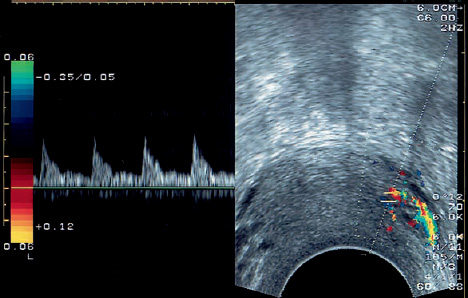
13 Physiology of Doppler Flow in Maternal Vessels during Pregnancy The introduction of Doppler flow measurements has enhanced our ability to investigate the conditions of intrauterine fetal life. For more than 20 years, fetal Doppler ultrasound has provided a simple, noninvasive method for measuring blood flow velocities in the fetal vessels23. Doppler measurements of uterine blood flow, or the maternal part of the fetomaternal circulation, were first reported in 19833. Since the advent of transvaginal sonography and the development of color-encoded pulsed Doppler technology, Doppler flow measurements of the uterine artery and arcuate arteries have been substantially improved. The color mapping of blood flow is particularly advantageous for examining the maternal circulation owing to the many small-caliber vessels in the maternal system. Doppler effect. Christian Doppler (born in Salzburg in 1803) described the effect by which sound waves are perceived as having a higher or lower frequency, depending on whether the source of the sound is moving toward or away from the listener. The amount of this frequency shift is directly related to the velocity of the sound source. By applying this effect, it was possible to measure the frequency shift between the ultrasound emitted by a transducer and the echoes returning from red blood cells and thus determine the velocity of blood flow in fetal and maternal vessels. We know from hemodynamics that the blood flow velocity (i.e., the velocity of the moving red cells) in a vessel is directly proportional to the blood pressure and indirectly proportional to the vascular resistance. Continuous-wave transducers. Various types of Doppler transducer are available. Continuous-wave (CW) transducers consist of a transmitter that continuously emits sound and a receiver that continuously receives the frequency-shifted echoes. One disadvantage of CW Doppler is that it does not discriminate echoes according to their depth. In theory, multiple vessels along the path of the beam can lead to superimposed signals and summation effects. Pulsed-wave transducers. Pulsed-wave (PW) transducers emit ultrasound for a fraction of a second and then switch to the receive mode. These instruments can provide depth discrimination by measuring the echo delay time. Only the echoes that return from a specified tissue depth are analyzed for their frequency shift. This selected depth, called the Doppler gate or sample volume, can be positioned precisely within the vessel lumen, allowing signals to be acquired from a uniquely defined anatomical location. Color Doppler. A color Doppler system displays not only the magnitude of the frequency shift but also the direction of blood flow (either toward or away from the transducer) by means of a color-encoding system (red = toward the transducer, blue = away from the transducer). This makes it easier to locate small vessels such as the arcuate arteries. Indices. Several angle-independent indices can be used to analyze the frequency-shift data: the S/D ratio of Stuart (S = maximum frequency shift in systole, D = minimum frequency shift in diastole), the resistance index of Pourcelot (RI = (S–D)/S), and the pulsatility index (PI = (S–D)/mean value). Uteroplacental blood supply. The uterus derives most of its blood supply from the two uterine arteries, which arise from the iliac artery. A small amount of blood is also supplied by anastomoses with the ovarian vessels, which branch directly from the abdominal aorta. The two uterine artery trunks divide within the myometrium into 10–15 arcade vessels on both sides. These vessels encircle the uterus and form anastomoses near the anterior and posterior midline. The radial arteries arise from these arcade vessels and pass more deeply into the uterus. The radial arteries in turn give rise to the basal arteries, which supply the basal endometrium and the spiral arteries with blood. The tortuous, helixlike spiral arteries supply blood to the placenta; this blood enters the intervillous space from the decidua basalis through broad openings in the spiral arteries. Spiral arteries. At one time it was believed that the ends of the spiral arteries bore constrictions that produced a “jet effect.” If this were true, a high resistance would be present in the spiral arteries. In fact, invading trophoblasts destroy the muscular portion of the spiral artery wall within the decidua by the 20th week of gestation, causing the lumen to expand in the direction of the placenta and creating a pressure difference of only 8 mmHg between the spiral artery and the amniotic cavity25. Uterine enlargement. Normally the uterus increases greatly in size during the course of pregnancy. The weight of a gravid uterus at term is 20 times the uterine weight outside of pregnancy (1000 g versus 50 g). The weight increase is not due mainly to an increased number of muscle fibers but to muscular hyperplasia, i.e., a marked enlargement of the muscle fibers of the myometrium. The blood supply during pregnancy adapts accordingly. Arterial dilatation. The uterine arteries dilate to approximately 3 times their original caliber, the arcuate arteries to 10 times, and the spiral arteries to 30 times15. By the end of pregnancy, blood is flowing through the intervillous space at a rate of approximately 60 ml/min28. The systemic blood pressure prevails to the level of the arcuate arteries. Beyond that, the pressure dwindles to the spiral artery openings, resulting in a low pressure gradient relative to the intervillous space (perfusion pressure 15–20 mmHg). It is apparent, then, that Doppler ultrasound scans of the uterine vessels are representative only to the level of the arcuate arterial bed. Placental blood supply. Because of the numerous anastomoses between the two uterine arteries, both vessels supply the placenta. The uterine arteries each supply a different number of cotyledons, depending on the placental location, and this accounts for the normal difference between the two sides that is recorded with Doppler flowmetry. Perfusion in normal and abnormal pregnancies. In a normal pregnancy, the maternal uterine arteries reflect the perfusion of the entire uterofetoplacental circulation. Owing to the tremendous increase in terminal vascular branches, the peripheral flow resistance declines, causing a rise in diastolic flow velocity. This results in part from progesterone-induced vasodilation and from the development of the intervillous space. In an abnormal pregnancy, vasoconstriction may occur in the uterine circulation (hypertension, preeclampsia) producing a high S/D ratio, or there may be an inadequate development of collateral channels causing an abnormal discrepancy between the sides. Normally a postsystolic notch in the Doppler waveform does not persist beyond the 24th week of gestation. If it persists after 24 weeks, the possibility of an impending pregnancy complication should be considered. The following values are normal for the third trimester: Patient position. In all vaginal ultrasound examinations, it is advantageous to place the patient in a lithotomy position as this allows greater mobility of the endovaginal probe. This position does not compromise uterine blood flow, eliminating the possibility of false-positive findings34. Transducer placement. Contact gel is applied to the ultrasound probe, which is then covered with a condom-like sterile rubber sheath. A lubricating gel is applied, and the probe is carefully inserted into the vagina. It is oriented to provide a sagittal scan of the lesser pelvis. A standard routine should be followed for Doppler flowmetry. In all of our examinations the right side of the monitor is caudal in the sagittal scan, and the left side is cranial. The probe is rotated 90° to obtain a coronal or transverse scan, in which case the right side of the monitor corresponds to the patient’s left side, and vice versa7. Adjusting the Doppler beam and sample volume. After making an initial survey of the lesser pelvis and identifying key landmarks (cervix, gestational sac, ovary, pelvic wall), the examiner positions the ultrasound probe in the lateral fornix of the vagina. Rotating the probe 90° makes it easier to locate the uterine artery in the parametrium, which can be examined in coronal section. The echogenic parametrium is surveyed by slowly moving the scanner anteriorly from the sacrum. With some practice, the uterine artery can be consistently identified as an elongated, pulsating vascular echo 2–4 mm in diameter. Besides its typical course, which can be defined over a variable length, the pulsations of the uterine artery are its most important distinguishing feature. The examination is done with a minimum amount of probe pressure. When the vessel has been located in the real-time scan, the Doppler beam and sample volume are adjusted so that the Doppler frequency shift can be received and recorded. It takes from 5 to 10 minutes to examine both uterine arteries and interpret their spectra. The total examination time depends partly on gestational age. In late pregnancy it can be difficult or impossible to position the probe in the lateral fornix owing to the low position of the presenting fetal part. This is not a problem, however, because Doppler velocimetry of the uterine arteries is used mainly for the early detection of pregnancy complications and is rarely performed after 36 weeks. Instruments. We use an end-fire vaginal probe (KretzTechnik, Zipf, Austria) with a 240° field of view. This instrument can cover all of the lesser pelvis, making orientation easier. We use a transducer frequency of 7.5 MHz and a Doppler beam frequency of 4.5 MHz. The optimum pulse repetion frequency (PRF) setting for most examinations is 5.2 kHz with a penetration depth of approximately 7–8 cm and a 125 Hz filter settings. According to the manufacturer, the power output of the scanner is less than 100 mW/cm2. Parameters. In principle, all of the angle-independent parameters mentioned above can be used for waveform analysis. However, because the maternal vessels exhibit diastolic flow even when the peripheral resistance is extremely high (early pregnancy, hypertension), it is sufficient to use simple indices such as the S/D ratio or RI. The qualitative analysis of Doppler waveforms would mainly be useful for detecting a postsystolic notch and has not found wide application12,36. Establishing normal values. We performed transvaginal Doppler velocimetric studies of the uterine artery in singleton pregnancies from 7 to 40 weeks’ gestation in order to establish normal values6. We analyzed the data from 88 women. The criteria for enrollment in the study were an ultrasound examination in early pregnancy for accurate dating, an uncomplicated course of pregnancy, and a birthweight within normal limits. Early pregnancy. Figure 13.1 shows a coronal scan through the parametrium demonstrating the uterine artery and a Doppler waveform pattern that is typical of early pregnancy, i.e., high pulsatility with high systolic flow velocities and low end-diastolic velocities. The further progression of pregnancy is marked by an increase in the flow velocities, especially during diastole, causing a significant decrease in the S/D ratio (Fig. 13.2). Fig. 13.1 Example of an original transvaginal pulsed Doppler scan of the left uterine artery in the first trimester of pregnancy. Transverse scan through the uterine wall at the level of the isthmus shows numerous color-encoded vessels of small caliber. The Doppler sample volume is positioned in the descending branch of the left uterine artery. The peripheral resistance is still high at this stage, and consequently the diastolic flow velocities are low. Second and third trimesters. The greatest changes in our study were observed at the start of the second trimester. We saw no significant increase in diastolic flow velocity after the end of the second trimester. The mean S/D ratio was 5.44 in the first trimester and 2.20 in the third trimester, while the pulsatility index fell from 2.59 to 1.32 (Figs. 13.3 and 13.4). Differences between the sides.
Conditions of Intrauterine Life
Physical Principles
Anatomical and Physiological Principles
Adaptive Processes during Pregnancy
 S/D ratio of the uterine arteries < 3, difference between the sides < 1
S/D ratio of the uterine arteries < 3, difference between the sides < 1
 S/D ratio of the arcuate arteries < 2
S/D ratio of the arcuate arteries < 2
Technique of Transvaginal Pulsed Doppler Flowmetry
Authors’ Studies
Uterine Perfusion in a Normal Pregnancy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree