Maternal assessment of fetal movement (kick counts)
Least expensive and least invasive fetal assessment test
Requires neither equipment nor hospital setting
TABLE 6-1 Comparison of Antenatal Fetal Tests
Antenatal Tests
Strengths
Limitations
Influential Factors
Kick counts
Inexpensive
Noninvasive
Simple
Need maternal participation
No supervision of physician
Nonstress test (NST)
Noninvasive
Simple
Limited value <32 wk
Low sensitivity
High false-positive rate
Smoking
Maternal medications
Illicit drug use
Magnesium sulfate
Sleep cycle
Prematurity
Vibroacoustic stimulation (VAS)
Noninvasive
Prevents some false-positive results from NST
Limited value <32 wk
Low sensitivity
Contraction stress test (CST)
Highest specificity
Contraindications: preterm labor, ruptured membranes, placenta previa, extensive uterine surgery
Cannot be used in premature infants
Labor-intensive
Biophysical profile (BPP)
Useful in premature fetuses
High false-positive rate
Betamethasone
Maternal hypoglycemia
Uterine artery Doppler ultrasound
Predicts fetal compromise earlier than other tests
Only useful in specific conditions
Purpose: Kick counts can be used for routine screening and reassurance in lowrisk pregnancies when a patient perceives decreased fetal movement. It can also be used as a method of surveillance in some higher risk pregnancies, for example, in women with a prior history of stillbirth.
Method of testing: The patient counts the number of fetal movements in a finite period of time. While performing this test, the woman should lie on her left side to improve blood flow to the fetus and eat prior to starting the test to
stimulate the fetus. Multiple testing strategies have been described, all with equal efficacy.
To perform the Cardiff technique, the patient counts fetal movements when she first gets up in the morning and records the time required for the fetus to move 10 times. Lack of 10 movements over 3 hours should prompt the patient to call her physician for further fetal testing.
Using the Sadovsky technique, the patient counts fetal movements over the course of 1 hour. To be considered “reassuring,” four or more fetal movements should be felt over the course of the hour. However, a second hour of monitoring to attain four movements is permissible. If four fetal movements have not been felt after 2 hours, the patient should contact her doctor for further recommendations.
Management after abnormal results: After the observation of decreased fetal movement, the follow-up test to evaluate fetal well-being is a nonstress test (NST).
Nonstress test
In the absence of acidosis or neurologic impairment, the fetal heart rate normally rises temporarily and randomly during fetal movement.
These increases in heart rate or accelerations are detectable using cardiotocography.
Method of testing: The NST is a noninvasive assessment that records the fetal heart rate simultaneously with uterine activity. The fetal heart rate is monitored with an external cardiotachometer, which uses ultrasound to evaluate fetal heart motion, giving an average of fetal heart beats. Uterine activity is monitored with an external tocodynamometer.
Criteria for test results: A “reactive” NST demonstrates at least two accelerations of the fetal heart rate over a 20-minute period. Prior to 32 weeks’ gestation, accelerations must be 10 seconds in duration and reach a peak 10 beats above the baseline to qualify as reactive. As the sympathetic and parasympathetic nervous systems mature, more stringent criteria are applied. In a fetus 32 weeks’ gestation or greater, each of the two accelerations must be 15 seconds in duration and must reach a peak of 15 beats above the baseline level (Fig. 6-1). If the fetal heart rate
is “nonreactive” after 20 minutes, the fetal heart rate should be observed for an additional 20 minutes to account for the possibility that the fetus may have been in quiet sleep during the initial observation period. There are many other factors that can influence the fetal heart rate tracing (see the following text).
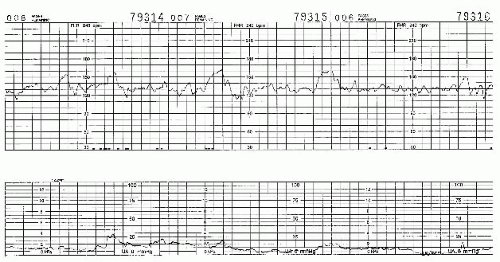
Figure 6-1. Reactive nonstress test. Fetal monitor strip records fetal heart rate (top) and uterine contractile activity (bottom). Several accelerations are evident.
Strengths and limitations: A reactive NST is highly predictive of a low risk of fetal mortality in the subsequent 72 hours, 96 hours, or a week depending on the indication for fetal testing. The negative predictive value of an NST is >90%. The positive predictive value is only 50% to 70%. Therefore, the NST is better suited to rule out rather than predict fetal compromise. Given the high false-positive rate, a nonreactive NST should be followed by more extensive testing such as biophysical profile, vibroacoustic stimulation, or contraction stress test.
Contraction stress test (CST) or oxytocin challenge test (OCT)
Purpose: The CST is designed to assess fetal response to the stress of induced uterine contractions causing transient uteroplacental insufficiency.
Method of testing: The mother is placed in the left lateral tilt position, and external monitors are applied. If three contractions of 40 seconds duration or greater are noted, a “spontaneous” CST can be performed without stimulation. In the absence of spontaneous contractions, uterine activity can be induced either by nipple stimulation or with a dilute solution of oxytocin until three contractions occur in a 10-minute time period.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


