Three years later, another group has tried again to answer to the same question [5]; meanwhile more studies using high accuracy methods have been published. In their systematic review of high accuracy studies, the prevalence in the general population was found to be 5.5 % (95 % CI: 3.3–8.5 %), in infertile population 8 % (95 % CI: 5.3–12 %), in recurrent aborters 13.3 % (95 % CI: 8.9–20 %) and in women having infertility and recurrent pregnancy losses the impressive incidence of 24.5 % (95 % CI: 18.3–32.8 %) (Figs. 13.1 and 13.2) [5].
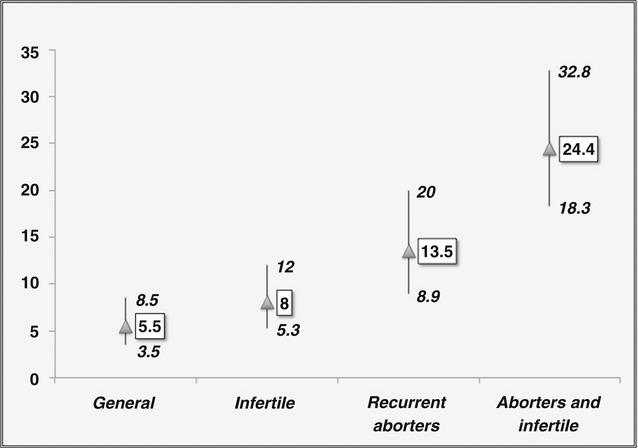
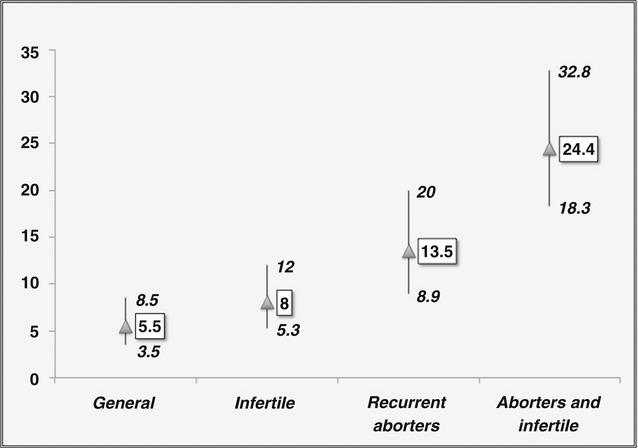
Fig. 13.2
Prevalence and estimated 95 % confidence intervals of uterine anomalies in the general and selected (infertile and recurrent aborters) populations (Data from Chan et al. [5])
It seems, therefore, that with the accumulation of more data and experience in the diagnosis of uterine anatomy with the newer available techniques, the incidence of CUA is higher in infertile population although this is not, yet, statistically significant.
Apart from the possible adverse effect of CUA, in general, on the achievement pregnancy, another interesting topic for investigation is the possibility that the different types of uterine anomalies could exert a different impact on the fertility potential of the woman. This possibility could be related to the fact that, the various categories of uterine anomalies are associated with different degrees of endometrial’s cavity deformity as well as with different structure and consistency of the myometrium.
Therefore, Saravelos et al. [26] reviewed the distribution and the prevalence of the various types of CUA in the different (general, infertile and recurrent aborters) populations based on the available data from the high accuracy studies. The prevalence of septate uterus in the general population was found to be 2 %, in infertile population 3.5 % and in recurrent aborters 5 %; the high incidence of uterine anomalies in the general population was mainly due to the presence of “arcuate” uteri. The same tendency was observed for bicornuate uterus and the others more severe anomalies. Consequently, the prevalence of uterine anomalies without arcuate uterus was 2.36 % in the general population, 5.6 % (more than double) in infertile patients and 7.1 % in recurrent aborters (Fig. 13.3).
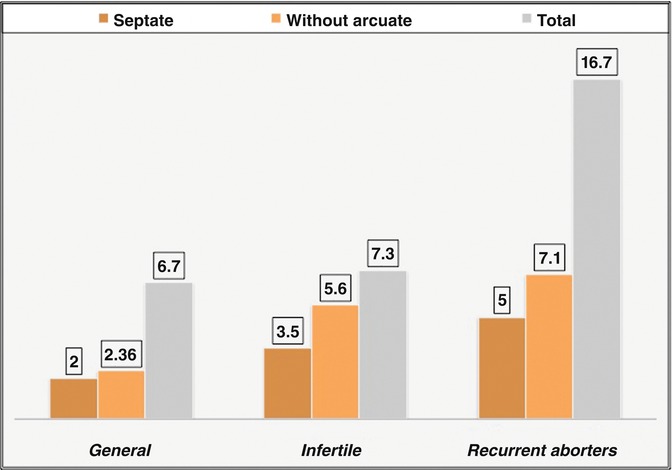
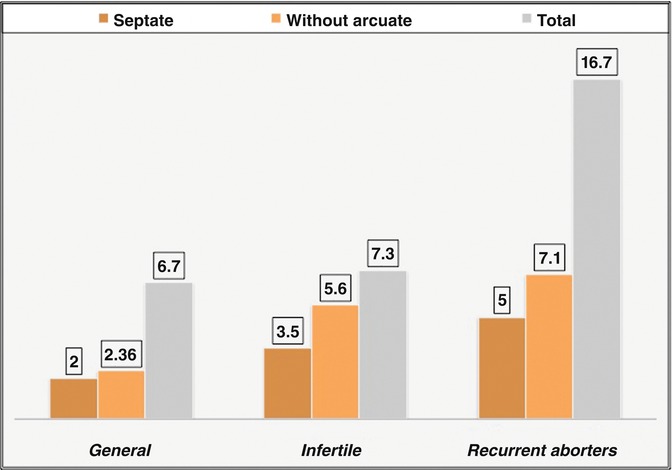
Fig. 13.3
Prevalence of uterine anomalies, uterine anomalies without arcuate uterus and septate uterus in the general and selected (infertile and recurrent aborters) populations (Data form Saravelos et al. [26])
Chan et al. [5] observed a similar tendency in their systematic review. The incidence of septate uterus in the general population was found to be 2.3 %, in infertile population 3 %, in recurrent aborters 5.3 % and patients with infertility and recurrent abortions 15.4 %. The high incidence of uterine anomalies in the general population was again found to be due to the presence of “arcuate” uteri. Furthermore, the prevalence of uterine anomalies without arcuate uterus was 3.2 % in the general population, 5.8 % in infertile patients, 9.3 % in patients with recurrent pregnancy losses and 20.1 % in patients with infertility and recurrent pregnancy losses (Fig. 13.4).
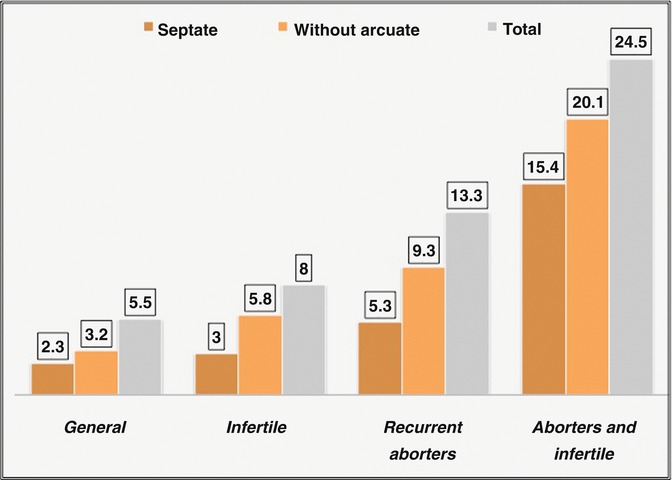
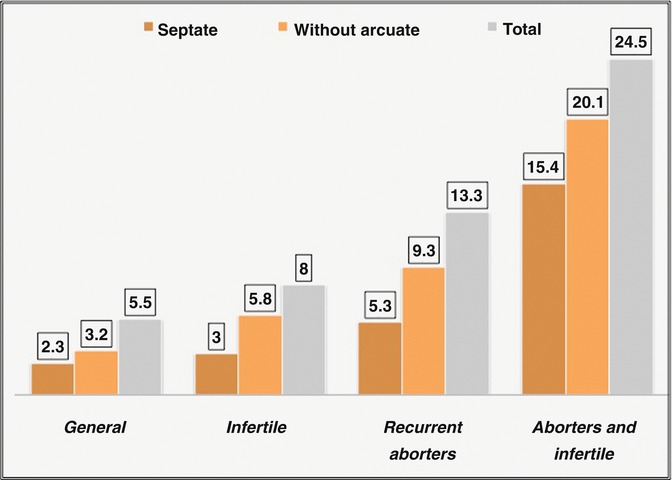
Fig. 13.4
Prevalence of uterine anomalies, uterine anomalies without arcuate uterus and septate uterus in the general and selected (infertile and recurrent aborters) populations (Data form Chan et al. [5])
Thus, the above-mentioned findings from prevalence studies represent indirect evidence supporting the notion that CUA could adversely impair fertility. Furthermore, it seems that the more severe the malformation of the cavity is, the more the possibility to play a role not only for the evolution but, also, for the achievement of pregnancy; septate uterus and more severe forms of uterine anomalies could adversely affect the fertility potential of the woman whereas this does not seem to be the case for arcuate uterus. It should be noted, however, that with the old AFS classification [3] the borders in the differential diagnosis between septate and arcuate uterus are not clear and the adoption of the new ESHRE/ESGE classification system could further elucidate this “hot” issue.
Conception in Women with Congenital Uterine Anomalies
Evidence coming from the study of the prevalence of CUA in the general and selected populations is useful but it is indirect. More reliable conclusions could be drawn only from comparative studies. In a systematic review of the available comparative studies, Chan et al. [6] was found that patients with septate uterus as compared with normal controls was associated with a statistically significant decrease by 15 % in the conception rates (RR: 0.86, 95 % CI: 0.77–0.96), a statistically significant almost threefold increase in the abortion rates (RR: 2.89, 95 % CI: 2.02–4.14) and a statistically significant increase almost by twofold in preterm delivery rates (RR: 2.14, 95 % CI: 1.48–3.11). The authors failed to detect a difference in the achievement of pregnancy in women with unicornuate uteri but the available data for this research question could not be considered as sufficient [5].
In a more recent meta-analysis, Venetis et al. [28] examined the probability of pregnancy achievement in a larger cohort of meanwhile available studies and in both natural and assisted conception cycles. They failed to detect any statistically significant difference when data were analyzed separately in natural (RR: 0.96, 95 % CI: 0.89–1.04) and assisted cycles (RR: 0.66, 95 % CI: 0.37–1.19) in women with CUA as compared to those without CUA. However, the probability of conception, assisted or spontaneous, in women with congenital uterine anomalies (CUA) was found to be significantly decreased by ~15 % (RR: 0.86, 95 % CI: 0.74–1.00) when all data from natural and assisted cycles were analyzed together, thus, confirming the observation of the previous meta-analysis.
Most of the comparative studies available in the literature and included in the pre-mentioned meta-analyses are still retrospective and, thus, solid conclusions could not be, yet, drawn. However, according to the best available evidence (level C/meta-analysis of retrospective comparative studies) the presence of CUA might be associated with a detrimental effect on patient’s fertility potential decreasing the probability of pregnancy achievement by ~15 % (Class IIb Recommendation).
Fertility After Hysteroscopic Treatment
The results of hysteroscopic treatment of septate and bicorporeal septate uteri [9, 16, 17] could offer some additional evidence for the potential role of these anomalies on patients’ fertility. However, the anatomic restoration of the cavity does not necessarily mean that it will accompanied by the restoration of normal fertility potential; treatment of septum is always associated with “trauma” and healing process of the cavity could impair the functional outcome of the procedure [13]. Hence, an increase in conception rates after surgical correction of the anomaly might be considered as an indirect proof of a harmful effect of the anomaly on woman’s fertility whereas a neutral effect might not, since this could be due to the “trauma” following the procedure.
Thus, Mollo et al. [21] studied prospectively conception rates in infertile patient with septate uterus and otherwise unexplained infertility after septum resection compared to those of couples with unexplained infertility only; conception rates were found to be almost double in the group of infertile patients who underwent septotomy, thus supporting that notion that the presence of septum adversely affects fecundity.
Nouri et al. [22], in a review of all available observational retrospective studies, found a pooled post-operative pregnancy rate of ~60 % and live birth rate of ~45 % in infertile women who underwent septum resection. A “theoretical” group for comparisons could be also considered untreated infertile patients with unexplained infertility; the expected spontaneous pregnancy rates in this group do not exceed 35 % (The ESHRE Capri Workshop 1996) [10].
Venetis et al. [28] examined the value of hysteroscopic septotomy in a systematic review of all the published comparative studies. They found that surgical correction of uterine septa is associated with a ~60 % decrease (RR: 0.37, 95 % CI: 0.25–0.55) in the probability of miscarriage as compared to women that are not treated. This effect seems to be present, not only in women with a history of recurrent spontaneous abortions but also in infertile patients and in the non-specific population analyzed in the remaining studies. However, hysteroscopic removal of the septum was not found to lead to a statistically increased probability of pregnancy achievement (RR: 1.14, 95 % CI: 0.79–1.65) and delivering at term (RR: 0.66, 95 % CI: 0.29–1.49). However, the effect sizes observed in this analysis (that imply a beneficial effect) and the fact that both achievement of pregnancy and preterm delivery have been shown to be associated with the presence of a uterine septum, mandate the accumulation of further evidence in order to properly assess the value of hysteroscopic septotomy for these indications.
Thus, concerning the achievement of pregnancy after septum incision, it seems that it is still very early to draw definite conclusions. However, there is some indirect evidence mainly from the prospective study of Mollo et al. [21], that septum could adversely affect fertility.
Possible Biological Explanations
Although the association between CUA and suboptimal fertility potential seems, nowadays, to be accepted and supported by the evidence available, the exact etiology and the plausible biological mechanism underlying infertility and pregnancy loss remain still unclear. Several hypotheses have suggested in an effort to explain these findings.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


