Evaluation of Vital Signs
Eron Y. Friedlaender
Fred M. Henretig
Introduction
Accurate vital sign measurement is essential for appropriate triage, initial evaluation, and ongoing assessment and management of all patients presenting for care in an emergency department (ED). The systematic evaluation of respiratory and heart rates, blood pressure, body temperature, and peripheral capillary refill enables the rapid determination of specific organ dysfunction and allows for the estimation of severity of illness. Trends in vital sign measurements also help to reflect responses to medical intervention. Certain clinical situations may require continuous monitoring of vital signs rather than intermittent recordings; the use of electronic devices for this purpose is discussed in Chapter 5, which also contains a detailed discussion of the physiology and procedural aspects of blood pressure and tympanic thermometry monitoring. Importantly, under any circumstance, the measurement and interpretation of vital signs in children requires skills, equipment, and techniques suited to the size and age-specific needs of this population, just as the practice of pediatric emergency medicine involves specialized care tailored to the physiologic and developmental needs of young patients.
Anatomy and Pathophysiology
The consideration of several patient factors is important for the accurate measurement and interpretation of pediatric vital signs. More often with children than adults the patient’s emotional state (anxiety, anger, pain), age, and weight and the methods used in obtaining measurements may influence the findings. In addition, significant variations exist in the normal ranges for blood pressure and respiratory and heart rates; failure to account for patient age in the interpretation of vital signs may cause undue alarm or false reassurance of stability.
Indication
Vital sign determination offers a fast, objective evaluation of patient disease and physiologic status. Vital sign measurements help the physician estimate the seriousness of current illness and assist in determining the need for various forms of medical intervention. In the apparently well patient, they may also serve as a screening tool, occasionally identifying patients with unsuspected pathologic conditions.
The extensive range of mechanisms and etiologies of emergency medical and traumatic conditions in children requires that providers approach the care of a sick child using a systematic schema for evaluating physical findings and vital signs. One system, currently advocated in the American Heart Association’s Pediatric Advanced Life Support course (1), utilizes the “ABC” mnemonic approach. This system emphasizes the early recognition of problems related to the airway (A), the determination of the adequacy of breathing (B), and the determination of the status of patient circulation (C). This chapter will use a similar approach to the determination and interpretation of pediatric vital signs.
The most serious problem encountered in any medical setting is a patient with cardiac arrest. Unlike in adult patients, cardiac arrest in children is rarely the result of sudden cardiac dysrhythmia or infarction. Rather, cardiac arrest in pediatric patients is more likely the result of a compromised airway or failure of pulmonary ventilation. In addition, children in septic, distributive, or hypovolemic shock states display signs of reduced peripheral perfusion (delayed capillary refill) and persistent tachycardia before they manifest hypotension.
It follows, then, that recognition of the early signs of cardiorespiratory compromise allows for therapeutic intervention and possible prevention of further clinical deterioration.
It follows, then, that recognition of the early signs of cardiorespiratory compromise allows for therapeutic intervention and possible prevention of further clinical deterioration.
Complications
Although vital signs are an important component of the initial ED evaluation, medical staff should not permit the precise measurement of vital signs to delay the establishment of an unobstructed airway or support respirations or circulation for a patient in extremis. The temptation to measure patient vital signs at the expense of necessary emergency interventions can have disastrous consequences. A rapid survey of the ABCs and interventions necessary to correct any problems should always take precedence over detailed measurement of routine vital signs.
Procedures
Vital Impression
Evaluation of a patient begins with a general assessment. This rapid survey or “vital impression” includes an assessment of airway patency, the adequacy of respirations, the quality of cry, and skin color and a general visual assessment of the degree of patient illness. Level of consciousness, eye contact and visual tracking (especially in the young infant), and age-appropriate interaction with caregivers all contribute to this global assessment. This vital impression is helpful as a quick first screen in determining the need for emergency interventions.
Respiration
After establishing the patency of the airway, ensuring the adequacy of ventilation and oxygenation must take priority over all other medical interventions. The evaluation of respirations should include the rate, effectiveness, and pattern of breathing and the work of breathing. A patient’s respiratory rate is the number of breaths taken in 1 minute. The effectiveness of respiration is clinically estimated by determining the adequacy of air movement, the presence or absence of cyanosis, and any changes in mental status.
Equipment and Procedure
The respiratory rate is routinely measured and recorded during the course of most ED evaluations. The respiratory rate should be taken while the patient is relaxed (asleep, if possible, in infants) and breathing at a rate unaffected by the process of evaluation. Attempts to calm or distract anxious or uncooperative patients prior to assessment will result in more accurate measurements. The respiratory rate may be measured directly by auscultation of breath sounds during a given length of time. In the young or uncooperative patient, the respiratory rate may sometimes be determined more accurately by simply counting chest or abdominal movements over a determined period. The accuracy of a counted respiratory rate improves when the period of time for determination is lengthened (1 minute is optimal).
The respiratory rate may also be determined by respiratory inductive plethysmography. By measuring changes in thoracic impedance between two cardiac chest leads, the number of chest wall movements over a set time can be determined. However, one must not rely on electronic measurement of respirations as the sole method in determining the respiratory rate of patients. Electronic measurement of chest wall movements may not accurately correlate with the number of effective respirations. Electronic measurement of respiratory rates may also be erroneously influenced by voluntary or involuntary patient movements, precordial cardiac activity, improper application or standardization of equipment, or equipment failure. In addition, chest wall movement does not ensure the presence of an unobstructed airway or the adequacy of air exchange. ED personnel should not rely solely on electronic monitors for the ongoing observation of severely ill children (see also Chapter 5). Failing to detect the presence of a respiratory emergency because of electronic monitor malfunction may have serious medical and legal ramifications.
Interpretation
The interpretation of respiratory rates among children requires consideration of patient age and emotional status at the time of measurement (Table 4.1). Normal resting respiratory rates vary between pediatric age groups (2). The respiratory rates of patients who are emotionally upset, in pain, or feel threatened by the interventions of medical personnel should be interpreted in the context of these stresses. As well, fever and crying will elevate respiratory rates transiently. Therefore, the ED record should reflect the presence of factors that may affect the measurement of respiratory rates.
An aberrant respiratory rate or pattern may be the result of abnormalities in the patient’s airway, pulmonary ventilation, oxygen exchange, acid-base status, central nervous system (due to metabolic or toxicologic derangement), or emotional status; brain or spinal cord lesions; seizures; or lack of patient cooperation.
TABLE 4.1 *Age-Adjusted Respiratory Rates | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Heart Rate
As with respiratory rates, the measurement and interpretation of the heart rate in pediatric patients requires that clinicians consider patient age, clinical condition, and emotional state. Clinical evaluation of the heart rate may also provide the first indication of cardiac rhythm disturbances.
Equipment and Procedure
The heart rate and regularity of rhythm may be determined by several different methods: palpation of pulses, auscultation of heart sounds, observation or palpation of apical chest wall movement, and electronic ECG monitors. The latter technique is detailed in Chapter 5. Palpation of pulses provides additional information concerning pulse volume and has a time-honored mystique that may confer some significant advantages when dealing with older children, adolescents, and adults (3). If possible, the patient’s heart rate should be determined while the patient is relaxed and unaffected by the process of evaluation, although this is typically difficult in the ED setting. Counting the number of heart beats over a defined period determines the beats per minute; counting the beats for a full 60 seconds helps to ensure accurate results. Measuring the rate for shorter periods of time may increase the chances of erroneous results and misguided clinical interventions.
Interpretation
The interpretation of heart rate and rhythm, like that of respiratory rate, depends on numerous physiologic and pathologic variables. Age-appropriate heart rates are listed in Table 4.2. Assuming an accurate measurement in a resting state, a heart rate significantly elevated for age may reflect numerous conditions, including fever, endocrine dysfunction, hypovolemia, hypoxia, hypoglycemia, acidosis, anemia, decreased cardiac function, tachyarrhythmia, vasodilatation, and increased sympathomimetic activity via any of a variety of exogenous or endogenous causes. Alternatively, bradycardia may reflect increased intracranial pressure, hypothermia, endocrine dysfunction, bradyarrhythmia, excess vagal tone, hypoxia, and poisoning, most commonly with digoxin, beta-blockers, or calcium channel blockers.
Pulse volume may be increased under the following conditions: patent ductus arteriosus, aortic insufficiency, hyperthyroidism, fever, and anemia. Decreased pulse volume may signify shock or aortic stenosis.
TABLE 4.2 *Age-Adjusted heart Rates | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
The approach to the diagnosis of an irregular pulse is beyond the scope of this chapter and has been summarized elsewhere (4). However, a common cause of benign heart rate irregularity in children is sinus arrhythmia. In this physiologic rhythm, the pulse rate increases with inspiration and decreases during expiration. If the relation to respiration is not easily apparent during the physical exam, an electrocardiographic rhythm strip will confirm the diagnosis.
Capillary Refill
The measurement of capillary refill time as an indicator of the adequacy of peripheral perfusion, although not a classic vital sign, is a useful complement to temperature, blood pressure, and heart and respiratory rates in the assessment of an ill child. Changes in capillary refill time may reflect decreased vascular volume or alteration in systemic vascular resistance. The capillary refill time is arguably the earliest measurable clinical indicator of inadequate peripheral circulation (5,6).
Procedure
The determination of capillary refill time is simple, reliable, and quick. The time required for the blanched nailbed to return to the normal color represents capillary refill (Fig. 4.1). It is most accurate in a fingernail depressed with gentle pressure for at least 3 seconds and under warm ambient conditions. When using capillary refill time as a reflection of response to medical therapy, serial determinations measured at the same anatomic location prove most reliable.
Interpretation
Normal capillary refill time for the pediatric patient is usually considered to be less than 2.0 seconds. The upper limit of normal for capillary refill time is slightly higher in adults. Schriger and Baraff reported an upper limit of normal of 2.0 seconds for adult men and 2.9 seconds for adult women (5). Skin temperature also plays a role in determining capillary refill time; capillary refill time may be significantly delayed with cool environmental conditions, including air-conditioning (7).
A delay in capillary refill of greater than 2.0 to 3.0 seconds may reflect inadequacy of peripheral perfusion. Saavedra et al. reported a correlation between the degree of dehydration in pediatric patients and prolongation of capillary refill time (6). In patients admitted to the hospital for diarrhea, a refill time of 1.5 to 3.0 seconds suggested a fluid deficit of greater than 100 mL/kg.
Other conditions that may result in a prolongation of capillary refill time include heart failure, hypothermia, electrolyte abnormalities, hypotension, and conditions resulting in alterations of circulatory regulation.
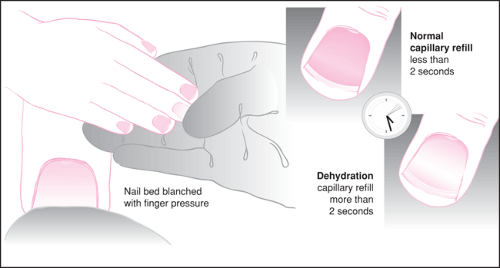 Figure 4.1 The assessment of capillary refill time at the fingernail bed.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|