Fig. 7.1
Severe deformity. A patient with pseudopseudohypoparathyroidism (pseudoPHP) with complex, multiplanar and multiapical deformities of both lower extremities using the Ilizarov technique and the Taylor Spatial Frame™. This case demonstrates the possibility through gradual correction to correct very severe deformity. (a) Preoperative clinical and radiographic view. (b) During correction. (c) After one side is completed. (d) Final result
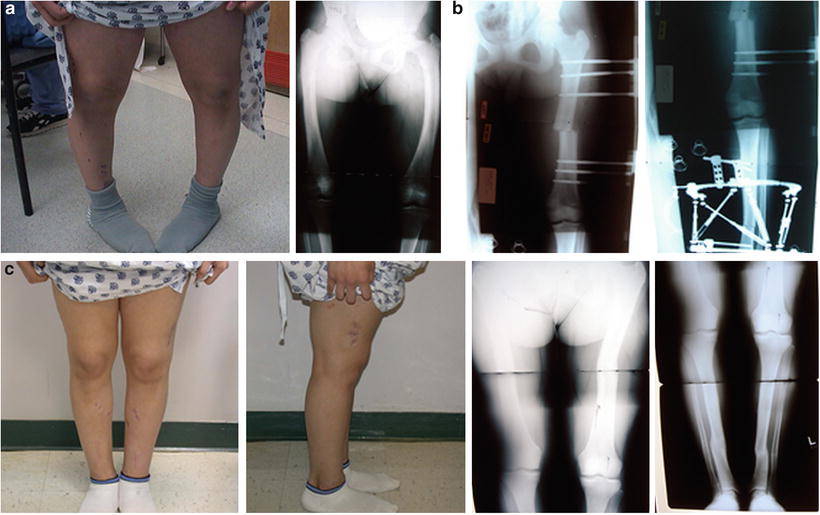
Fig. 7.2
In the case of hypophosphatemic rickets with a multiapical deformity and rotational deformities of the tibia and fibula, a femoral deformity resolved to one location and was corrected acutely while the tibial and fibular rotational deformities were gradually corrected with the use of a circular external fixation device. (a) Preoperative clinical and radiographic view. (b) During correction. (c) Final result
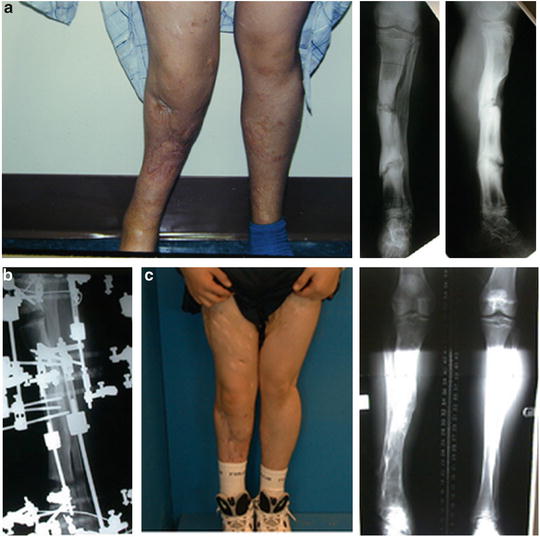
Fig. 7.3
Translation and angular deformity—This deformity of infected non-unions demonstrates a case in which the translational deformity cannot be corrected at the site of deformity due to poor soft tissue and a single vessel leg. This translational deformity is corrected by two angular osteotomies away from the site of the deformity. (a) Preoperative clinical and radiographic view. (b) During correction. (c) Final result
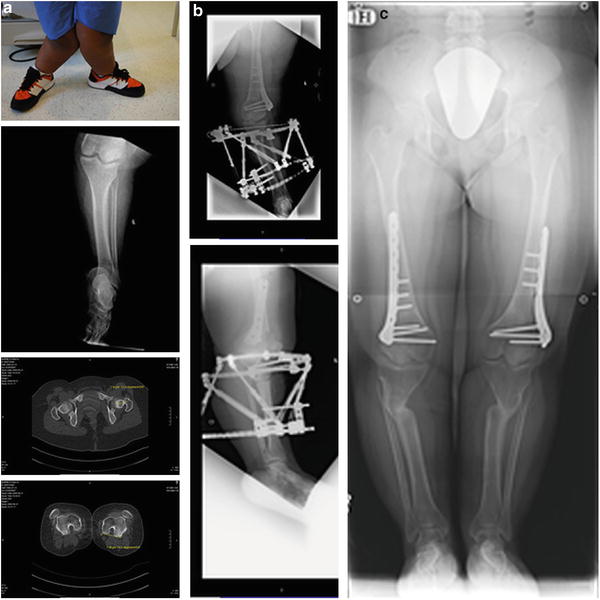
Fig. 7.4
In a patient with Ellis–van Creveld disease with femoral retroversion and tibial angular deformity, deformity correction was performed via an extra-articular osteotomy of the femur with derotation and gradual correction of the tibial angular deformity with external fixation. Note the initial patellar dislocation was reduced once the rotational deformity was corrected. (a) Preoperative clinical and radiographic view. (b) During correction. (c) Final result
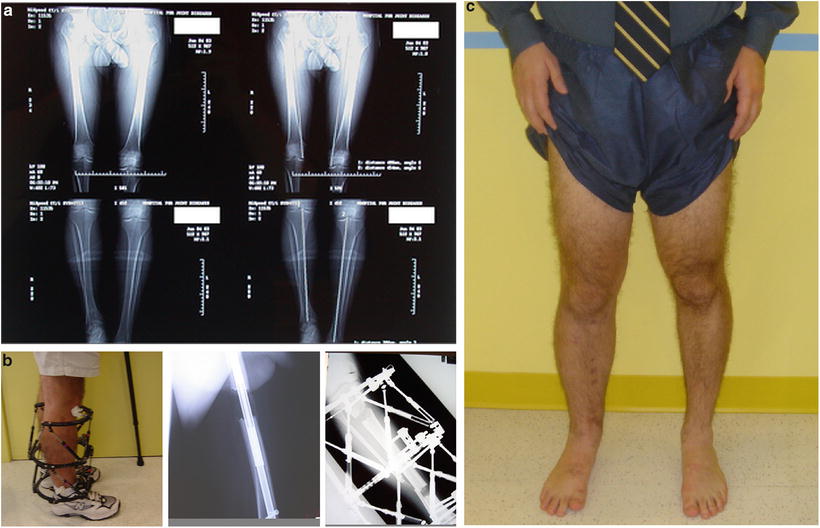
Fig. 7.5
Deformity correction with limb length inequality. This case demonstrates tibial varus and femoral rotation concurrent with length inequality of both bones. An acute derotational osteotomy of the femur and bifocal osteotomy of the tibia were performed. Deformity correction and lengthening of the tibia were achieved using a hexapod external fixation device. (a) Preoperative radiographic view. (b) Clinical and radiographic view during correction. (c) Final result
Blount disease, a condition ideally suited for gradual correction, is an oblique plane (anterolateral) deformity of the proximal tibia that presents in young children and adolescents (see Fig. 7.6). The deformity is often at the level of or close to the proximal tibial physis and may be associated with internal tibial torsion [15, 16]. Historically, the operative correction of Blount disease was associated with malunions and delayed unions as well as compartment syndrome and nerve injury (most commonly the nerve to the extensor hallucis longus). Many of these complications can be minimized with gradual correction [17, 22]. Compartment syndrome occurs either due to swelling in the compartment obstructing venous return or compression or injury to the anterior tibial artery as it transverses the interosseous membrane. Both of these etiologies, i.e., swelling and injury to the artery, are much less common with gradual correction. Rarely are prophylactic fasciotomies required in gradual correction.


Fig. 7.6
Angular deformity. This is a case of untreated Blount disease in an adult. To elevate and restore the joint line, an intra-articular osteotomy was performed. The deformity was then gradually corrected using a hexapod external fixation device. (a) Preoperative clinical and radiographic view. (b) During correction. (c) Final result
Box 7.4
There are many clinical uses for gradual correction.
Protection of nerve function and the soft tissue envelop are key components to gradual correction.
Analysis of Deformity
Planning for deformity correction follows the same principles whether performing a gradual or an acute correction. One must analyze the axes in the coronal, transverse and in the sagittal planes [18, 19], identify the apex of each deformity, plan the level of the osteotomy (or osteotomies), and decide on the surgical technique and hardware to be used. In addition to analyzing the axes and determining the degree and location of the deformity, the patient’s age and remaining growth are also important factors. Patients that are still growing can typically benefit from growth modulation procedures particularly when the deformity is close to the joint (refer to Chap. 4 for more details) [20]. To ensure accurate correction of a deformity of the lower limb, both the individual features of the bone being osteotomized and the limb as a whole must be understood. The overall alignment of the extremity, the alignment of the tibia and femur independently, the joint alignment (laxity), and rotational deformity require evaluation (refer to Chaps. 2 and 3 for more details).
Of the many factors that affect bone healing, the quality of the underlying bone is perhaps the most important [21] and should be the first step in assessing the deformity. The potential to heal dictates the success of the procedure, the extent of fixation needed, and the possibility of hardware failure. The ability of a bone to heal differs substantially between various conditions (Figs. 7.7 and 7.8). For instance, in multiple enchondromatosis, the bone has a higher neoplastic potential when compared to normal bone and may heal at a slower rate (see Fig. 7.7) [22]. Osteogenesis imperfecta is an example in which the bone density and architecture is weak [23], making it more difficult to maintain alignment without supplemental measures such as preoperative bisphosphonates and the use of an intramedullary device instead of an external fixator.
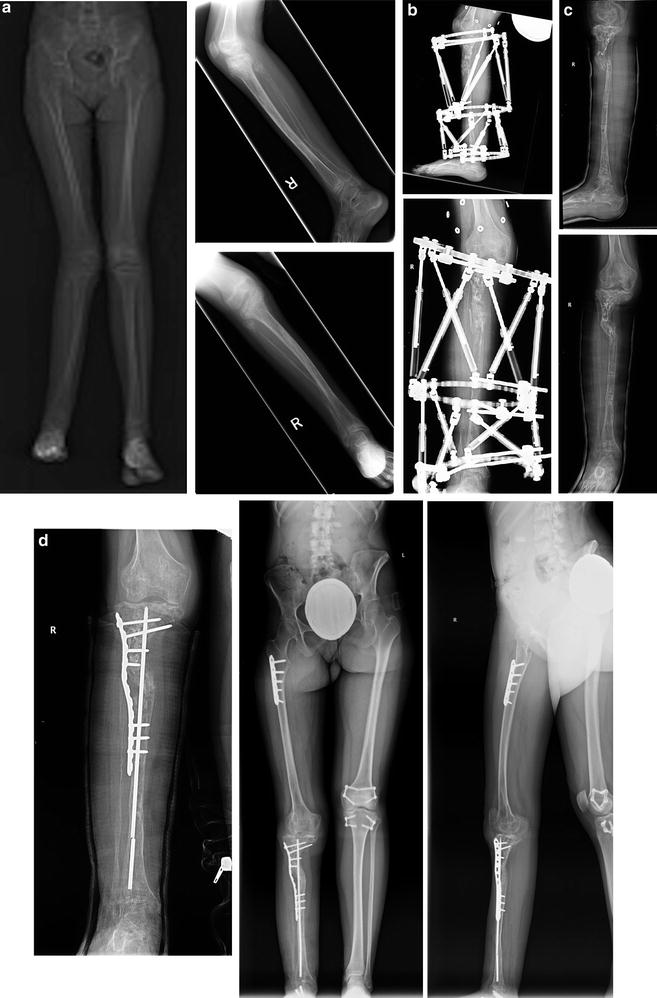
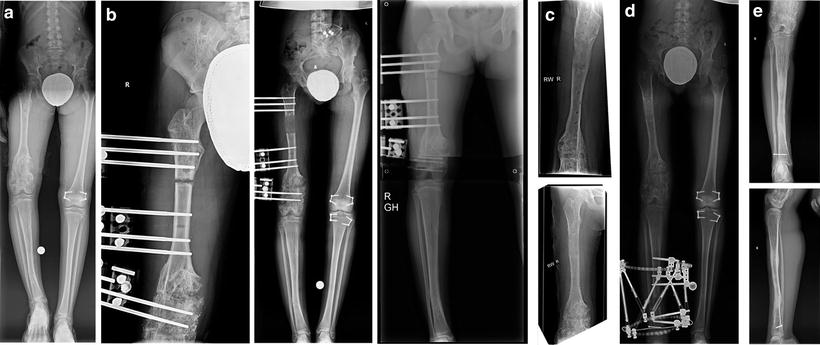
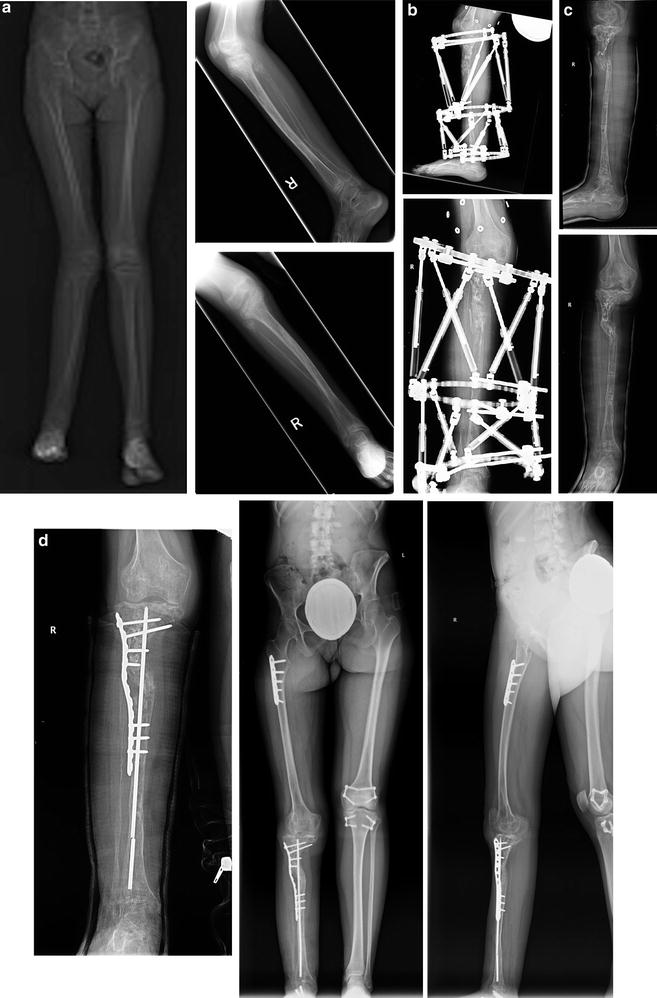
Fig. 7.7
Poor regenerate secondary to an underlying condition. An 11-year-old patient with hemangiomatosis and tibial bowing underwent deformity correction with hexapod external fixation. Hemangiomatosis prevented proper healing of the osteotomized bone, which necessitated stabilization of the bone internally with a rush rod and locking plate. (a) Preoperative radiographic view. (b) During correction. (c) Delayed union. (d) Final result
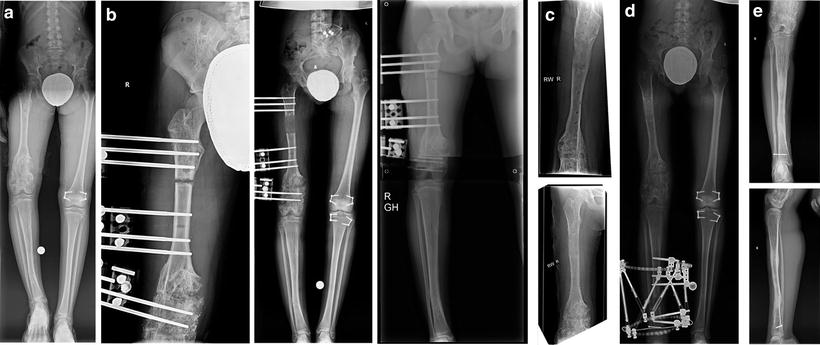
Fig. 7.8
Delayed healing secondary to underlying condition. This case demonstrates deformity correction and lengthening in the setting of Ollier’s disease. The patient had limb length inequality and varus deformity and underwent lengthening of the femur proximally with a monolateral fixator and deformity correction of the distal femur with the same monolateral frame. The tibial deformity was treated with a hexapod fixation device. The patient underwent simultaneous growth modulation on the contralateral side. (a) Preoperative radiographic view. (b) During lengthening. (c) Femur after femoral lengthening and deformity correction. (d) During tibial deformity correction. (e) Final result, tibia
The deformity must be quantified and should be analyzed on the anteroposterior (AP) and lateral radiographs. Varus or valgus angulation and the medial or lateral translation are measured on the AP view. Procurvatum or recurvatum and anterior or posterior translation are measured on the lateral radiographs. Rotational alignment is measured clinically using the thigh-foot axis with the patient in prone and if necessary may be supplemented with a CT scan or MRI. Length is measured using a standing full-length lower extremity radiograph. To quantify the deformity, mechanical axis deviation (MAD) and joint laxity, a standing patella forward full-length AP and lateral radiograph of both lower limbs are used [2]. Femoral and tibial deformities are further quantified on patella forward AP and lateral views of the individual long bones. In the case of the very young child with unossified epiphyses, an intraoperative knee arthrogram may be performed to outline the femoral condyles and tibial plateau to more accurately assess the deformity present in the tibia and/or femur (refer to Chap. 2 for more details).
Box 7.5
Thorough analysis of the deformity including an assessment of the quality of the bone is essential prior to gradual correction.
A thorough clinical exam and standardization of imaging studies allows for accurate deformity analysis.
Planning the Osteotomy
Determining the level of the osteotomy is an integral part of the presurgical plan. Ideally the osteotomy should be located at the apex of the deformity. At times, the osteotomy cannot be performed at the apex of the deformity due to the proximity of the joint, the physis, or compromised surrounding soft tissues. These issues necessitate moving the osteotomy away from the apex. For example in Blount disease, the apex is usually in proximity to the knee joint or the proximal tibial physis, making it impractical both to osteotomize in these areas and to safely obtain satisfactory fixation at the osteotomy site. Additionally, one must avoid performing the osteotomy proximal to the tibial tubercle since this may lead to patella tracking problems and injury to the tibial physis [24]. However, performing the osteotomy away from the apex has its consequences. Translation of the bone is necessary in such cases in order to restore the normal mechanical axis and allow the joint lines to remain parallel to the floor. The further the osteotomy is from the apex of the deformity, the larger the magnitude of the required translation. Additionally, it is necessary to keep in mind that gradual translational correction always begins with distraction. As long as the surgeon accounts for these factors preoperatively, they should not prove problematic.
The anticipated outcome of deformity correction is a normal mechanical axis without oblique joint lines (Fig. 7.9). In most cases, the need to have a straight bone is less important than having a corrected mechanical axis (see Fig. 7.1). Exceptions to this are the cases of metabolic bone diseases, such as hypophosphatemic rickets (see Fig. 7.2) or osteogenesis imperfecta in which a straight bone is often necessary for proper healing and the avoidance of later stress fractures.
