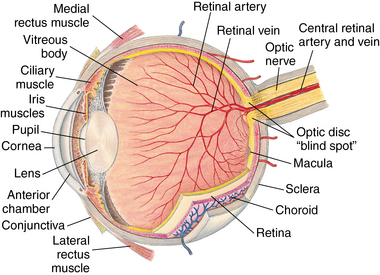
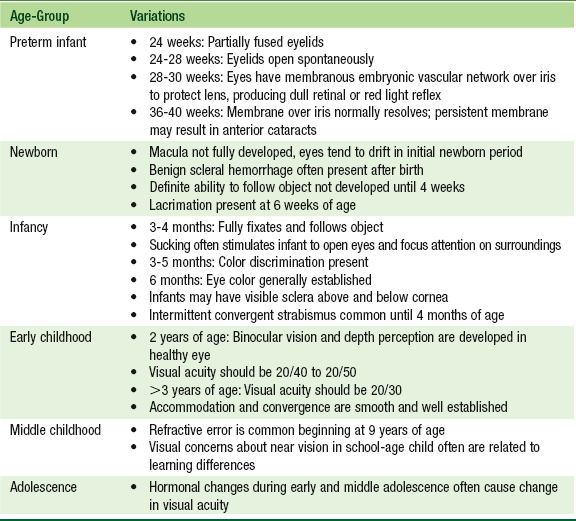
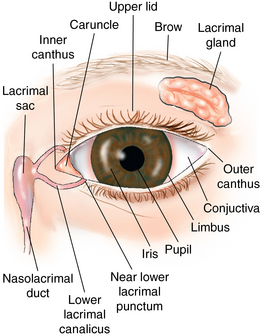
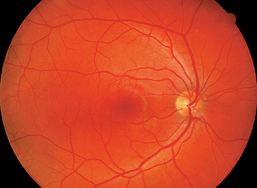
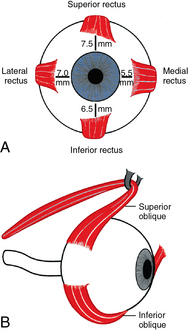
CHAPTER 11 The development of the eye fields begins in the third week of embryonic development with the optic groves forming in the neural tube, and by the end of the fourth week the optic vesicle is formed and lies close to the ectoderm surface. The surface ectoderm thickens and forms the lens placode. By the fifth week of gestation, the optic cup and the lens cavity are formed, and by the sixth week, invagination of the optic vesicle occurs forming the choroid layer and vasculature of the eye. The formation of the cornea, lens, and anterior chamber proceeds during the seventh and eighth week, and the eyelid folds develop and begin to cover the palpebral fissure. It is during this period of gestation that insults to the fetus, such as maternal rubella, cause the development of congenital cataracts. Development of the retinal tissue continues with the differentiation of the nerve fiber layer, proliferative layer of the macula, and the pigmented layer of the retina that precedes the development of the iris and the ciliary body, which occurs between the ninth and twelfth weeks of embryonic development. The ciliary body gives rise to the ciliary muscles, which control the accommodative reflex and pupillary aperture (Figure 11-1). Development of the structures of the eye is complete by 15 weeks’ gestation. At the fourth month of gestation, the development of the retinal blood vessels is initiated and full vascularization of the retina occurs just before birth in a term infant.1 The pupillary light reflex, which requires intact optic and oculomotor nerves, can be elicited by 30 weeks’ gestation. The optic nerve is also developing at the same time as the retina. There are as many as 8 million cells in the optic nerve and 5 million retinal cells in the optic neuron at birth that compete for synaptic sites on the nerve. Cells that are not oxygenated do not develop. Hypoxia or hyperoxia in the preterm infant often impact the normal development of the retina, and cause a retinopathy, a disorder of the retinal vessels. Infants born prematurely have an avascular zone in the periphery of the retina that disrupts the normal proliferation of the retinal vessels and interrupts blood flow to the visual receptors. The disruption of blood flow may lead to retinal detachment from the choroid, causing visual impairment or blindness if left untreated. The gestational age of the infant at birth determines the area of the avascular zone.1 Very low birth weight infants (≤1500 g) are at high risk for retinopathy of prematurity, and infants born at 28 weeks’ gestation or weighing ≤1000 g are at highest risk for developing macular folds and retinal detachment.2 Refractive anomalies also occur approximately eight times more frequently in preterm infants than in term infants.3 Term infants from 36 to 40 weeks of gestation can perceive shape, color, motion, and patterns at birth. Visual development in the newborn is dependent upon development of the visual pathways that link the eyes to the lateral geniculate nucleus in the thalamus to the visual cortex located in the occipital lobe of the brain. Exposure to light begins the synaptic development of the neurons at birth.3 Central fixation is present shortly after birth in the term infant, and the human face at a distance of 8 to 12 inches holds the most visual interest for a newborn. The term infant is hyperopic, or farsighted, at birth. Visual images are focused behind and not on the retina, so the visual image is blurred. For the infant to see near objects, the ciliary muscles of the eye must work hard to accommodate, or shape, the lens; in time these efforts of the ciliary muscles result in thickening of the lens, which makes accommodation of the image onto the retina possible. The term infant’s eyes often wander or deviate in the first 6 weeks when trying to achieve visual fixation in the central field of vision. After 6 weeks of early visual stimulus, an infant is able to focus and visually follow an object or the parent’s movements. Any inability to visually focus after 6 weeks of age