Evaluation of the Infant and Child with Liver Disease
Robert H. Squires Jr.
Evidence of liver disease in children may take different forms. Physical findings are the most obvious and include jaundice, hepatomegaly (with or without splenomegaly), and ascites. More subtle physical findings in chronic liver disease include prominent abdominal vessels that extend from the upper abdomen to the chest and hemorrhoids seen with portal hypertension, palmar erythema (eFig. 419.1  ), spider nevi (eFig. 419.2
), spider nevi (eFig. 419.2  ) digital clubbing, isolated splenomegaly and excoriations of the skin due to pruritus. An evaluation and management of nutritional deficiencies due to liver disease, pruritus, variceal bleeding and ascites are further discussed in Chapter 425.
) digital clubbing, isolated splenomegaly and excoriations of the skin due to pruritus. An evaluation and management of nutritional deficiencies due to liver disease, pruritus, variceal bleeding and ascites are further discussed in Chapter 425.
Laboratory studies may help confirm the presence of liver injury in the absence of other obvious clinical findings. Thus, “screening” laboratories in patients with non-specific symptoms may reveal elevations in liver-related enzymes, or liver functions in the absence of clinically apparent liver disease, being the only sign of liver injury.
The evaluation of the various presentations of liver disease depends upon the specific abnormalities identified and the severity of illness. Patient age must also be considered because the likelihood of various disorders varies with age. This chapter first reviews the diagnostic tests utilized for evaluation of the infant and child with liver disease, then discusses the approach to diagnosis of infants and children with various presentations of liver disease. The management of chronic liver disease is further discussed in Chapter 425. Details of the diagnostic approach for various liver infections are discussed in Chapters 247 and 308; and for liver tumors in Chapter 427.
BIOCHEMICAL EVIDENCE OF HEPATOCELLULAR OR BILE DUCT INJURY
Although commonly referred to as “liver function tests,” the majority of serum tests measure the enzymes that are produced within the hepatocytes or biliary system but are not measures of physiologic function. The serum levels of these enzymes that include a serum aspartate aminotransferase (AST, SGOT), alanine aminotransferase (ALT, SGPT), gammaglutamyl transpeptidase (GGT), serum alkaline phosphatase (SAP), and a fractionated bilirubin are nonspecific and can be increased in numerous different pathologic processes.1 However, elevation of these tests requires an evaluation for hepatocellular or bile duct injury. As described below, other common laboratory tests are more useful for the evaluation of “liver function,” including measures of serum albumin, ammonia, bile acids, and coagulation studies.
Table 419-1. Conditions Associated with Elevation in Aminotransferase Levels (AST, ALT)
Viral hepatitis |
|
|
|
|
Immune mediated disease |
|
|
|
Metabolic disease |
|
|
|
|
|
Drug or toxic injury (see also Table 422-1) |
|
|
|
|
|
|
Hypoperfusion |
|
|
|
Passive Congestion |
|
|
|
|
Liver trauma |
Nonhepatic causes |
|
|
|
|
AST, aspartate aminotransferase; ALT, alanine aminotransferase.
 SERUM AMINOTRANSFERASE
SERUM AMINOTRANSFERASE
Serum aminotransferase elevation is usually caused by hepatocellular injury owing to inflammation, toxin, or passive congestion. Although a list of specific conditions associated with elevated aminotransferase levels would be unwieldy and ultimately unhelpful, a list of categories of diseases along with common examples is compiled in Table 419-1. The degree of aminotransferase elevation does not correlate with the degree of liver damage and levels are of little prognostic value. The highest aminotransferase elevations are found in drug or viral induced hepatitis, cardiovascular shock, and exposure to hepatotoxins such as an overdose of acetaminophen. On the other hand, a rising serum bilirubin and normal or near normal AST and ALT in the setting of liver failure is an ominous sign reflecting near complete loss of hepatocellular mass. Importantly, injury or inflammation to cardiac or skeletal muscle is also associated with increased AST and ALT levels. When elevated aminotransferase levels are related to muscle injury, the AST is often, but not always, higher than the ALT. Serum CPK and aldolase levels should be obtained prior to any invasive procedure to evaluate isolated elevation of serum aminotransferase levels. Other causes of elevated aminotransferase levels include hemolysis, celiac disease and the presence of a macroenzye of AST. In the later circumstance, the AST will range from 60 to 1100 IU/L with a normal ALT. Low levels of ALT and AST can be caused by B6 (pyridoxine) deficiency because pyridoxal phosphate is a coenzyme for ALT and AST. Uremia may also cause an artificially low AST level.
 γ-GLUTAMYLTRANSPEPTIDASE (GGT) ELEVATION
γ-GLUTAMYLTRANSPEPTIDASE (GGT) ELEVATION
γ-Glutamyltranspeptidase (GGT) elevation is most commonly associated with injury to bile duct epithelial cells. Such injury may result from obstruction or inflammation (Table 419-2). Unfortunately, the GGT is not a component of the standard laboratory “liver profile.” Therefore, the GGT must be ordered separately. The GGT should be obtained on every infant and child with suspected liver disease as it can be the only abnormal test. While elevation of GGT suggests a significant bile duct injury or reduced bile flow, it can be paradoxically normal with certain bile acid enzyme or canalicular transport defects (eg, Progressive familial intrahepatic cholestatis-1, bile salt export pump transporter defects—see Chapter 421.2 Some medications, such as phenobarbital, induce production of GGT leading to increased serum levels. Glutamyltranspeptidase (GGT) is found in other tissues as well, including the kidney, liver, spleen, pancreas, heart, and brain, in such a manner that injury to these tissues may affect the serum value.
Table 419-2. Conditions Associated with Elevation of γ-Glutamyltranspeptidase (GGT)
Bile duct obstruction |
|
|
|
|
|
|
|
|
|
Cholestasis related to hepatocellular injury |
|
|
|
Progressive familial intrahepatic cholestasis 3 |
Biliary inflammation |
|
|
|
Medications |
|
|
 SERUM ALKALINE PHOSPHATASE (SAP)
SERUM ALKALINE PHOSPHATASE (SAP)
Serum alkaline phosphatase (SAP) is used infrequently to assess children with cholestasis as it may be elevated for reasons unrelated to hepatic function such as bone injury or growth. SAP levels rise above the normal levels for adults during adolescence when bones are growing at a rapid rate and may be reported as abnormal by a laboratory that does not utilize age-specific normal values for this test. Benign elevation of serum alkaline phosphatase is an important condition to remember when faced with unexpected, but marked elevation of SAP. A typical clinical setting is that of an infant or toddler with an apparent viral gastroenteritis in whom the SAP is measured. Very high levels of SAP that range from 500 to more than 5000 IU/ml tend to resolve spontaneously although familial elevation of SAP is described. Treatment for this condition is reassurance and avoidance of unneeded, expensive, and invasive tests in search of a suspected liver abnormality. Because zinc is a cofactor for this enzyme, zinc deficiency can result in a low AP level.
LABORATORY TESTS OF LIVER CELL FUNCTION
Although there are no standard clinical tests to assess the actual functional status of the liver, a variety of indirect measures to evaluate various synthetic and detoxification functions of the liver are available in most laboratories. These include measurements of conjugated bilirubin, glucose, ammonia, albumin, prothrombin time/INR, Factor V, Factor VII, and fibrinogen. These are surrogate markers of liver function as conditions other than liver disease may also affect their serum levels.
Bilirubin The unconjugated form of bilirubin is called α-bilirubin, the monoconjugated form is called β, and the diconjugated is termed γ. That fraction of bilirubin glucuronides covalently bound to albumin is called δ-bilirubin. Virtually all serum bilirubin in the normal individual is unconjugated. Elevated bilirubin levels reflect increased production, as in hemolysis, reduced hepatic uptake, as in parenchymal liver disease, decreased conjugation, as in Gilbert disease, or decreased biliary excretion, as in bile duct obstruction. Conjugated hyperbilirubinemia (greater than 2.0 mg/dL conjugated bilirubin, or conjugated bilirubin greater than 15% of the total bilirubin) indicates hepatobiliary disease and always requires investigation. Urobilinogen is formed from the degradation of conjugated bilirubin by bacteria in the intestine. Up to 20% is reabsorbed and undergoes enterohepatic circulation. With hepatic dysfunction, more urobilinogen appears in the urine, giving it an amber hue. In complete biliary obstruction, however, urobilinogen disappears from urine as less bilirubin enters the intestinal lumen.
Hyperbilirubinemia is discussed above but conjugated hyperbilirubinemia is a marker of liver cell or bile duct function.
Bile Acid Levels These are typically measured in serum as cholylglycine, reflect a balance of input (absorption from the intestine) and removal (uptake by the hepatocyte) of bile acids from the enterohepatic circulation. An abnormally high serum level is a sensitive indicator of cholestasis, even in the absence of jaundice. A low level may indicate an inborn error in bile acid metabolism or transport. Serum bile acid levels are usually measured in the fasting state.
Glucose Hypoglycemia is seen more commonly in the setting of liver failure, metabolic conditions such as glycogen storage disease, and disorders of fatty acid metabolism or mitochondrial enzyme defects, yet it is also seen in hyperinsulin states and malnutrition.
Ammonia Ammonia is produced primarily by the action of colonic bacterial urease on dietary proteins. It is cleared through hepatic transformation into urea via the urea cycle. Normal hepatic function allows for the removal of 80% of portal venous ammonia in a single pass. In chronic liver disease there is impaired removal as well as shunting of portal blood to the systemic circulation, allowing ammonia and other toxins to bypass the liver and reach the central nervous system. A rise in serum ammonia may portend the onset of hepatic encephalopathy, although the absolute concentration of ammonia does not correlate with onset or degree of encephalopathy. The sample for measurement of plasma ammonia should be collected from free-flowing blood, either via an arterial source or with venipuncture without a tourniquet. Fasting serum levels more accurately reflect ammonia clearance.
Hyperammonemia occurs in both acute and chronic liver diseases and in the setting of metabolic diseases that may or may not be associated with liver dysfunction such as urea cycle enzyme defects, organic acidemias, and mitochondrial dysfunction. Often, a change in diet, metabolic stress, or gastrointestinal hemorrhage will precipitate an episode of hyperammonemia. Blood for ammonia determination must be obtained properly from a free-flowing venipuncture after the tourniquet is released or an arterial catheter, then the blood sample is placed quickly into ice and taken immediately to the clinical laboratory for prompt analysis; any deviation from this protocol can result in a falsely elevated value.
Albumin and Prealbumin Albumin is synthesized only in the rough endoplasmic reticulum of the hepatocyte, at a rate of 150 mg/kg body weight/d. Its half-life in the serum is approximately 20 days. Prealbumin has a shorter half-life, so that changes in prealbumin levels represent more acute changes in hepatic synthetic function.
Hypoalbuminemia occurs with acute severe hepatocellular injury, chronic advanced disease, or decompensation of a stable liver condition, but can be seen with protein losing enteropathy, proteinuria, and malnutrition.
Coagulation Studies Prolonged prothrombin time (PT) and international normalization ratio (INR) can occur in both acute and chronic liver injury and, when present, suggests serious liver dysfunction. It is a convenient and affordable test that can be performed in virtually all laboratory facilities and should be obtained in all patients with evidence of acute liver injury. Yet abnormalities in coagulation also occur in non-liver-related conditions, typically related to malabsorption of vitamin K, such as pancreatic insufficiency, celiac disease, intestinal bacterial overgrowth. Factor VII levels that are less than 12% of normal may be predictive of irreversible fulminant hepatic failure.
EVALUATION OF HEPATOBILIARY STRUCTRURE
The macroscopic structure of the liver may be evaluated by several modalities. Abdominal radiographs are of limited value for evaluation of the liver, with the only clinically relevant findings being the demonstration of calcified lesions (including some gallstones), air within the portal venous system (as seen with necrotizing enterocolitis), or air in the biliary system (as seen in gallstone ileus).
Ultrasonography This test uses sound waves to demonstrate changes in the echotexture of the liver. This allows for detection of cystic lesions, solid tumors, or infiltration of the hepatocytes with storage material. Biliary system abnormalities such as ductal dilatation are well visualized by ultrasonography. Choledochal cysts and gallstones are detected with an accuracy of 95 to 99%. The use of Doppler flow technology allows visualization of the vasculature associated with the liver (ie, hepatic vein, hepatic artery, portal vein) and its direction of flow.
Computed Tomography (CT) This test enhances the spatial and density resolution of radiographic images. Images can be reconstructed along multiple planes with better ability to interpret data in three dimensions. The sensitivity is further enhanced with the use of intravenous contrast. Calcified lesions are seen with great clarity.
Magnetic Resonance Imaging (MRI) This test identifies tumors and tissue infiltrates comparably with CT, although it poorly visualizes calcium deposits. Magnetic resonance cholangiopancreatography (MRCP) is a result of recent advances in filtering of those signals within the liver that are slow moving (ie, bile) and has allowed for visualization of the bile ducts with clarity compatible to other forms of cholangiography, without the use of intravenous or intraductal contrast. Similar technology (MR angiogram) is available for the visualization of the vascular structures of the liver.
Endoscopic Retrograde Cholangiopancreatography (ERCP) This test uses a specialized side-viewing endoscope for direct injection of contrast medium into the common bile duct through the ampulla of Vater. It provides excellent images of the intra- and extrahepatic biliary tree. This method also allows for endoscopic interventions including stone removal, stenting of ducts, biopsies, and papillotomy. Difficulties involve the technical expertise required in using a special side-viewing endoscope as well as the risk of pancreatitis.
Percutaneous Transhepatic Cholangiography (PTC) This test allows visualization of the biliary tract by placing a needle into the hepatic parenchyma and injecting radiopaque contrast medium into the ductal system. This technique is often difficult in smaller children because of the small caliber of the intrahepatic ducts but can be useful, particularly when ducts cannot be accessed by ERCP, such as occurs after portoenterostomy.
Radionuclide Imaging using cholephilic radiotracers detects diffuse parenchymal abnormalities and hepatobiliary excretory dysfunction. N-Substituted iminodiacetates (IDAs) labeled with technetium-99 are used in the evaluation of infants with cholestatic liver disease based on their ability to demonstrate bile flow. Other studies can look specifically at gallbladder function and calculate the fractional percentage of bile that is ejected from the gallbladder after a fatty meal.
Liver Biopsy This test evaluates microscopic hepatic structure and can be used to diagnose disorders, assess prognosis, determine response to therapeutic interventions, and monitor effects of hepatotoxic drugs. Analysis of the biopsy specimen can include histology, metal content, biochemical or enzyme assay, culture for viral, bacterial, or fungal pathogens, and electron microscopy. Based on the clinical setting this tissue can be obtained by different techniques. Biopsy can usually be performed safely using a percutaneous approach. The biopsy site is typically just anterior to the right midaxillary line at about the 10th intercostal space. Relative contraindications to using this technique include significant coagulopathy, ascites, focal lesions (abscess, cyst, vascular lesions), and infection, infiltrate, or effusion involving the right lung, and elevations in right heart pressures. Risks of the procedure include bleeding, pneumothorax, intestinal perforation, hemobilia, and infection. Mortality is estimated at 0.009 to 0.12%. The use of ultrasound-guided biopsy allows for more specific targeting and thus an ability to sample a specific lesion and avoid vascular structures. Other approaches to liver biopsy include transjugular biopsy, most often used when there is a high risk of bleeding using the percutaneous approach. Laparoscopic or open liver biopsy is useful to obtain a large sample for enzyme analysis, etc. or when other approaches are associated with unacceptable risk.
SYMPTOMS AND SIGNS OF LIVER DISEASE
 JAUNDICE
JAUNDICE
Jaundice refers to the yellowish discoloration of skin, sclera, and mucous membranes due to an excess of bilirubin in the blood. Other body fluids, such as tears, saliva, and cerebrospinal fluid, may also be tinged with yellowish hues. Jaundice is clinically evident in infants with total bilirubin levels of 4 to 5 mg/dl (68–85 μmol/L*); in older children, bilirubin levels above 2 mg/dl (34 μmol/L) can be visually evident. Each elevated total bilirubin level should be fractionated to assess the relative contribution of unconjugated (indirect) bilirubin and conjugated (direct) bilirubin. The combination of yellow discoloration of the skin and clear sclera suggests carotinemia, a condition often seen in children taking a pureed diet containing yellow, carotene-containing vegetables. Carotinemia is not harmful to the child, requires no further investigation other than reassurance to the family, and will resolve as the diet is advanced to more solid foods. [* mg/dl × 17.1 = μmol/L; based upon the molecular weight of bilirubin of 584].
Approach to the Infant with Hyperbilirubinemia
The general approach to the evaluation of infant with unconjugated hyperbilirubinemia is discussed in detail in Chapter 53.3 In the hyper-bilirubinemic infant with jaundice persisting past the first 2 weeks of age further evaluation is important. An elevated conjugated bilirubin level is likely due to hepatocellular injury or obstruction of the biliary tract. A conjugated bilirubin level that is greater than 2 mg/dl or greater than 20% of the total bilirubin should be considered abnormal. Any elevation of the direct bilirubin should be repeated within 3 to 7 days to establish a trend toward either improvement or continued elevation.
If the infant has hepatosplenomegaly or ascites pathologic causes of hyperbilirubinemia are far more likely. Causes of direct hyperbilirubinemia in the infant are listed in Table 419-3.
Table 419-3. Causes of Direct Hyperbilirubinemia in the Infant
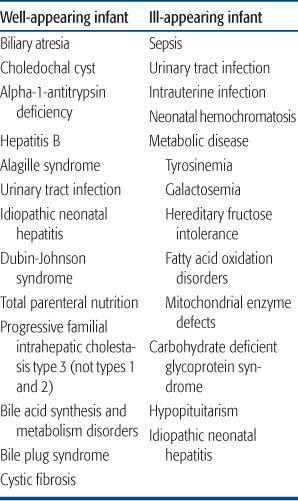
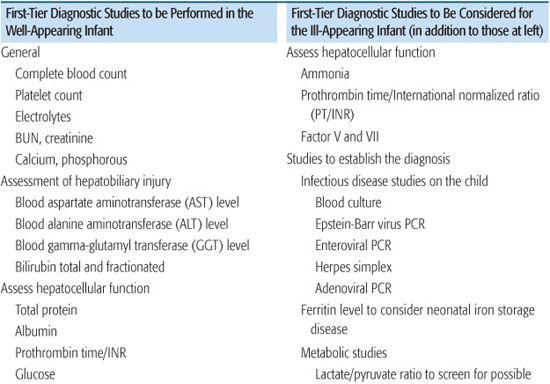
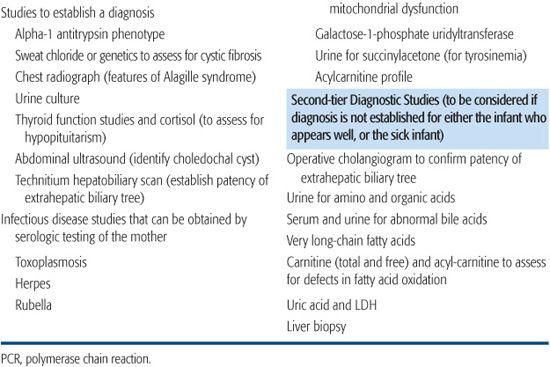
The diagnostic approach to the infant with direct hyperbilirubinemia varies depending upon the history and clinical presentation. The perinatal history is important to identify infants at risk for liver disease. Maternal factors associated with cholestasis in infants include maternal rubella, hepatitis B, HIV, syphilis, genital herpes or liver disease; exposures or complications during pregnancy such as medication or illicit drug use. Polyhydramnios, fever, and a history of consanguinity are also risk factors. Both acute fatty liver of pregnancy and the maternal HELLP (hemolysis, elevated liver tests, and low platelets) syndrome have been shown to be associated with LCHAD (long-chain 3-hydroxyacyl-CoA dehydrogenase) deficiency in the infant. Physical examination will determine whether the infant appears “sick” or “well” and identify whether important features such as a pathologic rash, hepatosplenomegaly, ascites, excessive bleeding or bruising, or an altered level of consciousness are present. The most common causes of conjugated hyperbilirubinemia is sepsis (especially urosepsis with E. coli) and hypoxia/ischemia. In the otherwise well appearing infant it is critical to establish whether the disorder is due to a treatable cause of extrahepatic obstruction. Ultrasound is useful for diagnosis of choledochal cyst (Chapter 427). Diagnosis of extrahepatic biliary atresia is critical since early surgical intervention (before 45 to 60 days of life) improves outcome (Chapter 427). Technitium hepatobiliary scans are used to evaluate bile duct patency in some centers, however, sensitivity and specificity are not optimal, and performing the text can delay diagnosis and therapy. Therefore, in many centers a liver biopsy is performed if other screening evaluations do not identify an etiology. Liver biopsy is useful for diagnosis of biliary atresia (bile duct proliferation, bile plugs and portal fibrosis), metabolic disorders or giant cell hepatitis, or biliary hypoplasia. Other studies are listed in Table 419-4, being prioritized depending upon whether the infant appears sick or well. Beyond infancy, jaundice is much more likely to signal significant liver problems such as congenital abnormalities of the biliary tract, infections, and inborn errors of metabolism.
Table 419-4. Laboratory Tests to Evaluate the Infant with Direct Hyperbilirubinemia
Approach to the Child with Jaundice
An isolated elevation of bilirubin without alterations in other liver enzymes should be considered separately from those disorders with jaundice with abnormalities of other liver enzymes. In isolated hyperbilirubinemia, if the direct component is less than 15% an evaluation for hemolysis should be performed (see Chapter 433). If there is no hemolysis the diagnosis of Gilbert syndrome is likely (see Chapter 421). If the direct bilirubin accounts for greater than 15% of the total bilirubin, a diagnosis of Dubin-Johnson or Rotor’s syndrome should be considered. After the first year of life, jaundice associated with other hepatic enzyme elevations is likely to have an infectious, autoimmune, or systemic disease affecting the liver. Table 419-5 lists those disorders associated with direct hyperbilirubinemia. Tables 419-1 and 419-2 list disorders commonly associated with biochemical evidence liver disease. In the patient with jaundice and elevated direct bilirubin it is essential to assess the severity of the illness. If there is no antecedent evidence of chronic liver disease, and jaundice is of rapid onset, urgent evaluation for possible fulminant hepatitis includes the performance of liver functional tests such as the prothrombin time, INR, glucose and ammonia levels (see Chapter 424). Similarly, in a patient with liver disease and a rapid increase in the level of jaundice, assessment of hepatic function should be assessed. The evaluation based upon the severity of illness is outlined in Table 419-6. Liver infections are discussed in more detail in Chapter 237 (see Tables 237-1 and 237-2).
Table 419-5. Conditions Associated with Direct Hyperbilirubinemia in the Older Child



