6 Color Doppler Sonography for the Optimization of Assisted Reproduction The inability to conceive is a problem that affects some 10–15% of all couples. The causes of infertility are multifactorial in many cases. In addition to primary ovarian, hypothalamic-pituitary, extragenital endocrine, psychogenic, immunological, genetic, tubal, uterine, cervical, and vaginal causes of infertility, there are growing numbers of cases that result from a male infertility factor or have an unexplained cause (“idiopathic infertility”). In 30% of cases, the causes of infertility relate to both partners22. For all therapeutic approaches that are applied in assisted reproduction (Table 6.1), it must be considered that the functional status of the endometrium is a major determinant of successful implantation. The outcome of any procedure in reproductive medicine depends critically upon whether the embryo encounters an endometrium that is receptive to implantation. Theoretical considerations led Paulson et al.34 to conclude that a lack of endometrial receptivity in hormone-induced cycles is responsible for two-thirds of all treatment failures. Histological studies. Histological studies have shown that different stimulation protocols lead to different distributions of endometrial abnormalities, with clomiphene showing a particularly high association with significant endometrial dysfunction ranging to complete atrophy8,42,51. Based on these findings, Dallenbach et al.8 state that endometrial biopsy histology should be an essential study in the investigation and treatment of infertility. The disadvantage of histological examination is its invasiveness. Sonomorphological studies. The value of sonomorphological studies of the endometrium in monitoring the cycles of infertile patients is discussed controversial. While it is true that modern high-frequency endovaginal probes can accurately define the sonoanatomy of the endometrium7, research to date has been unable to establish whether ultrasound can supply a clinically useful prognosis with regard to endometrial receptivity21,44. Our own studies indicate that histological findings are not consistently reflected in either the thickness or echo pattern of the endometrium.
Functional Evaluation of the Endometrium
| Method | Abbreviation |
|---|---|
| Intrauterine insemination | IUI |
| In-vitro fertilization and embryo transfer | IVF-ET |
| Gamete intrafallopian transfer | GIFT |
| Pronucleus stage transfer | PROST |
| Zygote intrafallopian transfer | ZIFT |
| Intratubal embryo transfer | TET |
| Intracytoplasmic sperm injection | ICSI |
| Partial zona dissection | PZD |
| Subzonal insemination | SUZI |
Pulsed Doppler ultrasound. Hemodynamic measurements of uterine and ovarian blood flow with Doppler ultrasound represent a new approach in the diagnosis of infertility. These measurements are based upon studies by Taylor et al.45. These authors recorded waveforms from the uterine and ovarian arteries by transabdominal pulsed Doppler scanning and distinguished them from other blood vessels in the lesser pelvis by their location and distinctive flow patterns.
Another advance was the development of Doppler-capable endovaginal transducers. Feichtinger et al.12 were able to obtain nonsuperimposed scans of the uterine and ovarian blood vessels by the transvaginal route and investigated uterine and ovarian blood flow under physiological and pathological conditions.
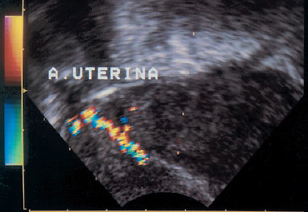
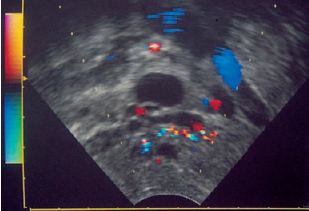
Color Doppler sonography. The use of color Doppler sonography can provide an anatomically precise view of the vascular supply in the lesser pelvis3,13. Uterine and ovarian blood vessels can be rapidly identified and evaluated with this technique (Figs. 6.1 and 6.2).
Goswamy et al.16 presumed that a relationship existed between hemodynamic parameters and implantation rates on the basis of their Doppler investigations of uterine blood flow. Shortly thereafter, we were able to confirm this observation in our own patients18,43. We later studied a larger population to determine whether Doppler measurements of uterine blood flow could be useful in predicting the outcome of implantation17.
Fig. 6.1 Color Doppler image of the ascending main branch of the uterine artery. Parasagittal scan at the level of the uterine cervix.
Fig. 6.2 Color Doppler image of ovarian blood flow in a spontaneous cycle.
Authors’ Studies
Patients and Methods
Patients. Our study population consisted of 124 patients with a tubal or male infertility factor who were undergoing in-vitro fertilization (IVF) after a standard hormone stimulation protocol with human menopausal gonadotropin (hMG) and human chorionic gonadotropin (hCG)42. Sonographic and Doppler sonographic examinations were performed in a total of 68 spontaneous cycles and 161 treated cycles.