in a term infant is considered suspect and at 3 months of age is considered abnormal. As the eyeball or globe grows, the hyperopia decreases and the lens hardens, but detailed visual acuity is not present until 3 to 4 months of age in the healthy eye and not until 3 to 4 months corrected age for preterm infants (Table 11-1). Differentiation and maturation of the retinal layers of the macula, which is responsible for colors and contrasts, precise visual acuity, and stereoscopic vision; and the fovea, which is responsible for central vision, continues until 8 months of age.3 The critical window for normal development of full visual acuity is from birth to 5 to 6 years of age, and the synaptic development of the neuronal paths in the visual cortex continues until approximately 10 years of age. After this age, conditions that affect early visual development cannot be completely corrected (Table 11-2). TABLE 11-1 The lacrimal gland is located in the lateral aspect of the frontal bone in the orbital cavity (Figure 11-2). It is a peanut-sized gland similar to the salivary glands. In each eyelid, a lacrimal duct opens onto the eyelid margin, and the nasolacrimal duct opens into the lacrimal sac, which is buried in the frontal process of the maxillary bone. The lacrimal puncta are noted at the edge of the upper and lower eyelids at the medial or inner canthus and allow the drainage of tears into the nasolacrimal duct and the lacrimal caruncle. The lacrimal caruncle is the elevated area of tissue bordering the upper and lower medial canthus and assists in drainage of tears. Tear production is normally present by 6 weeks of age in the term infant. The sclera, the outermost layer of the exterior structure of the globe or eyeball, is the firm collagenous layer that protects the intraocular structures (see Figure 11-2). The conjunctiva is formed by thin mucous membrane lining the anterior surface of the sclera and inner eyelids and acts along with the tear film as a protective covering for the cornea. The conjunctiva has two surfaces: the palpebral and bulbar. The palpebral conjunctiva lines the inner eyelids, is vascular, and is covered by papillae. The bulbar conjunctiva is clear and contains no papillae and very few blood vessels. The bulbar conjunctiva covers the sclera up to the limbus, the juncture of the sclera and the cornea. The iris is the pigmented structure containing the sphincter and dilator muscles, connective tissue, and pigmented epithelium. An absence of color in the iris may indicate albinism. The center of the iris is controlled by the ciliary body and iris muscles and forms the aperture, or pupil. The pupil constricts or dilates depending on the amount of light entering the eye. The ciliary body produces aqueous humor and controls accommodation. The iris lies behind the anterior chamber and in front of the crystalline lens and is protected by a thin clear capsule attached by small filaments to the ciliary body. A cataract is an opacity that obscures the crystalline lens. The six ocular muscles, inserted into the scleral surface, control the movement of the eye (Figure 11-3). The four rectus muscles—the superior, inferior, medial, and lateral recti—originate at the top of the globe deep in the cranium and extend from the anterior to insert at the back of the globe. The medial rectus muscle is responsible for the movement of the eye toward the midline, and the lateral rectus muscle innervated by cranial nerve VI moves the eye away from the midline. The inferior and superior rectus muscles move the eye upward and downward and also have overlapping functions with the oblique muscles. The two oblique muscles—the superior and inferior oblique—insert at the anterior and posterior globe. The superior oblique tendon passes through the trochlea, the small, cartilaginous pulley on the frontal bone. The superior oblique muscles are responsible for movement of the eye downward and inward, and the inferior oblique moves the eye upward and inward. The superior oblique muscle is innervated by cranial nerve IV, and paralysis of the nerve causes a head tilt or torticollis in children to compensate for the weakened muscle. FIGURE 11-3 A, Four extraocular recti muscles. B, Oblique extraocular muscles. (From Palay DA, Krachmer