Eye Emergencies and Trauma
Daniel J. Karr and Alex V. Levin
Ocular trauma is a frequent presenting complaint and a major cause of ocular morbidity and unilateral blindness in children. The magnitude of serious eye injuries in children has been estimated at 11.8 per 100,000 per year.1 Children in the 11-to-15-year age group have a higher incidence of trauma compared to other age groups. Boys outnumber girls approximately 3 or 4 to 1.2
Ocular injuries require prompt evaluation and care in order to preserve vision. Evaluation of the injury is more difficult due to decreased cooperation and understanding in children. The injured patient is frequently young, afraid, in pain, and able to provide only limited compliance. The examination should be as complete as the injury permits; forcible evaluation may risk further damage. Topical anesthesia, local anesthesia, and sedation are all useful for assessing and treating minor trauma. If the pediatrician or emergency room physician cannot perform an adequate examination, or as soon as there is concern for significant ocular damage, the injured eye should be covered with a protective shield (not patched) and ophthalmology consultation should be obtained. It is also important to recognize that managing the eye injury always takes a lower priority than managing life-threatening injuries and serious head trauma. The injured eye can be shielded while emergency procedures are under way to stabilize the child systemically. Yet, with the exception of the uncommon vasovagal response induced by eye examination, the ophthalmologist can conduct a limited brief assessment that will be relatively noninvasive and may offer helpful management guidelines. While that examination is pending, the eye should be shielded (not patched).
Assessment of visual acuity in both eyes is important for predicting the final visual outcome and for medicolegal purposes. It can also help in assessing the cause for visual loss. For example, if a child develops a swollen eye after being punched at school and the vision in that eye is 20/100 but the eyeball is otherwise apparently normal, it would be reassuring to know that the other eye (not injured) also sees poorly, indicating the child may simply need glasses for nearsightedness. Techniques for assessing vision, opening the eye, and examining the eyeball have been discussed in Chapter 580.
Amblyopia frequently results from ocular trauma. Extended observation and treatment for optimal vision development are often needed once the initial injuries have been managed.
CORNEAL ABRASION
Corneal abrasion is one of the most frequent ocular injuries of childhood. The abrasion results from mechanical removal of the superficial epithelial layers of the cornea. This can cause intense pain, protective spasm closure of the lids, tearing, and photophobia, although some children may be surprisingly asymptomatic. Examination is facilitated by a drop of topical anesthetic followed by fluorescein dye. The dye is available as a liquid mixed with anesthetic or in dry impregnated strips. The latter tends to be more effective in diagnosis, as it allows only a small amount of dye to be placed. The strip must be wet with a drop of liquid (water, normal saline, Ringers, etc) and then gently touched briefly to the pink palpebral conjunctiva lining the inside of the lower lid or the conjunctiva on the white of the eye. The fluorescein will define the extent of epithelial cell loss when examined with cobalt blue illumination (blue light on direct ophthalmoscope or Woods lamp; Fig. 583-1).
Use of a cycloplegic agent and topical antibiotic ointment will provide comfort and prevent infection. The placement of a pressure patch to close the eyelid and promote healing of the epithelium was traditional care for children and adults, but more recent studies indicate that the patch may not increase the rate of healing or comfort. Younger children may resist or remove the patch. Normal eye closure during sleep will usually be enough to promote a rapid recovery. Corneal abrasions typically are healed within 1 to 2 days. Patients are generally examined within 24 hours to monitor healing, particularly if the abrasion is large or central. Small abrasions away from the visual axis do not necessarily need follow-up if the child is asymptomatic and the eye is not injected after 2 to 3 days. Secondary infection is rare except in those who wear contact lenses. Any child wearing a contact lens who presents with a red or painful eye should have the contact removed immediately. The dye can then be applied. If a corneal abrasion is found, the child should be referred promptly to an ophthalmologist. If there is a white area (eFig. 583.1  ) at the site of the fluorescein staining, this may indicate an infectious ulcer. The pediatrician should not treat, but should refer the child immediately, as the ophthalmologist may choose to culture the area; the results of culture may be useless after prior antibiotic treatment. Never patch those who wear contact lenses, as there is evidence that it may increase the risk for secondary infection in these patients.
) at the site of the fluorescein staining, this may indicate an infectious ulcer. The pediatrician should not treat, but should refer the child immediately, as the ophthalmologist may choose to culture the area; the results of culture may be useless after prior antibiotic treatment. Never patch those who wear contact lenses, as there is evidence that it may increase the risk for secondary infection in these patients.
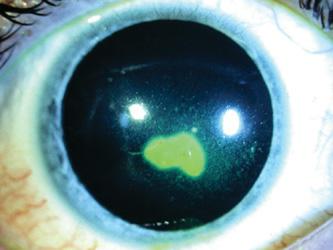
FIGURE 583-1. Corneal abrasion with fluorescein staining.
THERMAL INJURIES
Thermal burns of the cornea from cigarette ashes, match heads, and other combustible materials are usually not serious, but when they are, the ocular surface and lid margins may be destroyed with little hope for salvageable vision (eFig. 583.2  ). The rapid eyelid-closure reflex and Bell’s phenomenon (upward movement of the globe when threatened) usually limit the extent of the burn. Children burned in house fires or accidents usually sustain minimal, if any, corneal injury unless they were rendered unconscious by smoke inhalation or the eyes were abusively forced open. Cigarette burns of the cornea are the most common thermal injury to the ocular surface in childhood. The majority of these injuries occur in 2- to 4-year-old children and are usually sustained accidentally when a toddler runs into a cigarette held at eye level by an adult.3 The treatment is generally the same as for corneal abrasions.
). The rapid eyelid-closure reflex and Bell’s phenomenon (upward movement of the globe when threatened) usually limit the extent of the burn. Children burned in house fires or accidents usually sustain minimal, if any, corneal injury unless they were rendered unconscious by smoke inhalation or the eyes were abusively forced open. Cigarette burns of the cornea are the most common thermal injury to the ocular surface in childhood. The majority of these injuries occur in 2- to 4-year-old children and are usually sustained accidentally when a toddler runs into a cigarette held at eye level by an adult.3 The treatment is generally the same as for corneal abrasions.
RADIATION BURNS
Ultraviolet light from unprotected sun exposure, sunlamps, snow reflection, and welding arcs can produce a diffuse superficial punctate keratitis (many pinpoint corneal abrasions) of the cornea that is extremely painful. The patient will present with a combination of pain, foreign-body sensation, tearing, photophobia, and blepharospasm. The findings are similar to those found with corneal abrasion except that there may be a delay from the exposure to the time the child becomes symptomatic. Treatment consists of broad-spectrum antibiotic ointment (eg, erythromycin, polysporin), consideration for cycloplegia, and patching for comfort and to promote healing. The epithelium heals over 24 to 48 hours and usually causes no permanent sequelae. Those who wear contact lenses can also sustain this injury and require special treatment as discussed above.
CHEMICAL BURNS
Treatment for chemical burns should be started immediately once the history of exposure is obtained. Acid burns are less serious than alkali burns, because acid precipitates proteins and results in a barrier to further penetration. In contrast, alkaline agents (eg, lye, cement, oven cleaner) activate collagenases, which may produce corneal liquefaction and ulceration, possibly leading to full thickness perforation. Alkali burns may also cause an increased intraocular pressure secondary to contraction of the sclera and damage to the trabecular meshwork.
When the eye has been exposed to chemicals, begin copious irrigation with water or isotonic saline for 20 to 30 minutes. Use of a topical anesthetic and lid speculum will provide more comfort and permit thorough irrigation under the lids, but one should not wait to acquire these items if there is likely to be any delay. Effectiveness of irrigation is checked by assessing the pH of the tear film 5 to 10 minutes after installation. Irrigation should be continued until a neutral pH of 7.0 is attained or in unilateral exposure, until the pH of the affected eye is equal to that of the unaffected eye. Normal tear film pH is 7.3 to 7.7.
Intravenous tubing (with the needle removed) attached to an irrigation solution may be used to irrigate over the cornea and under the lids to effectively remove contaminants and neutralize the tear film. Commercial irrigation devices such as the Morgan lens permit a contact lens attached to irrigation tubing to be placed over the cornea and under the lids. This provides comfortable, extended, hands-free irrigation. Placement of a topical anesthetic drop should be applied periodically for comfort.
Chemical burns can cause changes that range from superficial punctate staining to complete sloughing of the corneal epithelium. Severe chemical burns may produce pronounced chemosis, conjunctival ischemia, corneal edema and opacification, and anterior chamber inflammation. Treatment after irrigation consists of removing all particulate debris, including sweeping the fornices with a moistened cotton-tip swab; administering cycloplegia or topical antibiotic ointment; pressure patching; and, if needed, giving oral analgesics, glaucoma medications, and topical corticosteroids (use cautiously). Urgent ophthalmology consultation is suggested but not until the irrigation procedure is completed. The long-term management of severe burns may involve lysis of conjunctival scars (symblepharon), application of collagenase inhibitors, conjunctival or corneal transplantation, and dry-eye management.
FOREIGN BODY OF THE CONJUNCTIVA AND CORNEA
When faced with an apparent superficial ocular foreign body, several considerations are useful before attempting to remove it. Any history of high-velocity exposure (metal striking metal), the presence of associated conjunctival hemorrhage, or a foreign body overlying an oval or teardrop-shaped pupil may indicate globe penetration with an intraocular foreign body. In such cases, urgent ophthalmology consultation is indicated and the pediatrician should not attempt to remove the object.
Superficial conjunctival foreign bodies (eFig. 583.3  ) are usually removed by flushing the eye with isotonic saline or using a moistened cotton-tip applicator. Eversion of the upper lid is necessary if a foreign body is not readily located, especially if there are linear vertical fluorescein stain lines on the superior cornea. Topical anesthetic installation will facilitate the examination and foreign-body removal. The dye will also pool around a foreign body and thus aid in its identification. Eversion of the upper eyelid can be performed by having the patient look down while placing a cotton-tip or other blunt object against the lid crease. At the same time, the lid margin and tarsal plate are elevated by pulling upward with the lashes (eFig. 583.3
) are usually removed by flushing the eye with isotonic saline or using a moistened cotton-tip applicator. Eversion of the upper lid is necessary if a foreign body is not readily located, especially if there are linear vertical fluorescein stain lines on the superior cornea. Topical anesthetic installation will facilitate the examination and foreign-body removal. The dye will also pool around a foreign body and thus aid in its identification. Eversion of the upper eyelid can be performed by having the patient look down while placing a cotton-tip or other blunt object against the lid crease. At the same time, the lid margin and tarsal plate are elevated by pulling upward with the lashes (eFig. 583.3  ).
).
Corneal foreign bodies generally cause more pain than conjunctival foreign bodies. If the foreign body cannot be removed by irrigation, referral to an ophthalmologist is advisable unless the pediatrician/emergency physician is comfortable with proper foreign-body-removal techniques using a slit lamp.4 After removing a foreign body, there is usually an associated corneal epithelial defect. Topical broad-spectrum antibiotic therapy is recommended for 2 to 4 days. All patients should be examined in 24 hours to rule out early corneal infection. Metallic foreign bodies may leave a localized rust stain. This may have to be removed by an ophthalmologist using a slit lamp.
EYELID LACERATIONS
The nature and extent of the injury will often be suggested by the history. With unobserved or high-risk trauma, especially high-velocity impact or injury by a projectile, an animal bite, or a penetrating implement, the possibility of intraocular penetration and foreign body must be explored. A small puncture wound to the lid, a conjunctival laceration and hemorrhage, or a distorted pupil can all be signs of globe perforation. Complete ocular examination is frequently necessary and includes a careful exploration of the wound(s), a dilated fundus examination, and a possible computerized tomography (CT) scan to exclude the presence of an intraocular or intraorbital foreign body.
Lacerations involving the eyelid margin (eFig. 583.4  ) or nasolacrimal system (eFig. 583.5
) or nasolacrimal system (eFig. 583.5  ) should be treated by an ophthalmologist. Other indications for referral to an ophthalmologist include ptosis, full thickness laceration, missing tissue, and any concern about globe injury. Careful ophthalmic primary closure can help to prevent permanent notching of the eyelid margin, chronic tearing, trichiasis (inward turning of the eyelashes), or scarring of the nasolacrimal drainage system. Canalicular injury may not be recognized initially but should be suspected in medially located lid lacerations, especially those caused by dog bites or by catching the lid on a hook or other object. Lateral displacement of the papilla on which the puncta normally sits is a worrisome sign that the canaliculus has been severed. An examination under anesthesia may be necessary to define the extent of injury more definitively. To repair a severed canaliculus, the ophthalmologist may place a silicone stent at the time of anesthesia.
) should be treated by an ophthalmologist. Other indications for referral to an ophthalmologist include ptosis, full thickness laceration, missing tissue, and any concern about globe injury. Careful ophthalmic primary closure can help to prevent permanent notching of the eyelid margin, chronic tearing, trichiasis (inward turning of the eyelashes), or scarring of the nasolacrimal drainage system. Canalicular injury may not be recognized initially but should be suspected in medially located lid lacerations, especially those caused by dog bites or by catching the lid on a hook or other object. Lateral displacement of the papilla on which the puncta normally sits is a worrisome sign that the canaliculus has been severed. An examination under anesthesia may be necessary to define the extent of injury more definitively. To repair a severed canaliculus, the ophthalmologist may place a silicone stent at the time of anesthesia.
Full thickness perforation of a lid, recognized by an external puncture wound that is also visible on lid eversion, is a high-risk indicator for orbital, globe, or brain (upper lid) injury. CT scan is recommended.
CONJUNCTIVAL LACERATIONS
All but the largest conjunctival lacerations can be managed without surgical repair. Most will heal spontaneously within a few days. Lacerated conjunctiva will stain with fluorescein dye as described above for the diagnosis of corneal abrasion. Application of topical antibiotic with or without a pressure patch and observation constitute the usual therapy. Secondary infection is rare.
CORNEOSCLERAL LACERATIONS (RUPTURED GLOBE)
A penetrating injury represents a full thickness scleral or corneal laceration. This is a serious ocular emergency requiring immediate medical attention. The history typically describes a sharp object striking the lid or eyeball. The globe can also be ruptured through severe blunt impact. Taking a careful history is essential to identify the risk for infection or a foreign body and the likelihood that the latter can be detected by CT or magnetic resonance imaging (MRI) imaging.
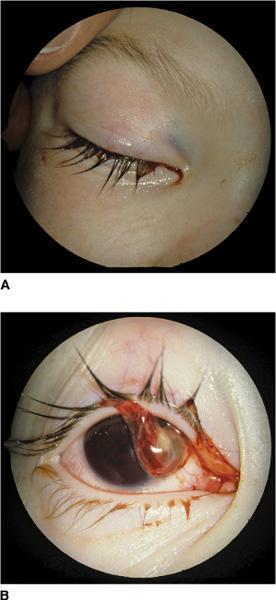
Clinical findings depend on entry site. Frequently the lids and conjunctiva are markedly swollen with severe subconjunctival hemorrhage (eFig. 583.6  ). In some cases, the eye may look remarkably normal until further exploration reveals the damage (Fig. 583-2). The eye attempts to naturally seal a rupture by having the uveal tract (choroid for lacerations of the sclera, iris for lacerations of the cornea) plug the wound. When the cornea is lacerated, the anterior chamber may be shallow with a distorted pupil (Fig. 583-3A). The peak of the pupil will point in the direction of the rupture as the iris flows into the wound (Fig. 583-3B). There may be accompanying hyphema, conjunctival laceration, or subconjunctival hemorrhage. Any black or brown tissue on the sclera after trauma should be presumed to be choroid emerging through a scleral laceration until proven otherwise (Fig. 583-4). If the patient has 360 degrees of subconjunctival hemorrhage or chemosis after trauma, it is impossible to rule out a scleral wound because the sclera is obscured from view. In such cases, urgent ophthalmology consultation is indicated regardless of the quality of the visual acuity. Vision may be surprisingly good even when the sclera has been ruptured.
). In some cases, the eye may look remarkably normal until further exploration reveals the damage (Fig. 583-2). The eye attempts to naturally seal a rupture by having the uveal tract (choroid for lacerations of the sclera, iris for lacerations of the cornea) plug the wound. When the cornea is lacerated, the anterior chamber may be shallow with a distorted pupil (Fig. 583-3A). The peak of the pupil will point in the direction of the rupture as the iris flows into the wound (Fig. 583-3B). There may be accompanying hyphema, conjunctival laceration, or subconjunctival hemorrhage. Any black or brown tissue on the sclera after trauma should be presumed to be choroid emerging through a scleral laceration until proven otherwise (Fig. 583-4). If the patient has 360 degrees of subconjunctival hemorrhage or chemosis after trauma, it is impossible to rule out a scleral wound because the sclera is obscured from view. In such cases, urgent ophthalmology consultation is indicated regardless of the quality of the visual acuity. Vision may be surprisingly good even when the sclera has been ruptured.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


