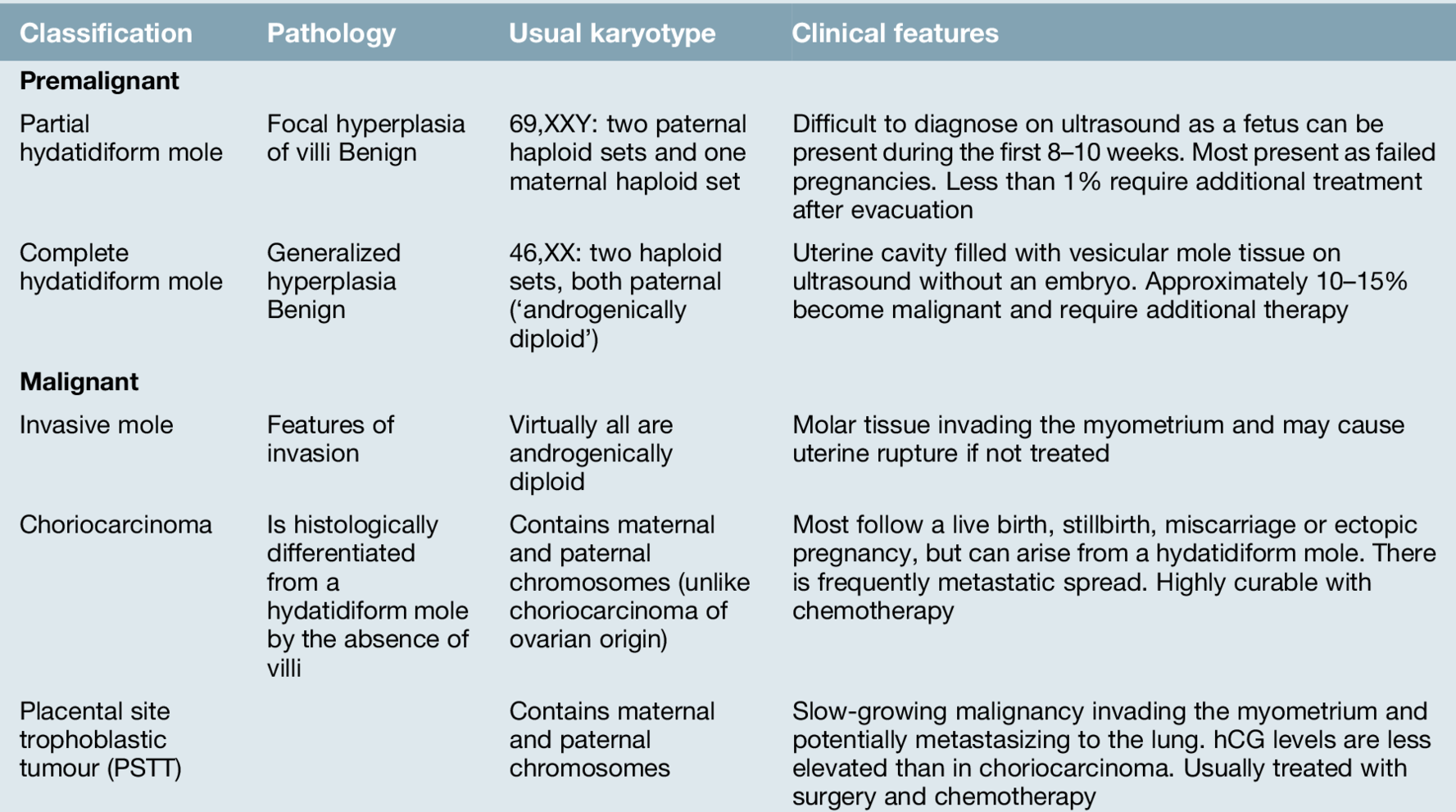
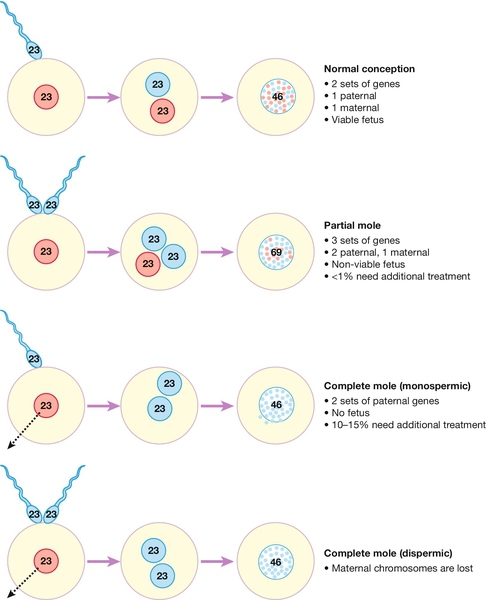
21 Trophoblast cells in health and disease Management of molar pregnancies Follow-up after a molar pregnancy Gestational trophoblastic disease (GTD) forms a group of conditions characterized by abnormal proliferation of trophoblastic tissue with hCG production. There are premalignant and malignant forms: the premalignant form is subdivided into partial and complete hydatidiform moles, and the malignant form into invasive moles, choriocarcinoma, and placental site trophoblastic tumours (Table 21.1). The malignant forms of GTD have a number of important differences from other more common forms of malignancy in terms of aetiology, genetic make-up, pathophysiology and responsiveness to treatment. Fortunately, the malignant forms of trophoblast disease are extremely sensitive to chemotherapy, and treatment routinely results in cure, even in patients presenting with widespread disease. Even molar pregnancy, which is the most common form of GTD, is a relatively rare condition, with an estimated worldwide incidence of around 1–3 cases for every 1000 live births. The incidence has previously been thought to vary significantly across different geographical regions and racial groups, with estimates from the 1960s showing a near 10-fold higher incidence in Korea, the Philippines and China compared with Europe and the USA. More recent data, however, shows that rates of 1–3 cases per 1000 are reported in nearly every worldwide series. The incidence of molar pregnancies is higher at the extremes of reproductive age, at approximately 1 in 30 in those aged under 15 and as high as 1 in 5 in those for women in their late 40s or early 50s. As these extremes of the reproductive age group make up only a very small proportion of the women who become pregnant, over 90% of cases occur in women aged 18–40. In view of the rarity of the condition, ongoing management of trophoblast after the initial uterine evacuation is best provided by a specialist centre. In a healthy pregnancy, the trophoblast cells make up a key component of the placental tissue. Their role is to promote invasion of the conceptus into the lining of the uterus, invade into the uterine blood vessels, promote angiogenesis and produce human chorionic gonadotrophin (hCG). The malignant forms of GTD, both those arising from molar pregnancies and those arising from malignant transformation of cells in healthy placentae, share many of these characteristics. In addition to the abilities to invade into the lining of the uterus and stimulate new blood vessels, the malignant cells are also able to spread to other organs of the body and grow at a very fast rate, without any control on their division. Fortunately, despite these changes, the production of hCG is always retained, and this is extremely helpful in establishing a diagnosis and in monitoring the response to treatment. Premalignant GTD (Table 21.1) is divided into partial and complete molar pregnancies. The original derivation of the term hydatidiform