Examination of the Newborn Infant
Joseph A. Zenel
GENERAL EXAMINATION
 INITIAL AND SUBSEQUENT ASSESSMENTS
INITIAL AND SUBSEQUENT ASSESSMENTS
Immediately after birth, all infants should be briefly examined for major congenital abnormalities, signs of serious illness, or discrepancy between expected gestational age and weight for gestation. The number of nursing evaluations in the next few hours depends on anticipated problems and should focus on heart rate, respiratory rate and effort, temperature, skin perfusion, skin color, and neuromuscular activity. Observation of the first feeding, usually within 4 hours of birth, indicates any underlying difficulty with sucking and swallowing. If no abnormalities are noted at birth, further newborn observation should occur at least every 8 hours. Any abnormalities detected at any time warrant more frequent, thorough examinations and possible investigation and initial therapy.
All infants should undergo a detailed medical examination within 24 hours of birth to ensure that investigation, treatment, or preventive management, when indicated, is implemented as soon as possible and to answer any concerns that a parent may have. Reassurance to a mother (or guardian) shortly after delivery is immensely important regardless of maternal experience with deliveries.1 Further detailed examinations are necessary if any neonatal problems are detected; infants discharged early, before 24 hours, should be reexamined by 3 to 4 days of age.
 PRINCIPLES
PRINCIPLES
The neonatal examination is best performed in an appropriately equipped, warm, draft-free room, preferably with the mother present; examining the infant under a servocontrolled radiant warmer is an alternative. Thorough hand-washing before and after handling each infant is essential to prevent the spread of pathogenic organisms. If possible, the infant’s mother or guardian should be present during the examination so the examiner may address any specific parental concerns or questions and observe parental-infant interaction. Observation of the infant’s appearance, posture, and state of consciousness should precede the formal aspects of palpation and auscultation. Presence of 1 anomaly suggests presence of another, since anomalies often coexist. Constellations of physical findings may indicate the presence of a syndrome. Evidence of trauma in one part of the baby should lead to a search for trauma in other areas. Signs of birth trauma are particularly common in large infants and in infants who underwent difficult deliveries such as breech or forceps delivery.
The obstetric history of the pregnancy and delivery may provide a clue or sign of possible neonatal problems. For example, polyhydramnios may signal bowel obstruction; oligohydramnios may signal renal anomalies and pulmonary insufficiency; small-for-gestational-age and postmature infants are suspect for hypoglycemia and polycythemia; and prolonged rupture of the membranes, maternal fever, and fetal tachycardia may signal neonatal sepsis. The neonatal consequences of intrauterine growth restriction, prematurity, multiple births, maternal diabetes, and meconium-stained amniotic fluid are discussed in detail in other sections.
 GESTATIONAL AGE AND SIZE
GESTATIONAL AGE AND SIZE
The infant’s gestational age should be estimated and body size compared with appropriate normal standards.
There are several ways to estimate gestational age, including reliable maternal history (based on known first day of the last menstrual period and regular pattern of menstruation before conception), prenatal ultrasound scan taken before 20 weeks of gestation, and physical characteristics of the skin, external genitalia, ears, breasts, and neuromuscular behavior of the newborn infant (Fig. 44-1).2-4Preterm (or premature) infants have less than 37 completed weeks of gestation, term infants have completed 37 to 42 weeks, and postterm (or postmature) infants are past 42 weeks of gestation.
Birth weight, occipitofrontal head circumference, and crown-to-heel length should be measured and recorded. Length is measured from vertex to heel with the infant’s legs fully extended. These measurements are then compared for gestational age against standard growth charts (Fig. 44-2).5 Ideally, growth charts for the specific population should be used. Babies born to mothers living at high altitude are smaller than babies born at or near sea level. An infant is considered to be appropriate for gestational age if it falls within 2 standard deviations of the mean on these charts.6 Infants who are more than 2 standard deviations below the mean are small for gestational age, and those more than 2 standard deviations above the mean are large for gestational age. Both groups need special observation7 (see Chapters 47 and 48). Twenty percent of infants with serious congenital malformations are small for gestational age.8
 GENERAL INSPECTION
GENERAL INSPECTION
Most babies born at term cry at birth, quickly establish normal regular breathing, and may remain awake and quite active for 30 minutes or more, during which the eyes are open; they make sucking, chewing, and swallowing movements; and they may have bursts of flexion and extension of the arms and legs with facial grimaces. This activity may be continuous or interspersed with quiet periods. Following the first few hours after birth, the normal term baby spends approximately 80% of the time in active or quiet sleep. The remaining 20% of the time is spent awake in varying states of activity with or without crying.
When the infant cries, the cry should be vigorous. A weak or whimpering cry is abnormal and warrants closer examination of the baby. A high-pitched or shrieking cry suggests an underlying neurologic problem. A hoarse cry may result from vocal cord paralysis, hypothyroidism, or trauma to the hypopharynx.
Initially, infants often adopt a position similar to that assumed in utero (eFig. 44.1  ). Placing a crying infant into this posture often calms the infant. About 2% of infants have significant deformities caused by mechanical forces that acted in utero to restrict motion or to create pressure on the limbs, spine, thorax, or skull. Mechanical forces include oligohydramnios, uterine malformations, or multiple pregnancies.
). Placing a crying infant into this posture often calms the infant. About 2% of infants have significant deformities caused by mechanical forces that acted in utero to restrict motion or to create pressure on the limbs, spine, thorax, or skull. Mechanical forces include oligohydramnios, uterine malformations, or multiple pregnancies.
 TEMPERATURE
TEMPERATURE
The normal infant is pink, well-perfused, and feels warm to the touch, but exposure to even a moderately cold environment leads to the hands and feet quickly becoming cool and slightly cyanotic. The normal axillary temperature is between 36.5 °C and 37.4 °C. The most common reasons for a low or high temperature are exposure to a cool environment and overheating (see Chapter 43). However, persistence of an abnormal temperature in a normal thermal environment indicates underlying pathology. Hypothermia may also occur with hypoglycemia, hypoxia, or hypothyroidism. Hyperthermia can be seen during drug withdrawal and with intracranial or adrenal hemorrhage.
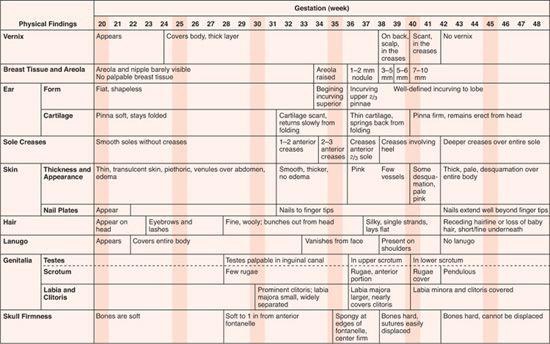
FIGURE 44-1. Examination: First hours of life. (Source: Adapted from Kempe C, Silver H, O’Brien D, eds. Current Pediatric Diagnosis and Treatment. 3rd ed. Los Altos, CA: Lange; 1974.)
 SKIN
SKIN
Gestational Changes
Fine, soft, lanugo hair covers the entire body in very preterm infants and disappears from the face and lower back between 32 and 37 weeks. The term infant has lanugo hair on the upper back and dorsal aspects of the limbs. Vernix caseosa, a thick white material with the consistency of soft cheese, covers the skin of the entire body until 35 to 37 weeks. By term, the amount of vernix has decreased so that it is present mainly in the flexor creases. Also by term, the subcutaneous tissue is relatively thick, and the fingernails and toenails are fully formed and extend slightly beyond the ends of the digits. If fetal hypoxia occurs at term, meconium may be passed into the amniotic fluid. If meconium has been in the amniotic fluid for several hours, it will also stain the skin, fingernails, toenails, and umbilical cord with a greenish hue. Fetuses at less than 34 weeks of gestation rarely pass meconium in response to hypoxia. The postmature infant (beyond 42 weeks) may have a somewhat wasted appearance with dry, peeling skin, a decreased amount of subcutaneous tissue, long fingernails, and an alert appearance.
Skin Abnormalities
A neonatal rash may also indicate a serious systemic infection. Intrauterine infections may present with thrombocytopenic purpura. A red maculopapular rash may occur with toxoplasmosis. Congenital rubella often produces macular or slightly raised purple lesions, called a “blueberry muffin” rash. Herpes simplex can cause a few vesicles or a generalized vesicobullous eruption with an erythematous base; these cutaneous lesions may precede disseminated disease or may appear following the onset of disease in other organs. Congenital syphilis may cause a pink, maculopapular rash that later turns brown or becomes vesicobullous and hemorrhagic. Syphilitic rashes commonly involve the palms or soles. Staphylococcal infection may appear as pustules, generalized erythema, or extensive bullous eruptions (termed scalded skin syndrome, toxic epidermal necrolysis, or Ritter disease). Listeria monocytogenes can produce purple, miliary granulomas of the skin. Cutaneous moniliasis often produces macerated, erythematous skin, usually in the diaper area, and often occurs in infants treated with antibiotics. Many of these skin lesions contain viable organisms (eg, syphilis, herpes, Staphylococcus) and are highly infectious. Some generalized viral infections are characterized by small red papules that contain infiltrations of erythroid cells.
The normal newborn often has some form of benign skin lesion. These neonatal skin abnormalities include congenital absence of skin (aplasia cutis), rashes, erythroderma, vesicles, pustules, bullae, purpura, and petechiae are discussed in Chapter 357. Pigmented skin lesions and nevi are discussed in Chapter 361, vascular lesions in Chapter 364 and other genetic skin disorders in Chapter 360.
Color
Pallor may result from anemia or poor perfusion. With poor perfusion from vasoconstriction or low cardiac output, capillary filling after blanching of the skin over the tibia is delayed (> 3 sec). In pigmented babies, poor perfusion is more readily detected by delayed capillary filling after blanching of the toes or fingers. Pallor of mucous membranes in these infants suggests anemia. A generalized gray hue may indicate acidosis. Pale, mottled skin occurs with sepsis or hypothermia. There may be cyanosis of the hands and feet (acrocyanosis), which is normal immediately after birth or if the infant has been exposed to a cold environment. Generalized cyanosis occurs with significant arterial hypoxemia as well as with methemoglobinemia. Plethora may indicate polycythemia. Harlequin skin describes a transient change in the skin color: one side of the body turns pale while the other side remains pink with a sharp line of demarcation in the midline. Harlequin change can last for seconds or a few minutes and may recur but is of no known pathologic significance.
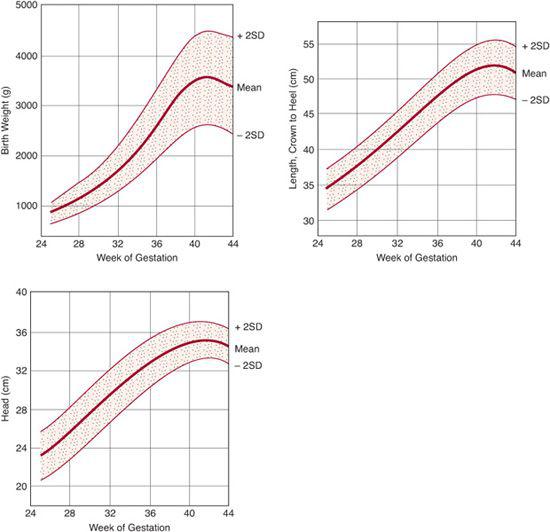
FIGURE 44-2. Intrauterine growth charts showing the normal values of body weight, length, and head circumference for infants born at different gestational ages at sea level (Montreal). (Source: From the data of Usher R, McLean F. Intrauterine growth of live-born Caucasian infants at sea level: standards obtained from measurements in 7 dimensions of infants born between 25 and 44 weeks of gestation. J Pediatr. 1969;74:901-910.)
Ecchymoses generally result from birth trauma and are often present over the head after vertex delivery or on the feet, lower limbs, and buttocks following breech delivery. With severe birth trauma, there can be extensive hemorrhage into the muscles underlying areas of bruised skin. Localized petechiae are usually found in areas of vascular stasis or compression that occurred during delivery, on the face after a vertex delivery, or on the lower limbs after a breech delivery. More generalized petechiae suggest thrombocytopenia.
The skin overlying an area of subcutaneous fat necrosis often appears red. The subcutaneous tissue is hard and sharply demarcated, with lesions most common on the cheeks, buttocks, limbs, or back.
Neonatal jaundice, with a yellow skin color, is caused by an elevation in indirect-reacting bilirubin. Elevation of direct-reacting bilirubin gives a yellow-to-green discoloration. It is easier to assess jaundice in a newborn by briefly pressing on the infant’s skin with a finger and observing the color in the blanched area. This is of particular value in pigmented infants. The normal newborn commonly develops mild physiologic jaundice between days 2 and 4 after birth. Jaundice in the first day warrants prompt investigation; it is usually from sepsis or hemolytic anemia. The differential diagnosis of neonatal jaundice is discussed in Chapter 53.
 HEAD
HEAD
Scalp hair of the infant is fine and silky. The head shape differs in infants who were in vertex or breech positions. After vertex presentation and vaginal delivery, there can be pronounced vertical elongation of the head. Breech infants often have occipital-frontal head elongation, with a prominent occipital shelf.
The cranial sutures should be palpably open and may be separated by up to several millimeters. Temporary overlap of bones, due to molding, should be distinguished from craniosynostosis (premature closure of a suture). If a suture closes in utero, it prevents growth of the skull perpendicular to the fused suture line, resulting in a sustained, abnormal skull configuration. In contrast, after molding occurs, the bones return to their normal positions in a few days, sometimes with a small concomitant decrease in head circumference.
Normally, the anterior fontanelle is open, soft, and flat; mean diameter is less than 3.5 cm. The posterior fontanelle is often fingertip size or just palpably open. A bulging or tense fontanelle, with separation of the bony sutures, indicates increased intracranial pressure.11
Caput succedaneum is edema of the scalp caused by local pressure and trauma during labor. With severe trauma, there may be extensive subgaleal hemorrhage under the galea aponeurotica. The scalp is tensely distended, and the swelling may extend to the suboccipital region and push the ears laterally. Hemorrhage can be massive and produce shock. Cephalohematomas are subperiosteal hemorrhages caused by the trauma of labor and usually involve the parietal or occipital bones. Cephalohematomas are fairly firm, fluctuant masses with a palpable rim that gives the impression of a shallow crater in the bone under the mass. They are distinguished from caput succedaneum because they do not extend beyond the suture lines of the affected bone. Parietal bone cephalohematomas may be bilateral but are palpably distinct from one another. Cephalohematomas should not be aspirated; they gradually resorb but can calcify before disappearing. Trauma to the head may also be accompanied by more serious intracranial hemorrhage. Other common traumatic scalp lesions include puncture wounds from fetal monitor electrodes and fetal scalp blood gas sampling. A circular hematoma may be seen at the site of application of a vacuum extractor.
 FACE
FACE
The newborn’s face often gives the first clue to the presence of a dysmorphic syndrome. There may be obvious malformations, such as cleft lip or the characteristics of the Pierre Robin sequence characterized by a small mandible (micrognathia), a high-arched or cleft palate, and a tongue that falls back into the hypopharynx (glossoptosis); this causes airway obstruction, which must be recognized promptly and can be relieved with an oral airway and by pulling the tongue or the mandible forward. Infants with fetal alcohol exposure may be more difficult to identify but may have growth deficiency, microcephaly, maxilla hypoplasia, and short palpebral fissures.
Intrauterine position may cause asymmetry of the face. Pressure over the stylomastoid foramen during labor and delivery may cause a peripheral facial paralysis, which is most obvious during crying. The paralysis usually resolves and should be distinguished from congenital absence of the depressor anguli oris muscle, which also results in an asymmetric crying facies.
Fracture of the zygomatic arch can occur during labor and delivery; this is detectable by palpation. Forceps often leave bruises on the face, usually in the shape of the forceps blade (see eFig. 44.2  ).
).
 EYES
EYES
Newborns generally open their eyes to permit inspection when they are awake, held upright, and shaded from bright light. An infant who is quiet and alert during the examination will fix on the examiner’s face and follow it, at least part way, as the examiner moves slowly from side to side.
Congenital lid ptosis will manifest itself as a drooping lid. Failure to close the eye fully can occur with facial paralysis. Horner syndrome, caused by lower brachial plexus injury, appears as ptosis, miosis, and enophthalmos. Congenital microphthalmia is usually obvious on inspection and palpation. Mass lesions, such as orbital tumors, hemangiomas, and encephaloceles, may be immediately apparent. Proptosis may be due to mass lesions or retrobulbar hemorrhage.
Birth trauma may also cause subconjunctival hemorrhages or hemorrhages in the anterior chamber, vitreous, and retina. Forceps deliveries can result in lacerations of the lid or globe. A rupture of the Descemet membrane in the cornea may become apparent because of corneal clouding.
Congenital glaucoma initially appears as an enlarged cornea that becomes progressively cloudy. A corneal diameter of 11 mm or more is suspect and warrants further investigation, as early detection is important in preventing eye damage.
Ophthalmoscopic examination should begin by focusing on the anterior portion of the eye and then progressing back to the retina. This allows detection of anterior lesions, such as cataracts and colobomas (defects) of the iris, which may occur alone but are often components of various dysmorphic syndromes. The iris is blue or blue-gray in fair-skinned babies but is dark gray to brown in darker pigmented infants. In fair babies, a red reflex is transmitted back through the lens, whereas in darker infants a paler orange-tan color may be seen. Visualizing retinal vessels verifies focusing on the retina. A cataract will appear as a black opacity that interferes with light transmission through the lens. A white pupillary reflex is abnormal and may occur with a large retinoblastoma or developmental abnormalities such as retinal coloboma, retinopathy of prematurity, and persistent hypoplastic primary vitreous. A family history of retinoblastoma warrants a thorough ophthalmologic examination to exclude small or peripheral tumors.
Conjunctivitis usually becomes apparent after the second day of life; common pathogens include Staphylococcus aureus, streptococci, and coliform bacteria. Gonococcal conjunctivitis is acquired from the birth canal and can progress rapidly to a panophthalmitis with eye destruction. Inclusion blennorrhea is also acquired from the mother’s birth canal; it is caused by Chlamydia trachomatis and typically appears toward the end of the first week of life. The various causes of conjunctivitis must be distinguished from one another by Gram stain and appropriate cultures (see Chapter 588).
 EARS
EARS
At term, the ears are well formed and contain sufficient cartilage to retain a normal shape and resist deformation. Preauricular pits are common and inherited in an autosomal dominant pattern; preauricular skin appendages also may be seen. When preauricular skin appendages are hereditary, they may be associated with deafness. Malformed auricles or low-set ears are found in many dysmorphic syndromes and are associated with urogenital malformations.
Gently pulling the pinna back and down aids examination of the ear canal and tympanic membrane. The tympanic membrane sharply angles back more in an infant than in an older child and is located more superiorly in relation to the external canal. Otitis media is uncommon but should be considered in an infant suspected of having an infection in the first days after birth. A crude estimate of hearing can be obtained if the infant is quiet and the examination is done in an environment without distracting noise. The alert, normal newborn will turn toward human speech and startle to a loud noise.
 NOSE
NOSE
Most newborn infants are nose breathers; rarely, obstructive lesions or foreign bodies in the nose can be lethal. Initially, an infant will become cyanotic and have respiratory difficulty but, if stimulated to cry, will breathe through the mouth. Occasional sneezing is the normal mechanism infants use to clear the nose. Nasal patency can be verified by checking each naris for a good airstream with a thin strip of tissue or cotton. To avoid confusion, the mouth may need to be occluded transiently. Unilateral or bilateral anatomic obstruction from choanal atresia is rare. When there is doubt, a thin catheter should be passed gently through each nostril into the hypopharynx. Masses, such as an encephalocele protruding into the nasopharynx, can also cause obstruction. Nasal stuffiness can occur as a result of retained mucus or trauma. Nasal stuffiness may be a sign of drug withdrawal.
 MOUTH
MOUTH
Examination of the mouth of the newborn infant includes inspection and palpation. A cleft palate may not be seen but may be detectable by palpation; a cleft uvula should raise suspicion of a palatal defect. Small, shiny white masses on the gums (epithelial pearls) are common. White Epstein pearls are found in the midline on the roof of the mouth, at the junction of the hard and soft palate. A ranula is a small benign mass (mucocele) that arises from the floor of the mouth. A high-arched or narrow palate is found in many dysmorphic syndromes.
The tongue may be attached to a short central frenulum; this rarely interferes with feeding or future function. An enlarged or protruding tongue can be seen with hemangiomas, isolated macroglossia, hypothyroidism, or in Down and Beckwith syndromes. Infants with Pierre Robin sequence have relative macroglossia because of a small mandible.
The normal, awake newborn will usually suck vigorously on a finger placed in the mouth. With normal effective sucking, the finger is actively drawn into the mouth by the movement of the tongue against the palate in a forward-to-backward motion. This coordinated function is easily distinguished from disorganized biting movements, which are ineffective in feeding from the nipple.
Natal teeth, if present, usually erupt in the lower incisor position. These can either be supernumerary teeth or true, deciduous “milk” teeth. If very loose or the cause of painful breast feeding, they may be removed. However, removal of deciduous teeth will leave a defect for 7 years, until the permanent teeth appear, and may alter positioning of the 6-year molars and dental arch.
 NECK
NECK
The neck of the newborn should have a full range of motion; limitation may indicate an abnormality of the cervical spine. Cervical masses, such as a goiter, cavernous hemangioma, or cystic hygroma, may compress the trachea and cause inspiratory obstruction, which may require tracheal intubation beyond the site of obstruction to establish an airway. Brachial cleft anomalies include cysts or sinuses along the anterior edge of the sternocleidomastoid muscle. Thyroglossal duct cysts usually occur in the ventral midline. Torticollis is seen with a tightened sternocleidomastoid muscle on one side and an atretic sternocleidomastoid muscle on the side toward which the head is turned; facial asymmetry is a common accompaniment.
Lateral traction during delivery may damage the upper root of the brachial plexus involving the fifth and sixth cervical roots, resulting in paralysis of the shoulder and arm. The arm is held alongside the body in internal rotation (Erb-Duchenne paralysis). The lower root of the brachial plexus, involving the eighth cervical and first thoracic roots, may be damaged, particularly during breech delivery. The small muscles of the hand are paralyzed, resulting in a clawlike posture (Klumpke paralysis). When there is neck trauma, the cervical sympathetic nerves may be damaged, resulting in an associated Horner syndrome, and the phrenic nerve may be injured, causing diaphragmatic paralysis.
 CHEST
CHEST
The chest of the normal newborn is barrel-shaped, with the xiphoid often prominent. The most frequent birth injury to the thoracic region is fracture of the clavicles, identified by crepitation upon clavicle palpation. Supernumerary nipples are a common minor anomaly; wide spacing of the nipple is seen in Turner syndrome. Breast engorgement may occur in boys or girls and increases over the first few days.
Lungs
The normal respiratory rate is 35 to 60 breaths per minute. Respiratory excursion is most easily judged in the lateral view. Excursion of the abdomen is quite prominent, as infants breathe principally with their diaphragms. With normal breathing, the chest and abdomen move together. When the airway is obstructed or the lungs are stiff, the abdomen appears to enlarge and the chest cage appears to get smaller with inspiration (thoracoabdominal asynchrony). The tissue between the ribs may be pulled in during inspiration; these retractions are normal during the first few minutes after birth. Thereafter, they are usually a sign of increased inspiratory effort from noncompliant lungs or airway obstruction. Inspiratory retractions of the ribs and sternum occur in severe lung disease or occasionally with an abnormal chest wall. Mild expiratory grunting, nasal flaring, and tachypnea occur during the first few minutes after birth. There may also be scattered crackles caused by residual intraalveolar lung fluid that clears rapidly. These signs, attributable to retained lung fluid, are more noticeable after cesarean section. Persistence or worsening of respiratory symptoms may indicate more serious problems, such as respiratory distress syndrome, bacterial pneumonia, meconium aspiration, or cardiac disease.
