Background
Preterm birth is the major cause of perinatal mortality in the United States. In the past, pregnant women have been recommended to not exercise because of presumed risks of preterm birth. Physical activity has been theoretically related to preterm birth because it increases the release of catecholamines, especially norepinephrine, which might stimulate myometrial activity. Conversely, exercise may reduce the risk of preterm birth by other mechanisms such as decreased oxidative stress or improved placenta vascularization. Therefore, the safety of exercise regarding preterm birth and its effects on gestational age at delivery remain controversial.
Objective
The objective of the study was to evaluate the effects of exercise during pregnancy on the risk of preterm birth.
Data Sources
MEDLINE, EMBASE, Web of Sciences, Scopus, ClinicalTrial.gov , OVID, and Cochrane Library were searched from the inception of each database to April 2016.
Study Design
Selection criteria included only randomized clinical trials of pregnant women randomized before 23 weeks to an aerobic exercise regimen or not. Types of participants included women of normal weight with uncomplicated, singleton pregnancies without any obstetric contraindication to physical activity. The summary measures were reported as relative risk or as mean difference with 95% confidence intervals. The primary outcome was the incidence of preterm birth <37 weeks.
Tabulation, Integration, and Results
Of the 2059 women included in the meta-analysis, 1022 (49.6%) were randomized to the exercise group and 1037 (50.4%) to the control group. Aerobic exercise lasted about 35–90 minutes 3–4 times per week. Women who were randomized to aerobic exercise had a similar incidence of preterm birth of <37 weeks (4.5% vs 4.4%; relative risk, 1.01, 95% confidence interval, 0.68–1.50) and a similar mean gestational age at delivery (mean difference, 0.05 week, 95% confidence interval, –0.07 to 0.17) compared with controls. Women in the exercise group had a significantly higher incidence of vaginal delivery (73.6% vs 67.5%; relative risk, 1.09, 95% confidence interval, 1.04–1.15) and a significantly lower incidence of cesarean delivery (17.9% vs 22%; relative risk, 0.82, 95% confidence interval, 0.69–0.97) compared with controls. The incidence of operative vaginal delivery (12.9% vs 16.5%; relative risk, 0.78, 95% confidence interval, 0.61–1.01) was similar in both groups. Women in the exercise group had a significantly lower incidence of gestational diabetes mellitus (2.9% vs 5.6%; relative risk, 0.51, 95% confidence interval, 0.31-0.82) and a significantly lower incidence of hypertensive disorders (1.0% vs 5.6%; relative risk, 0.21, 95% confidence interval, 0.09-0.45) compared with controls. No differences in low birthweight (5.2% vs 4.7%; relative risk, 1.11, 95% confidence interval, 0.72–1.73) and mean birthweight (mean difference, –10.46 g, 95% confidence interval, –47.10 to 26.21) between the exercise group and controls were found.
Conclusion
Aerobic exercise for 35–90 minutes 3–4 times per week during pregnancy can be safely performed by normal-weight women with singleton, uncomplicated gestations because this is not associated with an increased risk of preterm birth or with a reduction in mean gestational age at delivery. Exercise was associated with a significantly higher incidence of vaginal delivery and a significantly lower incidence of cesarean delivery, with a significantly lower incidence of gestational diabetes mellitus and hypertensive disorders and therefore should be encouraged.
Preterm birth is the major cause of perinatal mortality in the United States. In the past, pregnant women have been advised against exercise because of presumed risks of pregnancy loss and preterm birth, possibly because of reduced placental circulation. Physical activity has been theoretically related to preterm birth because it increases the release of catecholamines, especially norepinephrine, which might stimulate myometrial activity.
Conversely, exercise may reduce the risk of preterm birth by other mechanisms such as decreased oxidative stress or improved placenta vascularization, an adaptive response to intermittent reduction in uterine blood flow, as well as increased blood volume found in pregnant women during exercise. Physical activity during pregnancy may be decreased because of a lack of time, lack of energy, discomfort or pain, and concern about the baby’s health. In fact, bed rest is commonly recommended in pregnancy. Therefore, the safety of exercise regarding preterm birth, and its effects on gestational age at delivery, remain controversial.
The aim of this systematic review and meta-analysis was to evaluate the effects of exercise during pregnancy on the risk of preterm birth.
Materials and Methods
Search strategy
This meta-analysis was performed according to a protocol recommended for systematic review. The review protocol was designed a priori defining methods for collecting, extracting, and analyzing data. The research was conducted using MEDLINE, EMBASE, Web of Sciences, Scopus, ClinicalTrial.gov , OVID, and Cochrane Library as electronic databases. The trials were identified with the use of a combination of the following text words: exercise or physical activity and pregnancy and preterm birth or preterm delivery and randomized trial as publication type, from the inception of each database to April 2016. Review of articles also included the abstracts of all references retrieved from the search.
Study selection
Selection criteria included only randomized clinical trials of pregnant women randomized to an exercise regimen or not. We included only randomized clinical trials reporting preterm birth as an outcome. Types of participants included women with uncomplicated, singleton pregnancies without any obstetric contraindication to physical activity.
In all the trials, the intervention group participated in planned aerobic exercise. In the control group, women did not participate in exercise sessions and only attended regular scheduled obstetric visits. When possible, data only on women with normal body mass index (18.5–24.9 kg/m 2 ) were selected. Randomized clinical trials including only underweight (body mass index ≤18.5 kg/m 2 ) or only overweight or obese (body mass index ≥25 kg/m 2 ) women, those including diet, counseling, and/or weight monitoring, and those assessing reduction in exercise, were excluded. Quasirandomized trials (ie, trials in which allocation was done on the basis of a pseudorandom sequence (eg, odd/even hospital number or date of birth, alternation) were also excluded.
Data extraction and risk of bias assessment
The risk of bias in each included study was assessed by using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions . Seven domains related to risk of bias were assessed in each included trial because there is evidence that these issues are associated with biased estimates of treatment effect including the following: (1) random sequence generation; (2) allocation concealment; (3) blinding of participants and personnel; (4) blinding of outcome assessment; (5) incomplete outcome data; (6) selective reporting; and (7) other bias. Review authors’ judgments were categorized as low risk, high risk, or unclear risk of bias.
All analyses were done using an intention-to-treat approach, evaluating women according to the treatment group to which they were randomly allocated in the original trials. The primary outcome was the incidence of preterm birth at <37 weeks. Secondary outcomes were gestational age at delivery, spontaneous vaginal delivery, operative vaginal delivery, cesarean delivery, gestational diabetes, hypertensive disorders (defined as gestational hypertension or preeclampsia), and neonatal outcomes including birthweight and low birthweight (ie, birthweight <2500 g).
We assessed the primary outcome (ie, incidence of preterm birth <37 weeks) in a sensitivity analysis according to the risk of bias of the included trials and in subgroup analysis according to the type and length of exercise.
Data analysis
Data analysis was completed using Review Manager 5.3 (The Nordic Cochrane Center, Cochrane Collaboration, 2014; Copenhagen, Denmark). Statistical heterogeneity between studies was assessed using the Higgins I 2 statistics. In case of statistical significant heterogeneity (I 2 ≥0), the random effects model of DerSimonian and Laird was used to obtain the pooled risk ratio estimate; otherwise, in case of no inconsistency in risk estimates (I 2 = 0), a fixed-effect model was used.
The summary measures were reported as relative risk or as mean difference with 95% confidence intervals. Potential publication biases were assessed graphically by using the funnel plot and statistically by using Begg’s and Egger’s tests. A value of P < .05 was considered statistically significant.
The meta-analysis was reported following the Preferred Reporting Item for Systematic Reviews and Meta-Analyses statement. Before data extraction, the review was registered with the International Prospective Register of Systematic Reviews (PROSPERO, registration number CRD42016037841).
Three authors (D.D.M., E.R.M.-M., G.S.) independently assessed inclusion criteria, risk of bias, data extraction, and data analysis. Disagreements were resolved by discussion with a fourth reviewer (V.B.). Data from each eligible study were extracted without modification of original data onto custom-made data collection forms. Differences were reviewed and further resolved by common review of the entire process. Data not presented in the original publications were requested from the principal investigators.
Results
Study selection and study characteristics
Figure 1 shows the flow diagram (Preferred Reporting Item for Systematic Reviews and Meta-Analyses template) of information derived from a review of potentially relevant articles. Nine randomized clinical trials, including 2059 sedentary women with an uncomplicated, singleton pregnancy, were included in the meta-analysis. One study was published in abstract form only.

The quality of randomized clinical trials included in our meta-analysis was assessed by the Cochrane Collaboration’s tool. All the included studies, except one, used a computer-generated table of random numbers and had a low risk of bias in incomplete outcome data. No method of blinding as to the group allocation was reported ( Figure 2 ). Figure 3 shows the funnel plot for the primary outcome for assessing publication bias; the symmetric plot suggests no publication bias. Publication bias, assessed using Begg’s and Egger’s tests, was not significant ( P = .48 and P = .51, respectively). Unpublished data were kindly provided by an author.
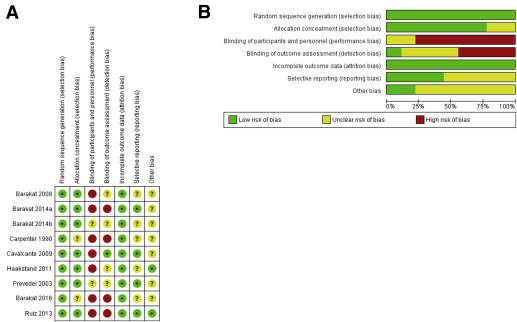
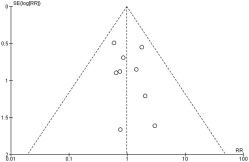
Table 1 shows the characteristics of the included trials. In 5 trials, women were randomized during the first trimester; in 4 studies, women were randomized during the early second trimester (≤22 weeks). Table 2 shows inclusion and exclusion criteria of these trials. Characteristics of the women included are reported in Table 3 .
| Study | Carpenter et al, 1990 | Prevedel et al, 2003 | Barakat et al, 2008 | Calvalcante et al, 2009 | Haakstad et al, 2011 | Ruiz et al, 2013 | Barakat et al, 2014 | Barakat et al, 2014 | Barakat et al, 2016 |
|---|---|---|---|---|---|---|---|---|---|
| Study location | United States | Brazil | Spain | Brazil | Norway | Spain | Spain | Spain | Spain |
| Sample size a | 14 (7 vs 7) | 41 (22 vs 19) | 142 (72 vs 70) | 71 (34 vs 37) | 105 (52 vs 53) | 687 (335 vs 352) | 200 (107 vs 93) | 290 (138 vs 152) | 513 (257 vs 256) |
| GA (wks) at randomization Mean ± SD or WR | 20–22 | 16–20 | 12–13 | 16–20 | 17.3 ± 4.1 vs 18.0 ± 4.3 | 5–6 | 6–7 b | 8–10 | 9–11 |
| Type of exercise | 30 min of physical training preceded and followed by 30 min of cycle ergometry at 60% maximum VO 2 | Hydrotherapy exercises: stretching; resistance, targeted, respiratory exercises in an indoor swimming pool with water at 28–32°C | Stretching; toning and joint mobilization exercises; resistance exercises | Water aerobics in an indoor swimming pool with water at 28–30°C | Aerobic dance followed by abdominal, pelvic floor and back muscle training, stretching, relaxation, and body awareness exercises | Aerobic, resistance, and stretching exercises | Walking and stretching followed by toning and joint mobilization exercises, aerobic dance, and specific exercises for leg, buttocks, and abdomen | Toning, joint mobilization, and resistance exercises preceded and followed by walking and light stretching | Aerobic exercise, aerobic dance, muscular strength, and flexibility exercises preceded by walking and light stretching and followed by relaxation and pelvic floor exercise |
| Duration of a single session, min | 90 | 60 | 35 | 50 | 60 | 50–55 | 55–60 | 55–60 | 50–55 |
| Times per week, number of days | 4 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| Intensity of exercise (HR) | NR | NR | <80% of their age-predicted maximum HR | <70% of their age-predicted maximum HR | NR | <60% of their age-predicted maximum HR | <60% of their age-predicted maximum HR | <60-75% of their age-predicted maximum HR | <70% of their age-predicted maximum HR |
| Self-reported intensity of exercise, Borg scale c | NR | NR | NR | NR | 12–14 | 10–12 | 12–13 | NR | 12–14 |
| Control group | 10 wks of nonexercise | No hydrotherapy program | No exercise, except those activities necessary for daily living | No regular physical activity during the entire pregnancy | Women were neither encouraged nor discouraged from exercising | Regular scheduled visits, every 4–5 wks until the 35th wk of GA, then weekly until delivery. Women received general nutrition and physical activity counseling and were not discouraged from exercising. | No exercise during pregnancy | NR | General advice from their health care provider about positive effects of physical activity; regular scheduled visits; women not discouraged from exercising on their own and asked by telephone about their exercise once each trimester |
| Primary outcome | Change in resting heart rate; exercise stroke volume; exercise VO 2 ; O 2 pulse | Maternal outcomes: body composition and cardiovascular capacity; perinatal outcomes: weight and prematurity | Healthy gravidae and GA at delivery | Evolution of pregnancy (GA at delivery, preterm birth), maternal body composition (weight gain, BMI, proportion of fat mass), and perinatal outcomes (Apgar score, weight at birth, and birthweight adequate for GA) | Infant birthweight | Maternal weight gain | Maternal (GA, preterm birth, blood pressure, weight gain, type of delivery, GDM) and fetal (birthweight, head circumference, birth size, Apgar score, pH of umbilical cord, sex) outcomes | GA at delivery | Gestational hypertension |
| Other comments | Physical training only 10 wks in midpregnancy | — | — | — | In addition to joining the scheduled exercise sessions, all women in the exercise group were asked to include 30 min of moderate self-imposed physical activity on the remaining weekdays | Sample size refers to only normal-weight women included in the original trial | — | — | Sample size refers to only normal-weight women included in the original trial |
a Data are presented as total number (number in the intervention group vs number in the control group)
b Pregnant women who underwent their first ultrasound examination at 10–12 weeks were offered the opportunity to participate, following a randomization process
c Borg scale is a 15 category scale (from 6 to 20) to measure the level of perceived exertion. Light exercise is about 6–11; 13 somewhat hard; 15 hard; 19 extremely hard.
| Study | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Carpenter et al, 1990 | Sedentary, pregnant women | Not reported |
| Prevedel et al, 2003 | Nulliparous with singleton, uncomplicated gestations | Any medical or obstetrical contraindication |
| Barakat et al, 2008 | Women with singleton, uncomplicated gestations, not at high risk of preterm delivery | Any obstetric contraindication to exercise suggested by ACOG; not planning to give birth in the same obstetrics hospital department; not to be under medical follow-up throughout the entire pregnancy; any serious medical condition |
| Calvalcante et al, 2009 | Low-risk, sedentary pregnant women with uncomplicated, singleton gestations | History of 2 or more cesarean deliveries; medical conditions contraindicating the practice of physical exercise and/or practical impediments |
| Haakstad et al, 2011 | Nulliparous women with uncomplicated, singleton gestations whose prepregnancy exercise levels did not include participation in a structured exercise program; ability to read, understand, and speak Norwegian; to be within the first 24 wks of pregnancy | History of more than 2 miscarriages, severe heart disease, and persistent bleeding after 12 wks of gestation; multiple pregnancy; poorly controlled thyroid disease; gestational hypertension or preeclampsia; diabetes or gestational diabetes |
| Ruiz et al, 2013 | Sedentary women with singleton, uncomplicated gestations, not at high risk of preterm delivery, and not participating in any other trial | Any obstetric contraindication to exercise suggested by ACOG |
| Barakat et al, 2014 | Women with uncomplicated, singleton gestations | Any obstetric contraindication to exercise suggested by ACOG; not planning to give birth in the obstetrics department of the study; not receiving medical follow-up throughout pregnancy; participating in another physical program or having a high level of pregestational physical exercise |
| Barakat et al, 2014 | Women with uncomplicated, singleton gestations | Any obstetric contraindication to exercise suggested by ACOG; not planning to give birth in the obstetrics department of the study; not receiving medical follow-up throughout pregnancy; participating in another physical program or having a high level of pregestational physical exercise |
| Barakat et al, 2016 | Women with uncomplicated, singleton gestations | Any obstetric contraindication to exercise suggested by ACOG; not planning to give birth in the obstetrics department of the study; not receiving medical follow-up throughout pregnancy; history of risk of preterm birth |
| Characteristics | Carpenter et al, 1990 | Prevedel et al, 2003 | Barakat et al, 2008 | Calvalcante et al, 2009 | Haakstad et al, 2011 | Ruiz et al, 2013 | Barakat et al, 2014 | Barakat et al, 2014 | Barakat et al, 2016 |
|---|---|---|---|---|---|---|---|---|---|
| Maternal age, y, mean ± SD | NR | 20 | 30.4 ± 2.9 vs 29.5 ± 3.7 | 25.8 ± 4.6 vs 24.4 ± 5.8 | 31.2 ± 3.7 vs 30.3 ± 4.4 | 31.6 ± 4 vs 31.9 ± 4 | 31.57 ± 3.87 vs 31.51 ± 3.92 | 31.4 ± 3.2 vs 31.7 ± 4.5 | 31.6 ± 4.2 vs 31.8 ± 4.5 |
| Parity | |||||||||
| 0 | NR | NR | 72.2% vs 57.1% | 47.1% a vs 62.2% a | NR | NR | 60.7% vs 53.9% | 60.9% vs 54.6% | 67.8% vs 59.8% |
| 1 | NR | NR | 22.2% vs 35.7% | NR | NR | NR | 34.6% vs 40.4% | 33.3% vs 39.5% | 26.2% vs 33.2% |
| >1 | NR | NR | 5.6% vs 7.1% | NR | NR | NR | 4.7% vs 5.6% | 2.9% vs 5.9% | 6% vs 7.1% |
| Occupation | |||||||||
| Sedentary | NR | NR | 26/72 (36.1%) vs 21/70 (30%) | NR | 37/52 (71.2%) vs 36/53 (67.9%) | 195/476 (41%) vs 184/477 (38.6%) | NR | 58/138 (42%) vs 68/152 (44.7%) | 171/382 (44.8%) vs 148/383 (38.6%) |
| Housewife | NR | NR | 31/72 (43.1%) vs 30/70 (42.9%) | NR | NR | 126/476 (26.5%) vs 118/477 (24.7%) | NR | 25/138 (18.1%) vs 33/152 (21.7%) | 72/382 (18.9%) vs 93/383 (24.3%) |
| Active | NR | NR | 15/72 (20.8%) vs 19/70 (27.1%) | NR | NR | 155/476 (32.5%) vs 175/477 (36.7%) | NR | 55/138 (39.9%) vs 51/152 (33.6%) | 139/382 (36.4%) vs 142/383 (37.1%) |
| Daily smokers, % | NR | 10% (overall smoking index) | 16/72 (22.2%) vs 20/70 (28.6%) | NR | 2/52 (3.8%) vs 1/53 (1.9%) | NR | 11/107 (10.3%) vs 12/89 (13.5%) | 18/138 (13%) vs 29/152 (19.1%) | 40/382 (10.5%) vs 54/383 (14.1%) |
| Prepregnancy BMI, mean ± SD | NR | NR | 24.3 ± 0.5 vs 23.4 ± 0.5 | 24.1 ± 4.5 vs 23.4 ± 3.8 | 23.8 ± 3.8 vs 23.9 ± 4.7 | 23.7 ± 3.9 vs 23.5 ± 4.2 | 23.8 ± 4.4 vs 24.1 ± 4.3 | 24.0 ± 4.3 vs 23.6 ± 4 | 23.6 ± 3.8 vs 23.4 ± 4.2 |
| Prepregnancy BMI, % | NR | NR | NR | NR | NR | <18.5 b 11/480 (2.3%) vs 24/482 (5%) ≥18.5-24.9 b 323/480 (67.3%) vs 329/482 (68.2%) ≥25-29.9 b 111/480 (23.1%) vs 92/482 (19.1%) ≥30 b 35/480 (7.3%) vs 37/482 (7.7%) | <18 b 1/106 (0.9%) vs 2/90 (2.2%) ≥18-24.9 b 73/106 (68.9%) vs 58/90 (64.5%) ≥25-29.9 b 25/106 (23.6%) vs 21/90 (23.3%) ≥30 b 7/106 (6.6%) vs 9/90 (10%) | NR | <18.5 b 10/382 (2.6%) vs 20/383 (5.2%) ≥18.5-24.9 b 258/382 (67.5%) vs 259/383 (67.6%) ≥25-29.9 b 89/382 (23.3%) vs 75/383 (19.6%) ≥30 b 25/382 (6.5%) vs 29/383 (7.6%) |
| Prior PTB | NR | NR | 2.8% vs 4.3% | NR | NR | 0% vs 0% | NR | 5.8% VS 3.9% | 0% vs 0% |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