mole, from the Greek hydatis meaning a watery vesicle and the Latin mola meaning a shapeless mass, is an accurate description of the appearance of a complete molar pregnancy evacuated after the first trimester. With the near-universal use of first trimester ultrasound, however, this florid appearance is now rarely seen in well-resourced countries. Molar pregnancies occur as the result of an error in either the production of the oocyte or at the time of fertilization. Normally, fertilization combines a 23,X set of haploid chromosomes from the ovum with either a 23,X or 23,Y haploid set from the sperm, the result being a diploid 46,XX or 46,XY zygote which has the correct balance of maternal and paternal genes. In contrast, a partial molar pregnancy has 69 chromosomes, 23 from the mother and the other 46 paternally derived, usually from the entry of two separate sperm into the ovum (Fig. 21.1). In a partial molar pregnancy, there is usually an embryo which may be seen on an early ultrasound. The ultrasound may have been ‘routine’, or have been carried out because of vaginal bleeding, vaginal discharge, abdominal pain or excessive morning sickness. Although structurally abnormal, there may be no obvious ultrasound features of this in the early first trimester and the diagnosis may therefore not become apparent until histological tissue examination is carried out after a failed pregnancy. The features are of focal hyperplasia and swelling of the villi, though many areas do not have these obvious changes and distinguishing a partial mole from a hydropic miscarriage can be difficult. Fortunately, the risk of malignant change after a partial molar pregnancy is less than 1%, and very few partial mole patients require chemotherapy. In contrast to partial molar pregnancies, complete molar pregnancies have the correct number of chromosomes, with the majority having a 46,XX karyotype. In complete molar pregnancies, however, all the genetic material is from the father and they are therefore termed androgenetic in origin. There appears to be two mechanisms by which this genetic combination arises:
Gestational trophoblastic disease
Introduction
Trophoblast cells in health and disease
Premalignant GTD
Partial hydatidiform mole
Complete hydatidiform mole
![]() the maternal 23,X haploid set of chromosomes in the ovum may be lost at the time of fertilization and the 23,X haploid paternal chromosomes from the fertilizing sperm may duplicate themselves, giving rise to the 46,XX cell
the maternal 23,X haploid set of chromosomes in the ovum may be lost at the time of fertilization and the 23,X haploid paternal chromosomes from the fertilizing sperm may duplicate themselves, giving rise to the 46,XX cell
![]() alternatively, an ‘empty’ ovum may be fertilized by two separate spermatozoa (dispermy), which also leads to a paternally derived karyotype.
alternatively, an ‘empty’ ovum may be fertilized by two separate spermatozoa (dispermy), which also leads to a paternally derived karyotype.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree