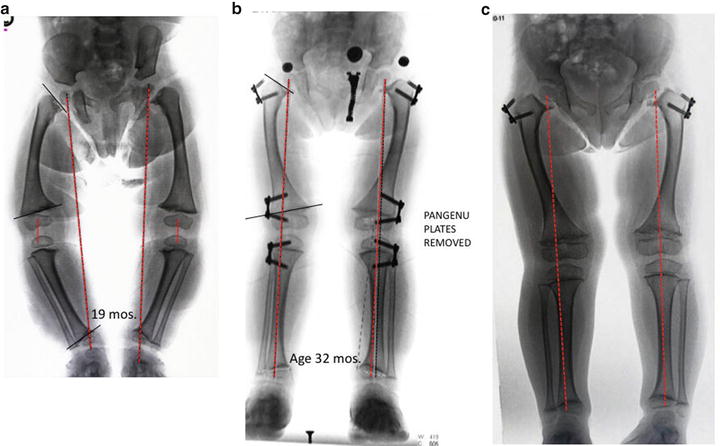
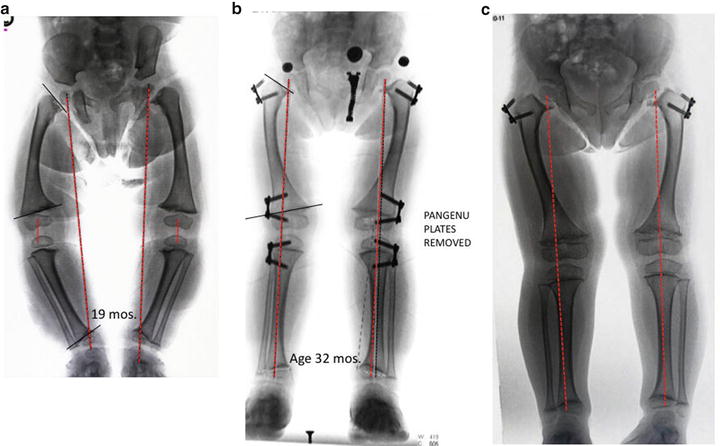
Fig. 4.3
(a) This 19-month-old girl with Schmid-type chondroepiphyseal dysplasia, presented with a waddling gait and hip pain (due to stress fractures of the femoral neck). (b) 13 months following bilateral, 3-level guided growth (outpatient/no cast), her mechanical axis neutral; her gait has become normal and hip pain abated. (c) At age 6, she remains asymptomatic, with neutral alignment. Note the indirect resolution of her ankle varus. Her femoral neck fractures remain healed; the plates will be left in situ, pending further growth. Proximal femoral osteotomies appear to be unlikely
Treatment
Timing/Angular
When dealing with progressive angular deformities, the previously preferred method of epiphysiodesis—now largely of historic interest—involved permanent arrest by either open [1] or percutaneous techniques [21, 22]. These required serial scanograms and bone age determinations with calculations using various methods [23–25]. Guided growth with tension band plates is more forgiving in terms of timing and calculations. On a standing AP teleroentgenogram, the relative limb lengths and mechanical axis are documented. The latter normally will bisect the horizontal knee at an 87 degree angle. The mechanical axis should fall within the center two quadrants (zones +/− 1) of the knee (Fig. 4.4). When it is in medial or lateral 2 or 3, surgical intervention is generally warranted. If two levels of deformity, for example femur + tibia, are identified, then pan genu guided growth is indicated, in order to preserve a horizontal knee joint line.


Fig. 4.4
The mechanical axis (dotted red line) comprises a vertical line connecting the center of the femoral head to the center of the ankle; normally, this bisects the knee. If you divide the knee into quadrants, medial zones (−) 1–3 reflect increasing varus and lateral zones (+) constitute valgus. While zone 1 may warrant observation, zones 2 or 3 call for treatment, in order to protect the physes and the knee
In children older than 10, the anatomic angles, as codified by Paley and Sabharwal et al. (Table 4.1), can be useful to monitor during correction; these reference joint/shaft orientation for the femur and tibia [26, 27]. The joint congruence angle is typically 0° (parallel lines), indicating ligamentous balance/integrity. There may be concomitant deformity in both the femur and tibia. By envisioning the knee joint horizontally, one can readily detect multilevel deformities. For example, in patients with Blount’s disease, there may be concomitant varus or valgus deformity of the distal femur that must be taken into account [26].
Abbreviation | Anatomic angles | Degrees |
|---|---|---|
MPFA | Medial proximal femoral angle | 90 |
LDFA | Lateral distal femoral angle | 81 |
PMTA | Medial proximal tibial angle | 87 |
LDTA | Lateral distal tibial angle | 87 |
PPTA | Posterior proximal tibial angle | 81 |
PDTA | Posterior distal tibial angle | 90 |
JCA | Joint congruence angle | 0–3 Apex medial |
To benefit from guided growth, the age of the patient is not critical, provided that there is at least a year of predicted growth remaining. Guided growth has been safely and successfully utilized in patients ranging from 18 months to 18 years in chronologic age. The latter figure reflects the delayed/prolonged growth observed in some children with neurologic delays or metabolic syndromes. Commencing as young as age 4, patients with progressive or symptomatic deformity (such as Klippel-Trenaunay-Weber, Beckwith-Wiedemann, neurofibromatosis), it may be preferable to correct the problem, even if it requires repeated guided growth subsequently, rather than trying for perfect timing or resorting to osteotomy. The risks of delaying surgical realignment include compensatory deformity of the hip, knee, or ankle, ligamentous laxity, and patellar instability.
Technique/Angular
Under tourniquet control, the designated physis is approached, through a 3-cm incision. The dissection is deepened through fascial and submuscular planes, down to the bone, preserving the periosteum. A Keith needle is inserted into the physis, checking its position in the frontal and sagittal planes, with the fluoroscope. The plate is then inserted, placing the small center hole over the Keith needle to align it with the physis. It is desirable to position the plate midsagitally, unless an oblique plane deformity is being corrected. For example, a knee flexion/ varus deformity may call for a single anterolateral tension band plate. One plate per physis is usually sufficient. The smooth 1.6-mm guide pins are inserted; they need not be parallel, but must avoid the physis and joint. Each hole is predrilled to a depth of 5 mm in order to facilitate advancement of the 4.5-mm cannulated screws, without undue torque.
While screw length is arbitrary, and sizes may be mixed, the longest practical screw is usually recommended. Each is inserted to be snug with the plate. It is then important to remove the guide pins, which may be binding on the screw, and further tighten each screw to countersink within the plate. This should be documented fluoroscopically. This critical maneuver will avoid 3-point bending stresses, reported in some patients with Blount’s disease, which could produce stress fracture of the screw. This is a potential technical error that may compromise any screw, be it titanium or stainless steel, cannulated or solid. Once the hardware is secured, the wound is closed in layers and a soft dressing applied. Most patients are discharged from same-day surgery with (optional) crutches. Full weight-bearing and activities are encouraged as tolerated.
Follow-Up
Routine follow-up is recommended every 3 months (for angle) or every 6 months (for length) until correction is achieved (Fig. 4.5). For angular correction, most deformities will be resolved within 12–18 months. Certain syndromes and bone dysplasias such as achondroplasia may require more time. There is no proven limit as to how long one can safely restrict one side of the physis. Since growth is unabated by the presence of a unilateral flexible tether, premature physeal closure is unlikely. Clinical correction is corroborated by full-length, weight-bearing teleroentgenogram, noting limb lengths and the mechanical axis. In children younger than 10, or with delay in skeletal maturity, it may be advisable to allow slight overcorrection of the mechanical axis into medial or lateral zone 1. In the event of rebound/recurrent deformity, the process may be repeated. Once the screws have reached maximum divergence, the narrow waist of the plate accommodates reverse bending of the plate, facilitating further correction. This characteristic may not be shared by the more rigid quad plates.
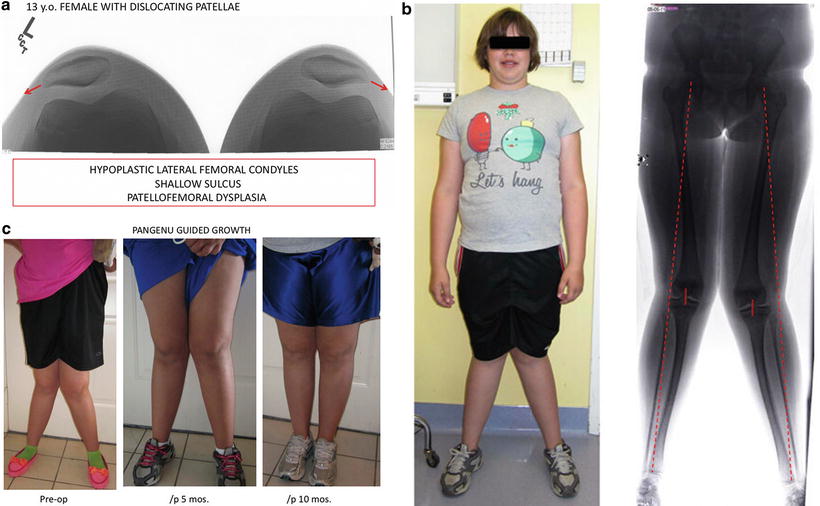
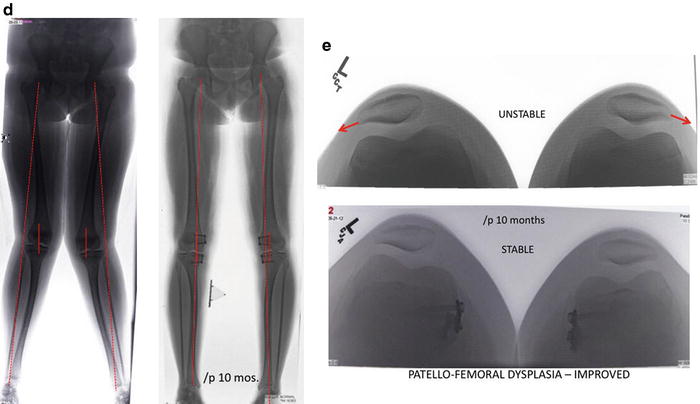
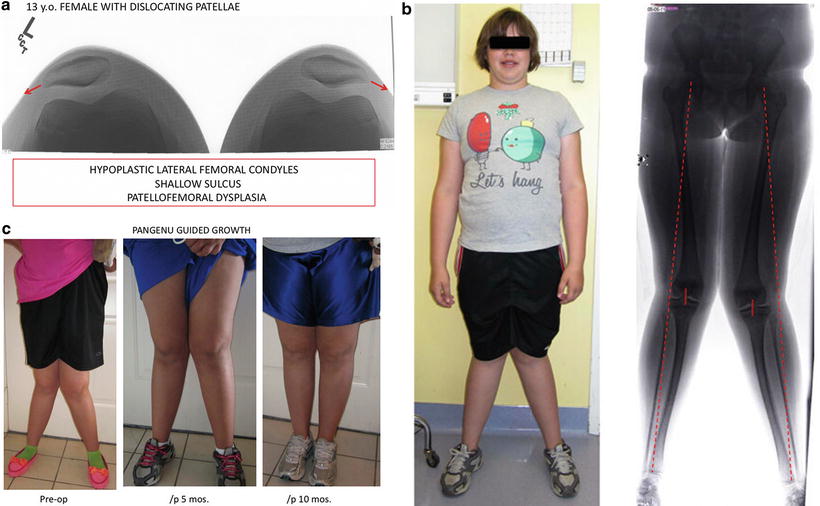
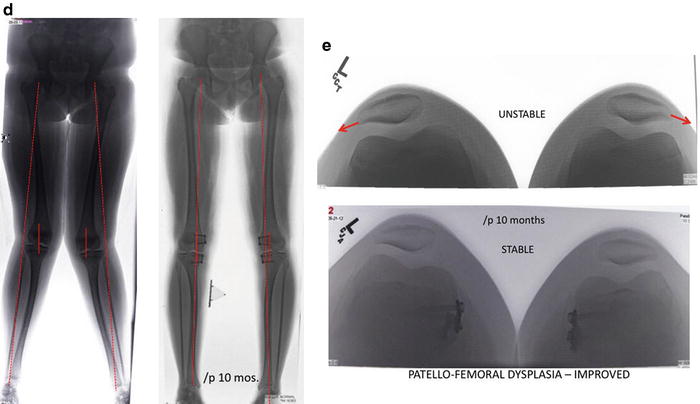
Fig. 4.5
(a) This 13-year-old girl presented with “patellofemoral dysplasia” manifest by bilateral patellar instability. (b) Clinically, her intermalleolar distance measured 20 cm. Her mechanical axis is lateral zone 3. It was apparent that idiopathic genu valgum (femur + tibia) was the proximate cause of her patellar dislocations and recognized that an MPFL reconstruction or patellar tendon transfer would not suffice to solve her problems. (c) Having hit her adolescent growth spurt, her deformities completely corrected within 10 months of pangenu plate application and her patellae stabilized, without direct intervention. (d) Radiographic comparison of before vs. 10 months after pangenu guided growth, whereupon the plates were removed. (e) “Sunrise” radiographs demonstrating improvement in the patellofemoral sulcus depth, presumably as a consequence of normalizing the mechanical axis and directing the patella in front of the femur
Angular: Sagittal/Oblique
Knee
Fixed knee flexion deformity (FKFD) may be associated with conditions including cerebral palsy, spina bifida, and arthrogryposis. It is important to differentiate between dynamic and fixed contracture, because the treatment is very different. Both conditions will limit the straight leg raise; with the former, the popliteal angle will change as the hip is flexed in the supine position. In addition to the typical supine straight leg raise, it is helpful to examine the patient prone, with the hip extended, relaxing the hamstrings. If the knee remains flexed and the foot does not reach the table, this indicates a fixed rather than dynamic knee deformity that will not respond to hamstring recession (Fig. 4.6).
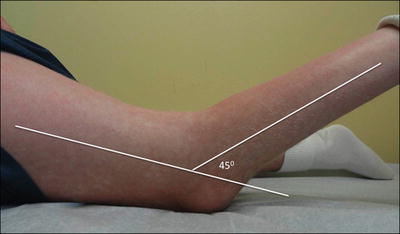
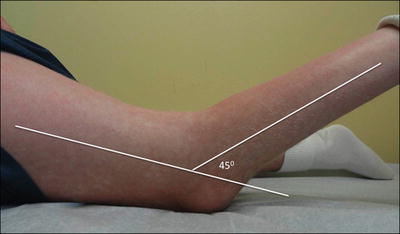
Fig. 4.6




Examination in the prone position places the hip in maximum extension, thereby eliminating the hamstrings as a source of deformity. With fixed knee flexion deformity (45° shown here) the ankle does not rest on the table. A hamstring recession will not resolve this deformity. An extension osteotomy may be averted with guided growth of the anterior distal femur
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