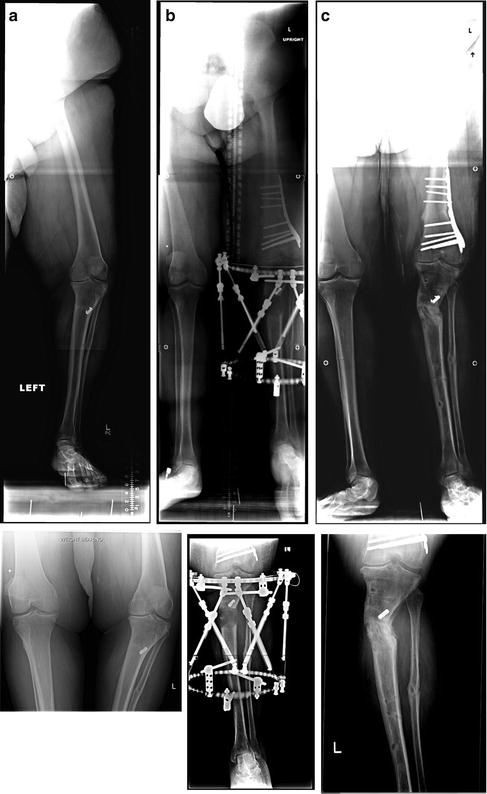
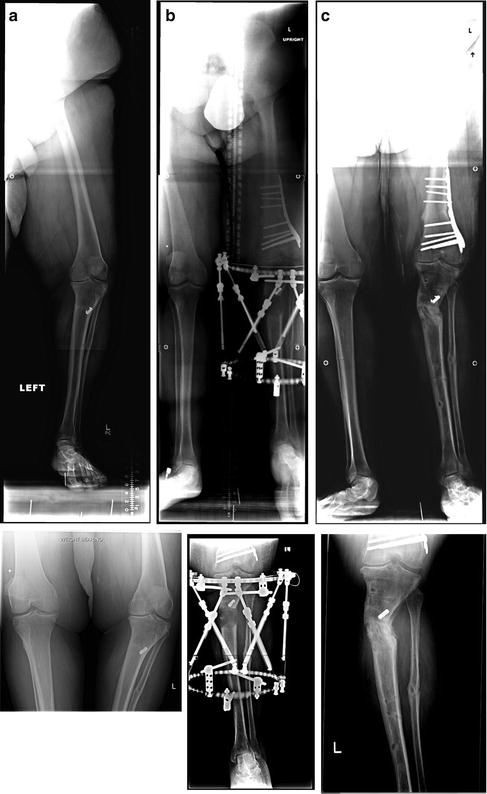
Fig. 7.9
Surgical correction at the location of the deformity, i.e., tibia or femur, is essential. This patient initially presented with 20° of femoral varus and a near normal tibia. The patient’s varus was surgically corrected by 10° via a distal femoral osteotomy, leaving 10° of varus unaddressed. The patient then underwent a tibial osteotomy with external hexapod fixation in an attempt to address the remaining varus deformity. This resulted in a corrected mechanical axis but a valgus deformity in the proximal tibia and created oblique joints of the knee and ankle. The patient’s resultant MPTA was 103° (15° of valgus) and aLDFA 94° (13° of varus). This oblique joint line creates sheer stress in the joints involved. The patient now has pain in his ankle and knee that will require a revision osteotomy. (a) Preoperative radiographic view. (b) During deformity correction. (c) Final result with oblique knee and ankle joints with pain. This osteotomy will require a revision
Box 7.6
Factors affecting the location of the osteotomy include the etiology and the location of the deformity.
Bone quality may affect the osteotomy location and the type of fixation utilized.
Devices
Many techniques and various types of fixation devices can be utilized once the preoperative planning phase has been completed. External fixation remains the gold standard for gradual deformity correction as it allows easy and accessible postoperative manipulation of the deformity. Both circular and monolateral options exist. Many circular systems utilize the principle of the hexapod fixator in which there are two rings: a fixed reference ring and a mobile ring (see Figs. 7.1, 7.2, 7.3, 7.4, 7.5, 7.6, 7.10, 7.11, and 7.12). This configuration allows for a three-dimensional movement of the mobile ring relative to the reference ring. The final configuration is the result of a combination of many uniplanar movements namely anterior–posterior translation, medial–lateral translation, and internal–external rotation. It is simply many vectors adding up over time to give the final vector correction, which is the desired orientation of the distal fragment [2]. Many hexapod systems are available including the Eisenberg fixator™, the Ortho-SUV™, the Smart Correction™, the Spider Frame™, the TL-Hex™ and the Taylor Spatial Frame™. These devices can be utilized to correct deformity not only of the tibia [2] or femur [25] but of the foot [26, 27] and upper extremity as well.




