Evaluation of Adrenal Function
Walter L. Miller
The clinical features of adrenal insufficiency or excess are discussed in Chapters 534 and 535, respectively. The diagnostic evaluation of adrenal function is primarily dependent on laboratory measurements that determine the circulating levels of various steroids and hormones, often following perturbations of the system that help localize pathology. Clinical symptoms and signs generally lack sensitivity or specificity, and imaging studies are rarely helpful.
 MEASUREMENT OF PLASMA CONCENTRATIONS OF CORTISOL AND OTHER STEROIDS
MEASUREMENT OF PLASMA CONCENTRATIONS OF CORTISOL AND OTHER STEROIDS
Measurement of the plasma concentrations of cortisol and other circulating steroids screens for adrenal disorders and may provide clues regarding specific enzymatic deficiencies. Tables 532-1 and 532-2 summarize the normal plasma concentrations for a variety of steroids. With the notable exception of dehydroepiandrosterone sulfate (DHEAS), most adrenal steroids exhibit a diurnal variation based on the diurnal rhythm of corticotropin (ACTH). Because the stress of illness or hospitalization can increase adrenal steroid secretion and because diurnal rhythms may not be well established prior to 3 years of age, it is best to obtain two or more samples for the measurement of any steroid.1-5
Plasma cortisol is measured by radioimmunoassay, immunoradiometric assay, or high-performance liquid chromatography (HPLC). Newborn plasma contains mainly cortisone rather than cortisol during the first few days of life. Therefore, comparison of newborn data obtained by HPLC to published standards obtained by immunoassays may incorrectly suggest adrenal insufficiency. It is important to assure that the assays used are sufficiently sensitive to detect hormone levels that are pathologic in children but may be below the limit of detection in some assays designed for adult laboratories. This is especially true for the measurement of sex steroids.
 URINARY STEROID EXCRETION
URINARY STEROID EXCRETION
Examination of the total 24-hour excretion of steroids eliminates the fluctuations seen in serum samples as a function of time of day, episodic bursts of corticotropin (ACTH) and steroid secretion, and transient stress (eg, clinic visit, difficult venipuncture). Two consecutive 24-hour collections should be obtained, and each should be assayed for creatinine to monitor the completeness of the collection. Because of the diurnal and episodic nature of steroid secretion, one cannot obtain 8- or 12-hour collections and infer the 24-hour excretory rate from partial collections.
Table 532-1. Mean Sex Steroid Concentration in Infants and Children
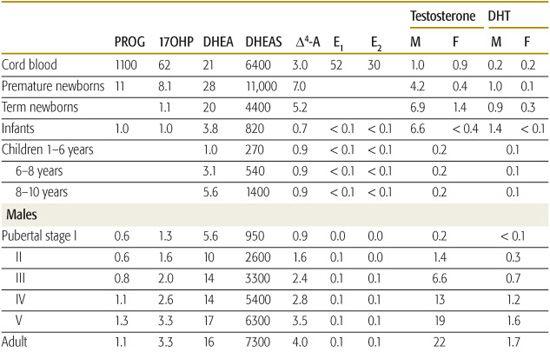
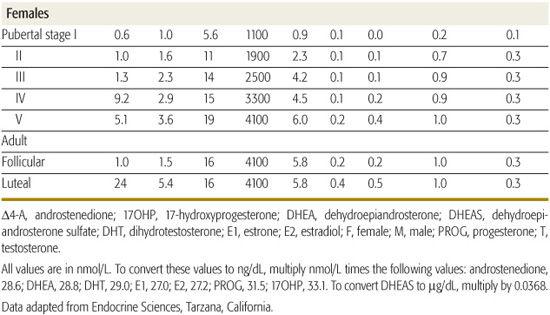
Table 532-2. Mean Glucocorticoid and Mineralocorticoid Concentrations
Urinary 17-hydroxycorticosteroids (17OHCS) measure the major urinary metabolites of cortisol, cortisone, and 11-deoxycortisol, which will be increased in 11-hydroxylase deficiency or after treatment with metyrapone, a commonly used diagnostic agent.  In most centers, measurement of 17OHCS has been replaced by measurement of urinary free cortisol, which avoids problems of nonspecificity and drug interference inherent in 17OHCS measurement. Excretion of urinary free cortisol and of total cortisol metabolites is closely correlated with age, body surface area, and adiposity, but are typically 11 ± 5 μg/m2/day.6,7 Other urinary steroid tests, such as 17-ketosteroids (17KS), which measures metabolites of dehydroepiandrosterone (DHEA) and dehydroepiandrosterone sulfate (DHEAS) and thus correlates with adrenal androgen production, may be helpful; however, measurements of 17-ketogenic steroids, a crude measure of glucocorticoids, are outmoded, unreliable, and should not be used.
In most centers, measurement of 17OHCS has been replaced by measurement of urinary free cortisol, which avoids problems of nonspecificity and drug interference inherent in 17OHCS measurement. Excretion of urinary free cortisol and of total cortisol metabolites is closely correlated with age, body surface area, and adiposity, but are typically 11 ± 5 μg/m2/day.6,7 Other urinary steroid tests, such as 17-ketosteroids (17KS), which measures metabolites of dehydroepiandrosterone (DHEA) and dehydroepiandrosterone sulfate (DHEAS) and thus correlates with adrenal androgen production, may be helpful; however, measurements of 17-ketogenic steroids, a crude measure of glucocorticoids, are outmoded, unreliable, and should not be used.
 MEASUREMENT OF PLASMA RENIN
MEASUREMENT OF PLASMA RENIN
Plasma renin measurement is useful in the evaluation of hypertension and in management of congenital adrenal hyperplasia (CAH). Renin is generally measured by its enzymatic activity: plasma renin activity (PRA) is an immunoassay of the amount of angiotensin I generated per milliliter of serum per hour at 37°C. PRA is sensitive to dietary sodium intake, posture, diuretic therapy, activity, and sex steroids. Because PRA can vary widely, it should be measured twice: once in the morning after overnight supine posture and then again after maintenance of upright posture for 4 hours.8 A simultaneous 24-hour urine for total sodium excretion is generally needed to interpret PRA results. Decreased dietary sodium, decreased intravascular volume, diuretics, and estrogens will increase PRA. Sodium loading, hyperaldosteronemia, and increased intravascular volume decrease PRA.
 DEXAMETHASONE SUPPRESSION TEST
DEXAMETHASONE SUPPRESSION TEST
Dexamethasone, a potent synthetic glucocorticoid, will suppress secretion of pituitary corticotropin (ACTH) and of adrenal cortisol. The dexamethasone suppression test remains useful for distinguishing whether glucocorticoid excess is caused by pituitary or adrenal disease. Dexamethasone also suppresses adrenal androgen secretion, and hence can distinguish between adrenal and gonadal sources of sex steroids. The classic dexamethasone suppression test is described in Chapter 535. A single dose of 1.0 mg in adults9-11 or 0.3 mg/m2 in children12 is useful for distinguishing Cushing syndrome from exogenous obesity.
 STIMULATION TESTS
STIMULATION TESTS
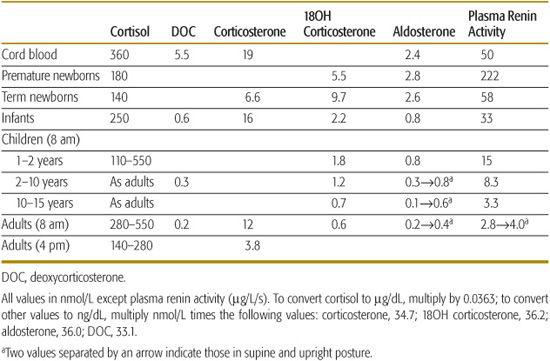
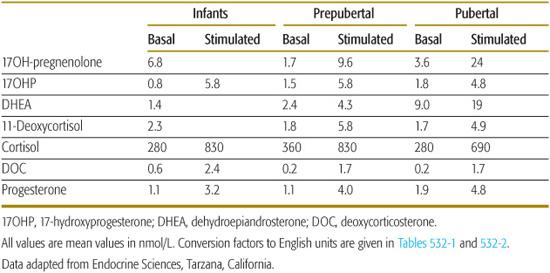
Corticotropin (ACTH) tests are essential for diagnosing all forms of congenital adrenal hyperplasia (CAH). Stimulating the adrenal with ACTH increases steroidogenesis, resulting in accumulation of steroids proximal to the disordered enzyme. A single bolus of synthetic ACTH (1-24) (cosyntropin) is administered intravenously, and cortisol and possibly other steroids are measured at 0 and 60 minutes.13 Normal responses to a 60-minute test are shown in Table 532-3.14 The usual dose is 15 mg/kg in children as old as 2 years, and 0.25 mg for children older than 2 years and adults. Comparing the patient’s basal to ACTH-stimulated values of 17OHP against those from large numbers of well-studied patients usually permits the discrimination of normal persons, heterozygotes, patients with nonclassical CAH, and patients with classical CAH, although there inevitably is some overlap between groups.16
Table 532-3. Responses of Adrenal Steroids to a 60-Minute Corticotropin (ACTH) Test
 METYRAPONE TEST
METYRAPONE TEST
Metyrapone testing is done to assess the capacity of the pituitary to produce corticotropin (ACTH) in response to a physiologic stimulus. Patients with a previous history of hypothalamic, pituitary, or adrenal disease, or those who have been withdrawn from glucocorticoid therapy can be evaluated with a metyrapone test to predict if they will respond normally to stressors such as surgery. Metyrapone blocks the action of P450c11β, which results in decreased cortisol secretion and subsequent increased ACTH secretion.
Metyrapone is given orally as 300 mg/m2 every 4 hours for a total of six doses (not to exceed 3 g total dose in 24 h).19 Blood is obtained for cortisol, 11-deoxycortisol, and ACTH at 8AM before and after the test, and a 24-hour urine collection should be obtained for 17OHCS before and during the test. In a normal response to metyrapone, cortisol decreases, ACTH increases, and 11-deoxycortisol increases greatly, to about 5 μg/dL.19
 IMAGING STUDIES
IMAGING STUDIES
Positive findings on imaging studies of the pituitary or adrenal may be useful, but absence of findings does not exclude pituitary or adrenal disease. CT may rarely detect pituitary tumors that secrete corticotropin (ACTH), but MRI with gadolinium enhancement is more sensitive, even though it will only detect less than half of these. Adrenal imaging may recognize enlargement of the adrenals in Cushing disease or congenital adrenal hyperplasia (CAH), but such enlargement is often not detectable by imaging techniques with any useful degree of certainty. In lipoid CAH, the adrenals are grossly enlarged, and they are hypoplastic in congenital adrenal hypoplasia or in the hereditary ACTH unresponsiveness syndrome. Many malignant tumors can be diagnosed by imaging studies, but many adrenal adenomas are too small to be detected.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