Chest wall respiratory movement should be symmetric. One side moving less or lagging behind the other suggests an elevated paralyzed diaphragm from phrenic nerve palsy or an intrathoracic mass such as herniation of bowel through a diaphragmatic hernia. However, the absence of such findings does not rule out these lesions. Breath sounds may be heard even when a pneumothorax is present. Coughing in the newborn period is abnormal and usually accompanies interstitial lung disease.
Heart and Vasculature
The point of maximal cardiac impulse is along the left side of the sternum at the fourth to fifth interspace and medial to the midclavicular line. The heart may be displaced if there is a pneumothorax or space-occupying lesion.
The heart rate may be 160 to 180 beats per minute (bpm) during the first few hours after birth. Thereafter, the normal awake heart rate averages 120 to 130 bpm. Occasionally, a normal newborn infant may have heart rates of 80 bpm, which may fall transiently to 60 bpm for short periods. A persistent heart rate below 80 bpm warrants investigation. Conditions associated with bradycardia include birth asphyxia, increased intracranial pressure, hypothyroidism, and heart block. Tachycardia occurs with hypovolemia, fever, drug withdrawal, poor systemic perfusion, tachyarrhythmias, anemia, and hyperthyroidism. Cardiac rhythm should be checked; premature atrial contractions are not uncommon.
Despite the rapid heart rate, heart sounds can be clearly distinguished. The pulmonic component of S2 may be prominent on the first day. Splitting of the second sound is audible along the left upper and midsternum. While postnatal circulatory adjustments are occurring, transient benign murmurs can be heard over the pulmonic area or cardiac apex. Murmurs accompanied by other symptoms, such as cyanosis (see Chapters 49, 483, and 484), poor perfusion, or tachypnea, and murmurs that persist past the first day require further evaluation.
Over the first 12 hours, the mean blood pressure averages 50 to 55 mm Hg in term infants (see Chapter 56). Pulses should be palpable in all 4 extremities, and there should be no delay between brachial and femoral pulses (see Chapter 483).
 ABDOMEN
ABDOMEN
An extremely hollow abdomen suggests absence of some of the normal contents, such as diaphragmatic herniation of the bowel into the chest. Distension occurs with dilatation of the bowel from functional or anatomic obstruction, ascites, intraabdominal blood, or a large mass. If abdominal distension is noted, an oral catheter should be advanced into the stomach for decompression.
Signs of obstruction of the upper gastrointestinal tract include polyhydramnios (excess amniotic fluid), regurgitation, and pooling of secretions in the hypopharynx. When obstruction is suspected, pass a soft catheter into the stomach and aspirate the gastric contents. Bile-stained fluid suggests a high intestinal obstruction. In the most common form of tracheoesophageal fistula, proximal esophageal atresia prevents passage of the tube into the stomach. Pass a radiopaque orogastric catheter and check its course by radiography.
Examine the structures of the abdominal wall. A gap between the abdominal rectus muscles in the midline (diastasis recti), most noticeable with crying, is quite common. There is also often a small defect in the periumbilical musculature of the anterior abdominal wall, which may allow an umbilical hernia; this usually closes as the muscles develop toward the end of the first year. There are several serious possible defects of the anterior abdominal wall including omphalocele and gastroschisis as discussed in Chapters 60 and 396. Absence of the musculature of the anterior abdominal wall (the so-called prune belly infant) is an anomaly associated with urinary tract abnormalities (see Chapter 476).
The umbilical cord normally contains two arteries and one vein, with the vein being larger than the arteries. Approximately 1% of newborns have a single umbilical artery, and 15% of these have 1 or more congenital anomalies, usually involving the nervous, gastrointestinal, genitourinary, pulmonary, or cardiovascular system. Otherwise normal infants with a single umbilical artery rarely have a serious anomaly.12 Remnants of the vitelline (omphalomesenteric) duct may persist and communicate with the umbilicus. If the remnant is a mucosal cyst, there may be umbilical mucus discharge. Persistence of the entire duct will create a fistula with the ileum, and some meconium may exit through the umbilicus. Persistent patency of the urachus results in a sinus extending from the bladder to the umbilicus, with urinary discharge from the umbilicus. A noncommunicating urachal cyst may also develop along the line of the urachus.
Palpation of the abdomen to define the size and shape of the internal organs should be gentle and not be done immediately after a feeding in order to avoid infant aspiration of gastric contents. The edge of the liver is normally felt 1 to 2 cm below the right costal margin. The spleen tip may be palpable but usually no more than 1 cm below the rib margin. In some pathologic conditions, the liver and spleen may be so massively enlarged that their edges are in the pelvis and not initially identified. Renal examination is easiest on the first day, before the bowel is filled with gas. The lower portion of each kidney is normally palpable on each side; the lateral and lower edges can be felt above the level of the umbilicus and lateral to the midclavicular line. The right kidney is situated slightly lower than the left kidney, and the palpable portion of the kidney normally feels about 2 cm wide. Enlarged kidneys may result from hydro-nephrosis, cystic malformation, a neoplasm, or renal vein thrombosis. Over 50% of all abdominal masses in the newborn arise from the genitourinary system. Mass lesions may also be caused by gastrointestinal malformation, neoplasms, or, rarely, neural lesions such as an anterior meningomyelocele.
Traumatic lesions to the abdomen at birth include subcapsular hematoma of the liver, which appears as an enlarging liver, an elevated right diaphragm, and shock when the hematoma ruptures; adrenal hemorrhage, which appears as a discrete palpable mass above the kidney and associated fever; and rupture of the spleen, when splenomegaly has been present in utero, with free blood in the peritoneum.
During the first few postnatal days, the umbilical cord stump dries and then turns brown and brittle. The cord usually falls off between 10 and 14 days, releasing a small amount of opaque, yellowish discharge. Separation after 3 weeks, however, is not uncommon. Delayed separation of the cord, past 3 weeks, often occurs in infants with defective phagocyte function. A small, raw-appearing granuloma at the site of cord separation is termed an umbilical polyp. During the first week, a small amount of erythema at the rim of the umbilical stump is common and of no consequence, but more extensive erythema, a deeper red color, or associated edema may indicate the onset of omphalitis. Omphalitis is a serious infection requiring intravenous antibiotic therapy because of possible spread along the umbilical vein into the portal venous sinus of the liver. Omphalitis may progress to peritonitis or necrotizing fasciitis of the abdominal wall, which often proves fatal despite antibiotic therapy.
 EXTERNAL GENITALIA
EXTERNAL GENITALIA
In preterm female infants, separation of the labia majora may give the illusion that the clitoris is enlarged. In term female infants, the labia majora meet in the midline, covering the rest of the genitalia. It is important to identify the urethra, which is just below the clitoris, and the vagina as distinct orifices; a single orifice or urogenital sinus is abnormal. Normally, the vagina has white secretions secondary to fetal stimulation by maternal hormones. These persist for a week or more and occasionally become tinged with blood several days after birth. Hydrometrocolpos results from an imperforate hymen or from vaginal atresia. It can present as a lower abdominal mass or as a bulging mass protruding through the labia and requires decompression.
The term male newborn has a penis approximately 3 to 4 cm long and a scrotum that is pigmented and has extensive rugae. Penile length less than 2.5 cm is abnormal and requires endocrinologic evaluation. The foreskin should not be forcibly retracted. Penile hypospadias is a common anomaly that can vary from a small ventral cleft at the distal end of the penile urethra to a major ventral defect along the length of the penis. Chordee, a ventral bend in the penis, commonly accompanies hypospadias. Epispadias, a similar defect on the dorsum of the penis, is much less common and is a variant of exstrophy of the bladder.
The testes are usually in the scrotum but, if not fully descended, are often palpable in the upper scrotum or inguinal canal. Unilateral undescended testes cause an asymmetry in the scrotum, with an immature appearance on the affected side. Hydroceles or fluid collections in the remnants of the processus vaginalis cause a swelling of the scrotum. They are common, usually do not communicate with the peritoneal cavity, and disappear gradually. Hydroceles that fluctuate in size or that persist are in communication with the peritoneal cavity and indicate a potential indirect inguinal hernia. Intestinal herniation can occur in the newborn period. Testicular enlargement, with discoloration of the overlying scrotum, suggests a testicular torsion that is a surgical emergency.
Ambiguous genitalia is a problem that requires investigation. Mild masculinization of the female newborn, with some enlargement of the clitoris, usually can be distinguished from mild feminization of the male neonate, with a small penis and hypospadias. When the processes are more extensive, however, the distinction between a girl with a very enlarged clitoris and a partially fused and pigmented labium and a boy with a very small penis and extensive hypospadias and bifid scrotum is much less clear (see Chapter 539).
Trauma to the external genitalia may occur during breech delivery. In addition to ecchymoses, there may be hemorrhage into the testes, scrotum, and pelvic muscles, which generally resolves in a few weeks.
 ANUS
ANUS
Imperforate anus is not always obvious on inspection. A fistula that opens onto the perineum, ventral to the normal anus, may accompany the imperforate anus. However, this fistula will not have the radiating skin creases of a normal anus. There can also be a normal-appearing anal dimple with no opening. Presence of meconium on the perineum and perianal area does not rule out imperforate anus; meconium in the anal area may have been passed by way of the skin fistula or, in a girl, a fistula from the rectum to the vagina.
 SPINE
SPINE
The spine of the newborn is quite flexible in both the dorsoventral and lateral axes; restricted movement suggests vertebral anomalies. The entire length of the spine, including the sacrum, should be palpated for bony defects and asymmetries. A midline abnormality of the skin over the spine, such as a small dimple, tufts of hair, or a pilonidal sinus, warrants close inspection, for any fluid extruding may indicate a tract that can allow bacteria on the skin to reach the cerebrospinal fluid. Midline cutaneous abnormalities may also indicate an occult spina bifida or a diastematomyelia (division of the spinal cord into 2 parts, which may become tethered as the child grows). Neural crest defects of the spine include meningocele, myelomeningocele, and rachischisis. Tumors of the spine, presenting at birth, are usually teratomas (see Chapter 460).
 LIMBS
LIMBS
Trauma and positional deformities secondary to intrauterine position can occur in the newborn. The most common forms of trauma of the limbs include fractures in the shaft of the femur, humerus, or clavicles and injury to the brachial plexus, causing paralysis of the hand and arm (discussed previously under examination of the neck).
It is important to distinguish between joints in one extreme of their normal position and joints that are deformed. As a rule, if simple manual pressure will correct a deformed joint back to its neutral position and a bit beyond, corrective positioning or simple exercise and stretching will correct the deformity. If the deformity cannot be corrected by gentle pressure, orthopedic evaluation is needed.
If the hips are flexed to 90 degrees, the legs normally can be abducted until the knees touch the table the infant is lying on. If this cannot be done, or if the maneuver can be done on one side only, there may be developmental dysplasia of the hip. In this condition, the head of the femur is displaced posteriorly, out of the acetabular fossa. The affected leg may appear shorter. The examiner will feel a click when abducting and adducting the hips in about 10% of all infants. However, only 10% of infants with hip clicks have developmental dysplasia of the hip. Two diagnostic manipulations of the hip joint can test for a dislocatable hip: the Ortolani and the subluxation maneuvers (see Chapter 215). Infants constrained in a breech position in utero tend to keep their hips flexed after birth and resist full hip extension. These infants, particularly girls, also have an increased incidence of dislocatable hips.13
Malformations of the limbs include hemihypertrophy and hemiatrophy; in both conditions, the limbs on each side of the body are noticeably different in size but normally proportioned. With phocomelia, there is underdevelopment and abnormal shape of the limbs to a variable degree. The arms may be flipperlike with small digits projecting from the ends, or there may be only a nubbin of tissue at the site of origin of the limb. This malformation was particularly common among infants whose mothers took the drug thalidomide during pregnancy, but it also occurs spontaneously. The short limbs with achondroplastic and thanatophoric dysplasia are evident at birth (see Chapter 179). Newborns with arthrogryposis multiplex congenita have severe contractions of multiple joints that cannot be corrected by simple manual pressure.
The most obvious anomalies of the hands and feet are fusions of digits (syndactyly) and extra digits (polydactyly). The latter may be well-formed digits or merely small tags of tissue. Some minor malformations of hands and feet occur in many of the dysmorphic syndromes. For example, widely spaced first and second toes, hands with simian creases, downward displaced origin of the thumbs, and incurved little fingers are found in trisomy 21 (Down syndrome). A clenched hand with overriding index finger and a convex or rocker-bottom foot are seen in trisomy 18. Bands originating from the amnion may wrap tightly about a limb and cause a sharp, deep, circumferential depression. These intrauterine constriction bands may amputate the digits or cause localized edema by obstructing lymphatic drainage (see eFig. 44.3  ).
).
NEUROLOGIC EXAMINATION
Interpretation of neurologic signs in a newborn infant requires knowledge of normal development because maturational changes parallel increase in level and complexity of neurologic function. Examination of a baby differs from that of the older child, but it is useful to retain the same basic approach in evaluating neurologic function, including a systematic assessment of mental status (level of alertness), cranial nerve function, the motor and sensory systems, and the evoked reflexes.
 MENTAL STATUS
MENTAL STATUS
Mental status examination consists of observing spontaneous eye opening and movements of the eyes, face, and extremities as well as response to stimulation. A preterm infant born before 32 weeks of gestation spends much of the time sleeping but can be aroused by gentle stimulation. Arousal consists of transient eye opening and movement of the face and extremities. After 32 weeks of gestation, there are periods of spontaneous eye opening with roving eye movements and movements of the face and extremities. More mature babies show an increase in the frequency, duration, and quality of alertness, so that by term there are periods in which the infant may attend to auditory and visual stimuli. The state of quiet alertness (state 3 of Prechtl, Table 44-1) is ideal for eliciting optimal responses. Subtle abnormalities are marked by irritability or lethargy. The irritable and agitated infant cries spontaneously with minimal stimulation and cannot be calmed. Delayed or poorly maintained response to stimulation suggests lethargy. In coma, arousal is impossible. The depth of coma is identified by the level of reflex response to stimulation.
 CRANIAL NERVE EXAMINATION
CRANIAL NERVE EXAMINATION
At 28 weeks of gestation, a baby will blink when a bright light is shone in the eyes (cranial nerves II and VII). The pupillary reaction to light appears between 28 and 32 weeks of gestation (cranial nerves II and III). From 34 weeks of gestation onward, the demonstration of “fix and track” abilities is an essential part of routine examination (cranial nerves II-IV and VI). The “bull’s eye,” a round piece of cardboard printed with glossy black and white concentric circles, makes visual pursuit testing easy to perform (Fig. 44-3). Extraocular movements (cranial nerves III, IV, and VI) can be assessed by observing spontaneous or reflex eye movements.
Table 44-1. Prechtl States of Sleep and Wakefulness in the Newborn