JH: Primary care ophthalmology, ed 2, St. Louis, 2005, Mosby.) The vitreous body is the large interior cavity of the globe and contains a clear gel or vitreous humor. The choroid is the interior layer of the eye between the sclera and the retina and is continuous with the iris and ciliary body. It is highly vascular and nourishes the receptor cells of the retinal epithelium. The outer layer of the retina contains photoreceptors, the rods and cones, which are stimulated by light focused by the lens and translate light energy or impulses into neuronal activity. The neurons activate the nerve fiber layer of the retinal epithelium and synaptic activity and transmit through the optic nerve to the brain, which perceives the visual image. The retinal vessels and optic nerve fibers enter and exit through the optic cup and divide into two branches on the surface of the optic disc. The optic disc, the anterior aspect of the optic nerve, is pink to orange-red or pale with a yellow cup at its center (Figure 11-4). There are no photoreceptors in the optic disc, which creates a blind spot of 5 degrees in the visual field.4 The macula lies medial to the optic nerve on the fundus, the posterior surface of the retina. The fovea or fovea centralis is a central depression in the macula without vessels and has darker pigmentation than the retina. This is the area where vision is most perfect, and the ciliary body works to accommodate the lens to focus an image on the fovea. The arteries on the fundus appear thinner and more orange-red than the veins, which are larger and darker (see Figure 11-4). The normal arterial-to-venous ratio (A:V) is approximately 2:3 in the healthy individual. Vascular changes present in the retina often reflect abnormal conditions in the systemic vasculature such as diabetes and hypertension. Papilledema, bilateral optic disc edema, is also associated with increased intracranial pressure. Retinal hemorrhage is associated with acute traumatic brain injury and inflicted traumatic brain injury. Retinal hemorrhages associated with inflicted traumatic brain injury in children involve deeper layers of the retina and are found more on the periphery of the retina.5 Thick epicanthal folds are seen more commonly in infants and young children of Asian and Latino descent. They partially or completely cover the inner canthus at birth and diminish by middle childhood. Asian populations have a genetic predisposition to myopia. In one study, 68% of Asian children were found to be myopic.3 The pediatric health care provider should focus particular attention to early vision screening in this population of children. Ethnicity is a risk factor for severe retinopathy of prematurity (ROP). Asian and black infants have a higher risk of developing threshold ROP as compared to white infants.6 Retinal pigment or melanin is often found on the scleral surface of Latino and African-American children. The pigmented areas usually become evident in early or middle childhood and persist into adulthood. This is within the range of normal variations of the eye and does not impact visual health. The retinal light reflex or “red” light reflex varies in color in darkly pigmented individuals. The fundus appears pale yellow or beige because of the increased melanin in the skin, and the optic disc is also often a pale yellow.
Eyes
Embryological development
Developmental and physiological variations
Age
Developmental Stage of Vision
Birth
Awareness of light and dark
Neonatal
Rudiments of fixation on near object
2 weeks
Intermittent fixation
4 weeks
Follows moving objects
6 weeks
Fixates and follows moving objects
8 weeks
Convergence beginning to stabilize
4 months
Inspects hands and small held objects; vision 20/300
6 months
Retrieves small objects; hand-eye coordination appears
9 months
Binocular vision clearly established; beginning of depth perception
12 months
Vision 20/180; looks at pictures with interest; fusion is established
18 months
Convergence established; visual localization peripherally poor
2 years
Accommodation well developed; vision 20/40 in normal eyes
Anatomy and physiology
External eye
Extraocular muscles and internal eye
Family, cultural, racial, and ethnic considerations
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree