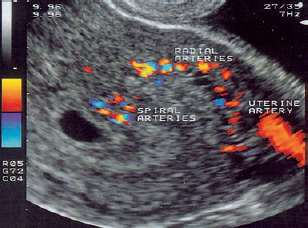
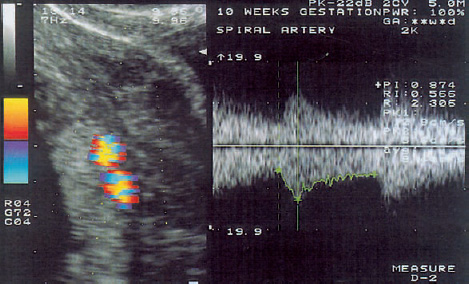
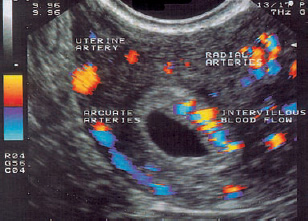
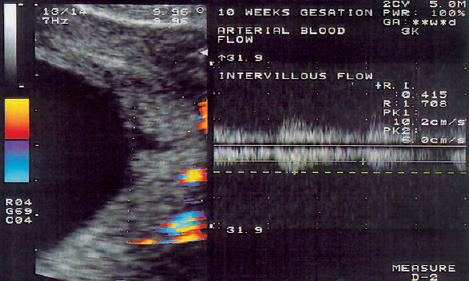
11 Evaluation of Early Placentation and the Embryonic Circulation with Doppler Ultrasound There is a brief period after ovulation in which the endometrium is most receptive to implantation. During this time, a blastocyst entering the uterine cavity can establish contact with the endothelial surface and become implanted41. The optimum time for implantation is between the fifth and seventh day after ovulation. Thus, implantation of the blastocyst occurs on about day 21 of the cycle and is complete by day 26, when the endometrial membrane completely envelops the blastocyst. When implantation commences, the inner cells of the blastocyst face the endometrium41. The action of proteolytic enzymes produced by the syncytiotrophoblast causes erosion and invasion of the uterine mucosa. As implantation continues, the trophoblast erodes adjacent maternal capillaries, allowing maternal blood to come into direct contact with the embryo. Finally this lacunar system gives rise to the intervillous space of the placenta. Transformation of the spiral arteries. During the 4th week of gestation, the trophoblast invades the uterine wall and gradually penetrates into larger venous sinusoids and superficial arterioles. The extravillous cytotrophoblastic cells penetrate to the lumina of the spiral arteries. They transform the thick-walled arteries surrounded by smooth-muscle cells into flaccid, saclike uteroplacental vessels, which can accommodate the surge of maternal blood flow through passive dilation. The increased blood flow is necessary to supply the fetus with oxygen and support its growth3 (Fig. 11.1). Cells of the trophoblast can be found in the spiral arteries starting at about five weeks after fertilization (Fig. 11.2). The destructive action of the trophoblast on the muscle cells and elastic fibers of the spiral arteries has two effects: 1. The increasing blood flow causes a progressive expansion of the vessels. They are transformed into uteroplacental arteries that can accommodate the burgeoning blood supply. 2. The uteroplacental arteries are not subject to control by the autonomic nervous system17. Connection of the spiral arteries to the intervillous space. During the second month of gestation, the intervillous space becomes markedly larger owing to arborization of the villi. At this time, nests of cytotrophoblastic cells are found in the tips of many spiral arteries near the intervillous space. Meanwhile, numerous anastomoses form among the veins of the decidua. After 40 days (crown–rump length [CRL] = 15 mm), the spiral arteries communicate through direct openings with the intervillous space, and cytotrophoblastic cells begin to line the arterial lumina. Maternal blood reaches the intervillous space through gaps between the cells of the endovascular trophoblasts. The fact that the cytotrophoblastic cell columns are not flushed from the lumen of the spiral arteries suggests that the blood pressure is not high. Fig. 11.1 Transvaginal ultrasound scan of an early gestational sac. Note the eccentric position of the sac, its location in the fundus, its elliptical shape, and its double contours. Color Doppler provides an excellent view of the uterine vessels. Fig. 11.2 Transvaginal scan of an early gestational sac. The color-encoded area represents the spiral arteries (left). The Doppler spectrum (right) indicates a high flow velocity and low impedance. Definitive placenta. By the end of the fourth month of gestation, the definitive placenta has developed from the chorion frondosum. The peripheral villous trees of the chorion, which are connected to the decidua capsularis, degenerate and the associated intervillous space disappears. The smooth, avascular chorion laeve17 is formed by fusion of the chorionic plate and basal plate. Trophoblastic infiltration of the myometrium occurs between the 8th and 18th weeks of gestation. The endovascular cytotrophoblast partially replaces the endothelium of the myometrial vessels and invades the smooth-muscle cells of these vessels. This results in increasing expansion of the radial arteries located in the myometrium. Uteroplacental circulation. The uteroplacental circulation is a low-pressure system because the diameters of the vessels steadily increase on their way to the intervillous space. To keep the normal arterial pressure from being transmitted to the intervillous space, a considerable pressure drop occurs between the proximal, nondilated portion of the uteroplacental arterioles and the distal, dilated portion. Opening of the spiral arteries in the 12th week of gestation. The classic theory on the origin of the uteroplacental circulation described above4,43 was challenged for a time by the results of Hustin and Shaaps6,7. Their in-vivo studies of the placenta using transvaginal sonography, intervillous hysteroscopy, and phase-contrast examination of chorion villus sampling material showed that there is no true continuous blood flow in the intervillous space during the first 12 weeks of pregnancy. The authors studied tomograms of hysterectomy specimens from an in-situ pregnancy that were taken in the 7th, 8th and 9th weeks of pregnancy and found no contrast medium in the intervillous space. When this study was done in the 13th week of pregnancy, the placenta filled rapidly with contrast medium. Histological examinations of these hysterectomy specimens showed occlusion of the uteroplacental arteries by trophoblastic cells until the 12th week of gestation. Serial sections of spiral arteries also indicated an absence of intervillous blood flow before the 12th week. On the other hand, no trophoblastic plugs were found in the uteroplacental arteries in the 13th week, and contrast medium was found surrounding the villi in the intervillous space. These results suggested that mainly fluid from the maternal plasma and uterine glandular secretions enter the early placenta on the maternal side. The authors assumed that intervillous blood circulation was absent or rudimentary during the first 12 weeks of gestation. According to this theory, the expansile changes in the spiral arteries take place throughout the first trimester. Finally, by about the 12th week of gestation, all of the trophoblastic cell columns in the spiral arteries are loosely arranged and displaced. This process gives the maternal blood free access to the intervillous space, clearing the way for a fully developed placental blood flow. PO2 values in the placenta. This theory was supported by a more recent study45 using a polarographic oxygen electrode that was introduced under ultrasound guidance. This study showed that the Po2 values in the placenta were significantly lower than in the endometrium between the 8th and 10th week of gestation, while these values were similar between the 12th and 13th week. The intraplacental PO2 values rose significantly between the 8th–10th and 12th–13th weeks. These findings suggest that the rise of the placental PO2 is related to the development of continuous maternal blood flow in the intervillous space at the end of the first trimester. The introduction and evolution of transvaginal color Doppler sonography has made all portions of the embryonic/fetal and uteroplacental circulation accessible to hemodynamic evaluation in vivo22,23,27,28,30–33. Researchers have been able to focus their attention directly on the developing embryo, greatly expanding our knowledge and understanding of the embryonic circulation. Current knowledge on the anatomy and physiology of the uteroplacental blood supply is based largely on the classic early studies on this subject. We shall therefore review chronologically the theories on the origin of the intervillous circulation that have been derived from Doppler ultrasound studies. Intraplacental flow. In 1991 and 1992, Jauniaux et al.10,12 and Jaffe and Warsof9 were unable to detect “intraplacental” flow before the 12th week of gestation with transvaginal color Doppler ultrasound. They did detect intraplacental flow by the 14th week of gestation, accompanied by the appearance of pandiastolic flow in the umbilical artery and a sudden rise of peak systolic flow velocity in the uterine artery. Building on the theories of Hustin and Shapps6,7, they postulated that the simultaneous occurrence of these three phenomena could be explained by the disappearance of the trophoblastic plugs from the spiral arteries. However, Kurjak et al.26 detected no abrupt change in the uteroplacental circulation between the 12th and 14th week of gestation. When a new generation of much more sensitive color Doppler scanners became available, several authors reported on the existence of intervillous blood flow during the first trimester of pregnancy (Fig. 11.3). Pulsatile and continuous flow. In 1995, Kurjak et al.25 published the first study on the combined assessment of intervillous blood flow using Doppler ultrasound and pathomorphological analysis. Two types of intervillous flow were detected in all patients scanned with an endovaginal color Doppler probe: pulsatile, artery-like flow (Fig. 11.4) and continuous, veinlike flow (Fig. 11.5). In a parallel histological study, there was no time at which the spiral artery lumina were completely occluded by trophoblastic cells. These results suggest that the development of the intervillous circulation is more a continuous process than an abrupt event at the end of the first trimester. Fig. 11.3 Color Doppler permits the simultaneous visualization of uterine, embryonic, and intervillous blood flow. Passage of red blood cells. Subsequently, several other groups of authors published similar results. Valentin et al.46 did a study on uteroplacental and luteal flow combined with a pathomorphological analysis. Color Doppler measurements indicated the presence of intervillous blood flow starting as early as week 6 of a normal pregnancy. They also detected and measured the two types of Doppler signals (pulsatile and continuous flow) in more than 90% of 66 pregnancies from the 5th to the 11th gestational weeks. The authors claimed that the high blood flow velocities observed in subchorionic arteries were at odds with the concept that these arteries are completely occluded by trophoblastic plugs. On pathomorphological analysis, it was found that trophoblastic cells did not completely occlude the spiral arteries but allowed red blood cells to pass through. This led the authors to conclude that intervillous flow was present as early as the first trimester. Fig. 11.4 Pulsatile, artery-like blood flow pattern in the intervillous space (left) is characterized by a low vascular resistance (RI = 0.42). Merce et al.36 published similar results based on a study of 108 normal singleton pregnancies from the 4th to the15th gestational weeks. They were able to detect intervillous blood flow as early as the 5th week (+ 6 days). This flow produced a slightly undulating, veinlike signal that tended toward higher velocities over the course of the first trimester. They also documented arterial signals in the retrochorionic segments of the uteroplacental vessels. They concluded that their results were consistent with the classic embryological concept that intervillous flow develops between the 4th and 7th weeks of gestation. According to Merce et al.36, the uteroplacental circulation undergoes pronounced changes starting in the 4th week of pregnancy. Intervillous blood circulation and initial umbilical blood flow were detected from the 5th week onward. Comparison with nonhuman primates. Experiments in primates, especially monkeys, have been a crucial part of research on the development of the placenta and the uteroplacental circulation. The classic study by Elisabeth Ramsey on blood circulation in the intervillous space of the primate placenta is the basis for all present-day research in this area43,44. Nimrod et al.38,39 more recently reported on the assessment of early uteroplacental blood flow in the cynomolgus monkey (Macaca fascicularis
Implantation
Development of the Intervillous Circulation
Classic Theory
Objections and Alternative Theories
Color Doppler Studies
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree