(1)
Department of Pediatric Urology, Children’s Medical Center, Dallas, TX, USA
(2)
Department of Urology, Pediatric Urology Research, Children’s Medical Center, Dallas, TX, USA
Abstract
Many children require cystourethroscopy to diagnose, characterize, or treat their genitourinary disorder. Several diseases or anomalies are best treated by cystoscopic minimally invasive means, including posterior urethral valves, ureteroceles, vesicoureteral reflux, urethral stricture/fistula/diverticulum, hematuria, urinary stones, tumors, or other rare birth defects. In this chapter, preoperative, operative, and postoperative techniques and tips of cystourethroscopy are discussed, highlighting its versatility.
Keywords
CystoscopyCystourethroscopyPediatricInfantGenitourinaryAnomaliesAs a form of minimally invasive surgery, endoscopy of the lower genitourinary tract of the pediatric patient can achieve diagnostic and therapeutic goals for a broad range of pathological entities. Advances in instrumentation have permitted endoscopic treatment of even premature infants and in utero fetal surgery [1]. This chapter focuses on general principles of pediatric cystourethroscopy. The reader is referred to other chapters in this text for more detailed discussions of the management of other clinical entities.
Indications and Contraindications
Recurrent urinary tract infections (UTIs), urinary incontinence, obstructive uropathy, urosepsis, and radiological anomalies are the usual indications for lower tract endoscopy. Although many diagnoses are made before cystoscopy by using ultrasound, cystourethrography, CT scan, nuclear scan, IVP, and/or MRI, many pediatric cases require further delineation of the anatomy and physiology by endourological techniques. Cystoscopy followed by transurethral incision of posterior urethral valves for obstructive uropathy [2, 4, 5] is a common indication (Fig. 21.1). Similarly, transurethral incision of ureterocele(s) for outlet obstruction or urosepsis [3] is another clear-cut indication (Fig. 21.2), while prophylactic intervention after prenatal detection is more debated. Cystoscopically guided ureteral or bladder neck injection of bulking agents is frequently employed to treat vesicoureteral reflux (VUR) and urinary incontinence, respectively (see Chaps. 22 and 23). Some surgeons recommend routine cystoscopy before open ureteral reimplantation to assess for the configuration of a prior refluxing ureter, missed ureteral duplication (Fig. 21.3), or cystitis, which would cancel the open surgery. Male urinary incontinence should be evaluated cystoscopically after hypospadias repair or abnormal retrograde urethrogram, assessing for urethral stricture (Fig. 21.4), urethral duplication (Fig. 21.5), or urethrocutaneous fistula. In rare cases, gross hematuria in the pediatric patient may warrant study after a thorough negative medical and radiological evaluation. If clot retention occurs, clot evacuation can be achieved cystoscopically with the instillation of therapeutic agents if indicated. Cystourethroscopy can serve the purpose of ureteral access for retrograde or antegrade upper tract imaging and lithotripsy techniques; however, a trial of medical therapy is warranted because many stones pass in children. Retrograde placement of an occlusion balloon at the ureteropelvic junction can prevent antegrade migration of stone fragments during percutaneous nephrolithotripsy. Retrograde ureteral stenting may be useful at the time of extensive tumor resection or at the time of laparoscopic pyeloplasty. Bladder stones can be endoscopically removed or fragmented via urethra, appendicovesicostomy, or percutaneous cystostomy approaches. At the time of cystoscopy in the child with an open bladder neck due to epispadias (Fig. 21.6) or classic bladder exstrophy, a ballooned catheter can be used for cystography to measure bladder capacity under anesthesia and assess for vesicoureteral reflux.

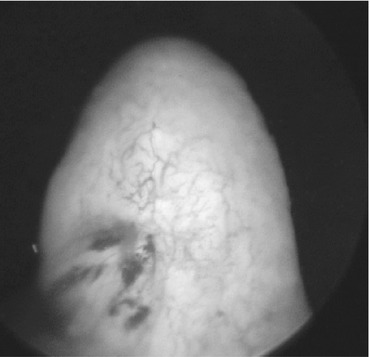
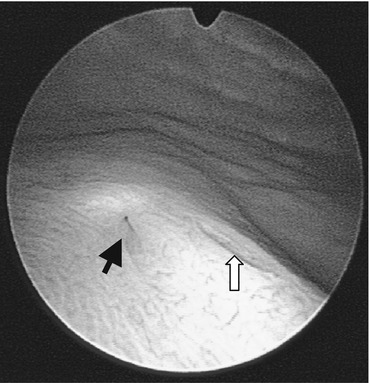
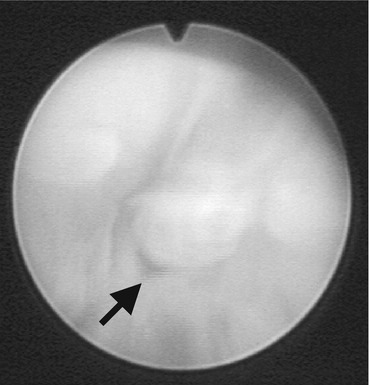
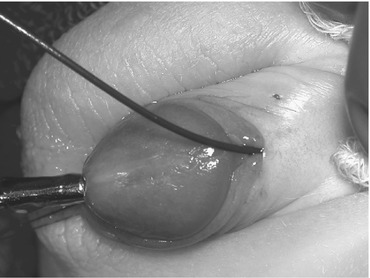
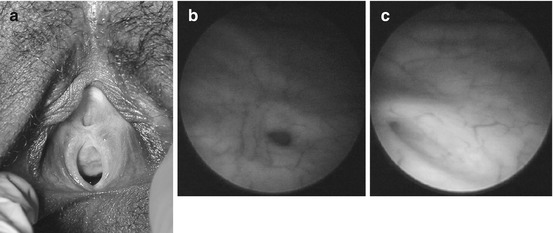

Fig. 21.1
Cold-knife incision of posterior urethral valves. The “half-moon” knife, seen in the center of the image, is cutting through the right valve leaflet. The verumontanum is seen in the right third of the image. The left valve leaflet is out of the image
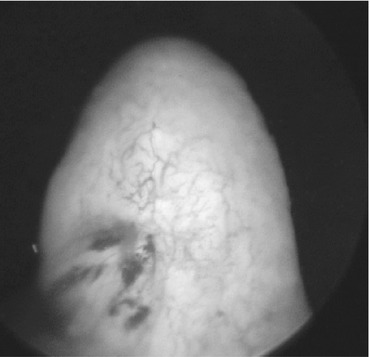
Fig. 21.2
Ureterocele. Figure shows a right moderately sized ureterocele associated with febrile UTIs, right complete ureteral duplication, and a multicystic dysplastic hydronephrotic upper pole moiety. It was transurethrally incised
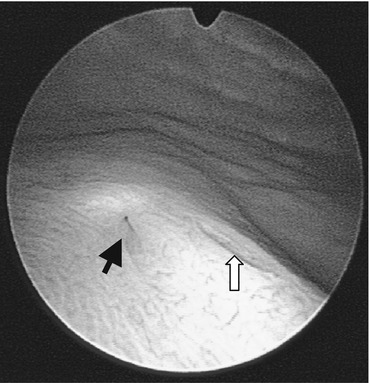
Fig. 21.3
Complete ureteral duplication. View of the right trigone reveals two ureteral orifices, the lateral, cephalad refluxing orifice (black arrow) serving the lower pole, and the medial, caudal orifice (white arrow) serving the upper pole duplex kidney
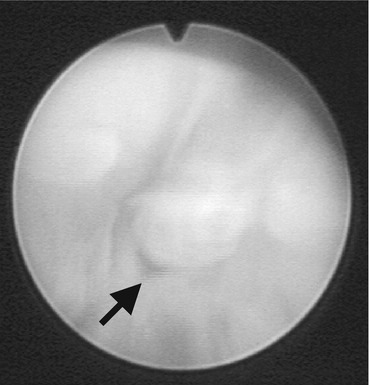
Fig. 21.4
Urethral stricture. Urethroscopy revealed a pinpoint lumen in the bulbar urethra (arrow) at the site of a prior visual internal urethrotomy. Open primary urethroplasty was required to correct this recurrent urethral stricture
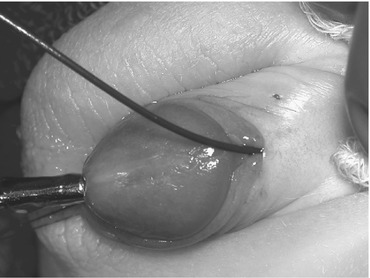
Fig. 21.5
Urethral duplication. When a dorsally foreshortened foreskin was noted, cystoscopic inspection revealed a partial urethral duplication to the symphysis. In this image, with the foreskin retracted, the black wire enters the dorsal nonfunctioning urethra, and the metal urethral sound enters the ventral functioning urethral meatus
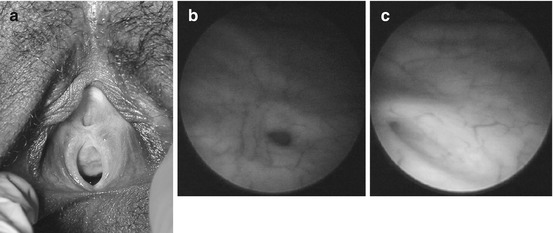
Fig. 21.6
Female epispadias with bilateral VUR. Exam under anesthesia reveasl subtle case of female epispadias associated with bilateral VUR and urinary incontinence. (a) External genitalia of female epispadias – note the horizontally wide urethral meatus with open urethral plate dorsally. The clitoris is bifid. The refluxing left (b) and right (c) ureteral orifices are seen
Cystourethroscopy with vaginoscopy is indicated in the patient with intersex (Fig. 21.7), urogenital sinus, or cloaca to delineate the surgical anatomy for repair. Tissue diagnosis of genitourinary malignancy (rhabdomyosarcoma, urothelial cancer) can be achieved by cystoscopy with tumor biopsy.
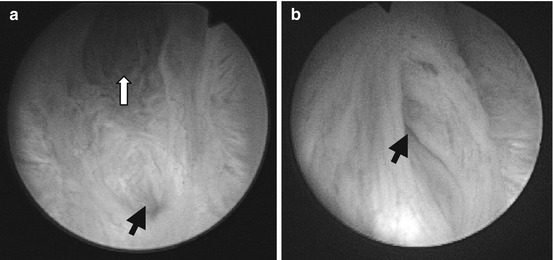
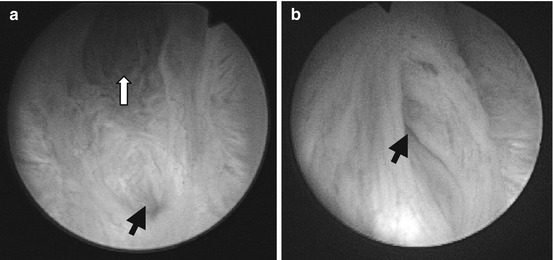
Fig. 21.7
Intersex. (a) Urogenital sinus of congenital adrenal hyperplasia (CAH). Cystourethroscopic evaluation of the urogenital sinus orifice reveals the bifurcation of the urethra (white arrow) and the vagina (black arrow). Cystourethroscopic placement of Fogarty balloons into the urethra and vagina aids the surgical reconstruction of the urogenital sinus. (b) Urethroscopic view of entrance into large utricle (arrow) on the verumontanum of an intersex patient with mixed gonadal dysgenesis
Contraindications include active bleeding disorders, hemodynamic instability, or untreated UTI/urosepsis.
Preoperative Investigation
Cystourethroscopy generally requires general anesthesia. Therefore, a standard preoperative evaluation, considering cardiopulmonary, endocrinological, and hematologic disorders that increase anesthetic risks, is necessary. Children with identified disorders may require preoperative blood chemistries, and children with congenital adrenal hyperplasia require stress steroid dosing. Preoperative radiological investigations often include ultrasound, cystourethrography, CT scan, nuclear scan, IVP, and/or MRI. Sterile urine is required to reduce risk of upper tract UTI prior to invasive instrumentation.
Preoperative Patient Preparation
Once cleared for surgery and meeting NPO restrictions, an oral sedative is given to prevent separation anxiety. At this time, IV antibiotics may be administered in the child with recurrent UTIs, depending on physician preference.
Specific Instrumentation
Most cystoscopic suites are equipped with monitors for fluoroscopic and video camera imaging, which allow multiple viewers, teaching, optical magnification, and video recording. A fiberoptic xenon light source and electrocautery are also required. Cystoscopic irrigant (sterile normal saline or sterile water) should be warmed to body temperature to diminish hypothermia. Several companies manufacture pediatric endoscopic equipment, including Wolf, Storz/Olympus, and ACMI. Given the delicate nature of this equipment, it is crucial to have several scopes available in case of equipment malfunction or unanticipated needs. Rigid pediatric cystoscopes range from 5 Fr to adult sizes, and the pubertal status of males should be noted to help judge the equipment needed. The 5 Fr “all-in-one” cystoscope is a one-piece instrument with united telescope and sheath; the 2.5 Fr to 3 Fr working channel is rather limiting. However the working channel increases in the larger scopes, with greatest caliber in the “all-in-one” cystoscopes. Other scopes consist of two pieces: the interchangeable telescope (0°, 30°, and 70°) and the sheath. A range of reusable and disposable equipment (graspers, biopsy forceps, bugbee electrode, wires, catheters, stents, balloons, baskets, laser fibers, and STING needles, to name a few) exist to achieve the indicated therapy but may be impossible if the working channel caliber is <5 Fr. Pediatric cystoscopes with an offset lens allow straight entry into the working channel. 7.5 Fr flexible or semirigid ureteroscopes should be on hand if ureteral access is necessary. Pediatric resectoscopes, ranging from 7.5 FR to adult sizes, require loops, balls, blades, or hooks unique to the FR size of the resectoscope. Resectoscopes can be used cold or hot (with electrocautery); however, most recommend sparing use of electrocautery to minimize thermal damage and stricturing with the highest stricture rates reported with loop resection [4]. Some have used holmium or Nd:YAG laser to cut valves or strictured tissue [4, 5]. It is convenient to have urethral sounds and/or bougies available for urethral dilation if needed.
Endoscopic bladder stone management requires the use of rigid and flexible cystoscopes. If percutaneous access to the bladder is needed, cystoscopically guided suprapubic access sheaths can be quite useful and come in an assortment of sizes, with 13 Fr to 18 Fr the most useful. To achieve stone fragmentation, electrohydraulic, ultrasonic, combined ultrasonic and pneumatic (Swiss lithoclast), or holmium laser lithotripsy can be used. Rigid probes include the electrohydraulic probes (3 Fr or 5 Fr), ultrasonic probes (as small as 5 Fr), and the Swiss lithoclast (3.3 and 3.8 mm). Of the flexible probes, holmium laser fibers are 200, 400, 600, or 1,000 μm, and Swiss lithoclast has a 0.9 mm flexible pneumatic probe.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