Methods of assisted reproduction and controls. Ultrasound-guided transvaginal follicular aspiration was performed in 105 patients. The harvested oocytes were inseminated with washed spermatozoa from the male partner within 12 hours after collection. Embryo transfer was performed at the 4-cell or 8-cell stage.
Nineteen patients underwent pelviscopic follicular aspiration with subsequent gamete intrafallopian transfer (GIFT).
In both the IVF-ET and GIFT groups, the endometrium was endosonographically evaluated and uterine blood flow was measured just prior to follicular aspiration.
Sonographic and Doppler sonographic examinations were performed in 36 patients during the proliferative phase of a spontaneous cycle, at midcycle, in the secretory phase of the cycle, and between days 8 and 10 of the next hormone-stimulated cycle.
Comparison group. Consistent with the definition of our study population, no biopsies were performed in the stimulated cycles. For comparison, we formed a group of 53 women with normal cycles in whom oocyte fertilization did not occur after hormonal stimulation with gonadotropins during the study period. These patients underwent an endometrial biopsy on the day of the planned embryo transfer.
Results. Pregnancy was confirmed sonographically in 34 of 124 patients (27%) following successful fertilization of the oocytes and embryo transfer (n= 105) or GIFT (n = 19) (29 singleton pregnancies, 3 twin pregnancies, and 2 triplet pregnancies). A total of six abortions and one tubal pregnancy were recorded. Twenty-seven pregnancies culminated in a live birth (22%).
Examination Procedures
Endometrial Sonography
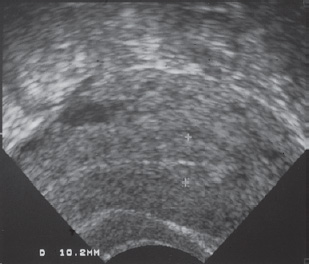
Ultrasound examinations of the endometrium were performed with a 5 MHz endovaginal probe. The uterus was scanned in sagittal section, depending on the position of the anterior fornix (anteflexed uterus) or posterior fornix (retroflexed uterus).
Endometrial thickness was determined as twice the thickness of the endometrial layer, disregarding the periendometrial vascular zone7 (Fig. 6.3).
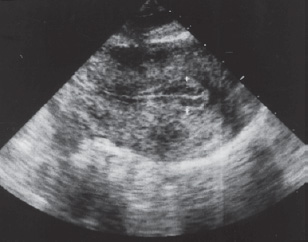
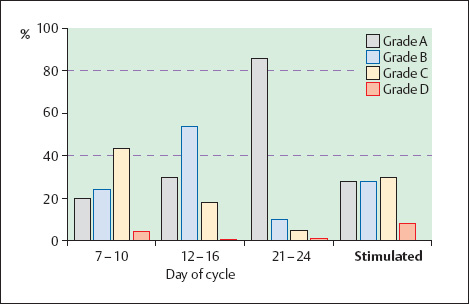
The endometrium was also classified by its echo pattern using the grading system proposed by Smith et al.38 (Figs.6.4–6.7).
The endosonographic findings were related to the phase of the cycle (spontaneous cycles), the result of the histological examination, and the clinical course (implantation rate).
Histology
A uterine fundus biopsy was performed in 70 patients during the secretory phase of the spontaneous cycle (n = 17) or stimulated cycle (n = 53). The biopsy material was immediately fixed in formalin and embedded in paraffin. Sections were prepared and stained with hematoxylin–eosin or van Gieson stain, and the specimens were evaluated according to the criteria of Noyes et al.28 All histological examinations were performed at the Prof. Dallenbach Institute in Mannheim.
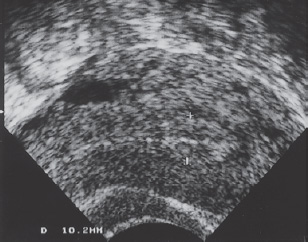
Fig. 6.3 Transvaginal scan of the anteflexed uterus from the anterior fornix. The boundaries of the endometrium are marked with cursors.
Fig. 6.4 The endometrium is echo-free except for a prominent central echo (grade D pattern of Smith et al. 198438).
Fig. 6.5 Increasing echogenicity of the endometrium. The endometrium is always less echogenic than the surrounding myometrium, however (grade C pattern of Smith et al. 198438).
Fig. 6.6 Endometrial echogenicity is comparable to that of the myometrium. A hypoechoic zone (periendometrial vascular zone) can be identified between the myometrium and endometrium (grade B pattern of Smith et al. 198438).
Fig. 6.7 The endometrium is more echogenic than the myometrium (grade A pattern of Smith et al. 198438).
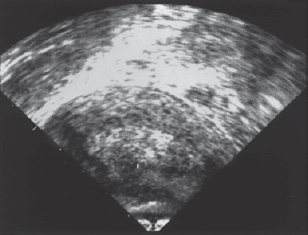
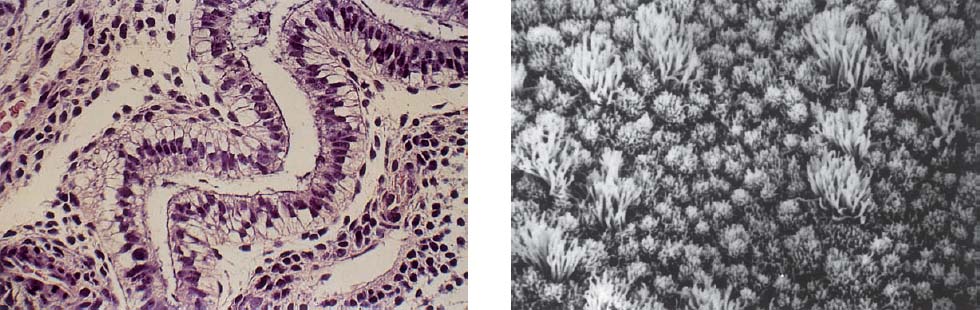
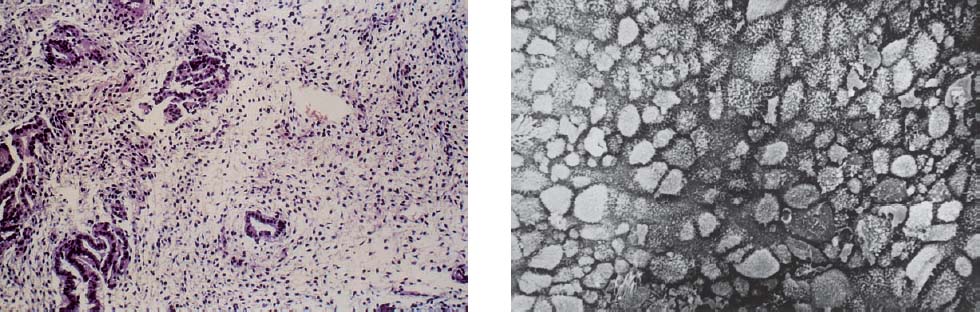
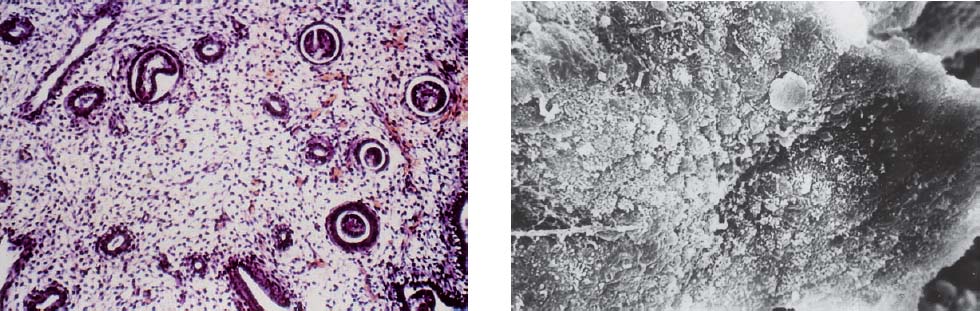
Scanning electron microscopic examinations were additionally performed in a subgroup of patients (Figs. 6.8–6.10).
Doppler Sonography
Equipment. The Doppler studies of uterine blood flow were performed with an endovaginal probe using duplex technique. The probe was a mechanical 5 MHz transducer (B-mode) combined with an integrated 4.5 MHz Doppler transducer (Combison 320–5 with 300 Doppler module, Kretztechnik, Zipf, Austria). The color Doppler scanner was equipped with a 5 MHz endovaginal probe (Toshiba 270 A, Neuss, Germany).
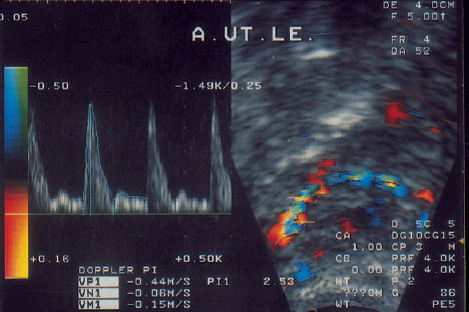
Parameters. The probe was positioned in the vaginal fornix, and the uterine artery was scanned in parasagittal section at the level of the cervix. The Doppler beam was then directed toward the uterine vascular bundle at an angle that produced a maximum frequency shift. The waveforms were subjected to semiquantitative analysis using the resistance index35 and pulsatility index14. These values reflect the degree of vascularity and functional state of the distal arteriolar and capillary bed. High indices signify a low degree of vascularity with a correspondingly high vascular resistance, while low indices reflect a low vascular resistance and high degree of vascularity in the distal bed.
Semiquantitative measurements. Semiquantitative measurements were performed on the day of follicular aspiration in all 124 patients and in the previous spontaneous cycle of 39 patients. Twenty-three other patients were examined in the spontaneous cycle but not in the subsequent, stimulated cycle. Thus the semiquantitative parameters determined for spontaneous cycles are based on a population of 62 patients.
Quantitative measurements. Quantitative measurements are possible only if the angle of the Doppler beam is known. This requires a precise longitudinal image of the vessel to be examined. Color Doppler can provide an extended view of the ascending main branch of the uterine artery (Fig. 6.11). A total of 272 quantitative measurements of systolic and mean uterine blood flow velocities were performed in 32 untreated cycles and in 33 hormone-stimulated cycles.
Fig. 6.8 Normal histological endometrial structure in the secretory phase of the cycle.
a Light micrograph (×240).
b Scanning electron micrograph (×1250).
Fig. 6.9 Deficient secretion.
a Light micrograph (×100).
b Scanning electron micrograph (×1250).
Fig. 6.10 Abortive secretion.
a Light micrograph (×100).
b Scanning electron micrograph (×1250).
Fig. 6.11 Color Doppler image of the uterine artery in parasagittal section. The sample volume has been placed over the vessel lumen at an insonation angle of 52°. At left the Doppler spectrum is recorded from that area.
Evaluation. Both the semiquantitative and quantitative measurements were performed bilaterally. For statistical analysis, the mean value of the measurements taken on the right and left sides was used for each parameter.
The hemodynamic parameters were correlated with the sonomorphological, hormonal, histological, and clinical parameters (implantation rate). The dependence of hemodynamic parameters on the phase of the cycle and on hormonal stimulation was also evaluated.
Results
Endometrial Sonography
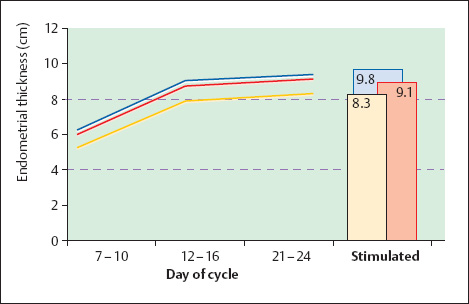
Endometrial thickness. Figure 6.12 shows the sonographically determined endometrial thickness in spontaneous cycles and after hormonal stimulation (mean values ± standard deviation). Analysis of variance indicates a highly significant increase of endometrial thickness over the course of the cycle (p < 0.001). Intergroup testing (t-test) shows a highly significant difference in endometrial thickness between the midproliferative phase and midcycle (p < 0.001). The values measured at midcycle and in the mid-secretory phase do not differ significantly (p = 0.2). The endometrial thickness in these phases corresponds to the values measured in the stimulated cycles (p = 0.5).
Echo pattern. A characteristic change of echo pattern was observed in the spontaneous cycles (Fig. 6.13). While a grade C pattern38 was noted most frequently during the proliferative phase, grades A and B were more prevalent at midcycle. The echo pattern in the secretory phase was almost exclusively grade A. The echo pattern in the stimulated cycles most closely resembled the pattern observed in the proliferative phase.
Implantation rate. Neither the endometrial thickness nor the echo pattern showed a definite correlation with implantation rate. No significant difference was found in endometrial thickness following successful or unsuccessful implantation (9.5 mm versus 9.1 mm; p = 0.71). Figure 6.14 shows the distribution of echo patterns by successful or failed implantation. Clinical pregnancies occurred in association with all four endometrial grades as defined by Smith et al.38.
Fig. 6.12 Endometrial thickness measured endosonographically in spontaneous cycles and after hormonal stimulation. Mean values ± standard deviation.
Fig. 6.13 Endometrial echo patterns (grades A–D after Smith et al. 198438) in spontaneous cycles and after hormonal stimulation.
Histology
Sonographic findings and histological diagnosis. Most endometria in the secretory phase were assigned to grade A as defined by Smith et al.38
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree