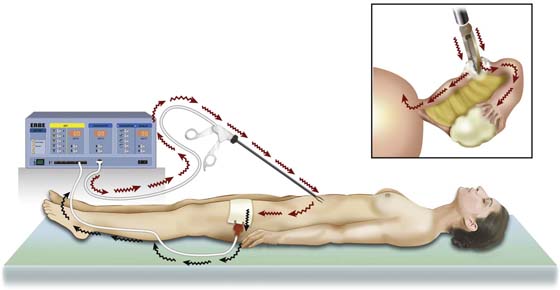
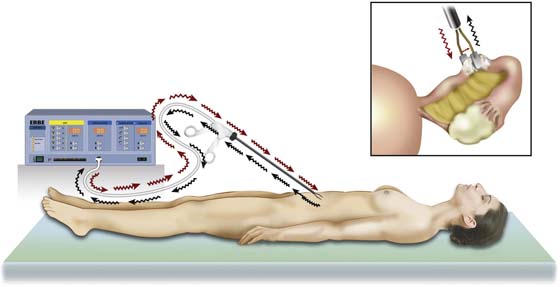
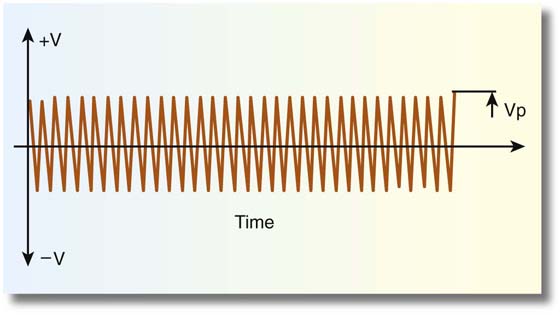
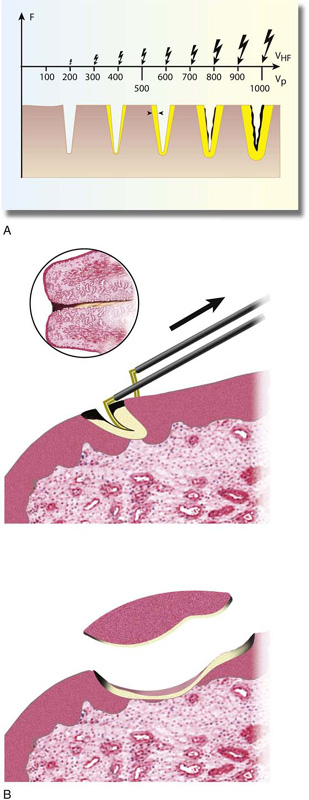
CHAPTER 5 Energy-releasing devices have been used in the past and currently are employed in pelvic surgery. The raison d’être for such tools consists of hemostasis and speed. Compared with cold knife or scissor cutting, energy devices create a greater degree of surrounding tissue damage, usually in the form of thermal injury leading to necrosis, devitalization, subsequent fibrosis, and scar formation. Because of the aforesaid events, tissues neighboring the operative site are vulnerable to injury by a variety of mechanisms. The surgeon, his or her assistants, and supporting nursing staff must be fully acquainted with these devices and with the mechanisms by which each device produces desired and undesired actions. The aforesaid exercise is intended to protect a patient from unintended injury. Two terms misused relative to electrosurgery are cautery and bovie. A cautery is rarely used in a modern operating room. It refers to heating of a conducting metal (e.g., an iron poker, a branding iron, an electric stove top heating element) until it has reached sufficient temperature such that the iron glows red. The heat of the device makes direct contact (e.g., severed limb stump), thereby cauterizing open vessels and quenching the flow of blood. In 1928, William Bovie, a physicist, and Harvey Cushing, a neurosurgeon, developed an electrosurgical unit capable of cutting and coagulating. The Bovie unit was thus an early spark gap generator, which has been for many years obsolete. Contemporary microprocessor-controlled electrosurgical units are not Bovie units. The following four terms are of key import for understanding the physics and tissue interactions of electrosurgery units: current voltage resistance power Current refers to the flow of electrical charges. Without current flow, no electrosurgical action would happen. It is measured in amps (Amperes). The action of the electric generator produces a current within a complete electrical circuit. Current flows in the direction of positive charges. For work to be accomplished, electrical charges must be moved from one point to another (i.e., the difference in potential between two points is expressed as volts [a potential force]). Impedance to the conduction of electrical current through a given medium is referred to as its resistance and is expressed in ohms. The relationship of current, potential, and resistance is expressed as Ohm’s law: Power is equivalent to work performed over a period of time and is expressed in watts. or Two major types of current flow are described: direct and alternating. In the United States, electrosurgery utilizes radio-requency (RF) (>100,000 Hertz or cycles per second) alternating current to cut or coagulate tissue. A monopolar circuit travels from the electrosurgical unit (ESU) via a copper wire to an electrode, where vaporization (100°C) [i.e., cutting or coagulation] (60°C) occurs. The current is then conducted through the patient’s body, usually via the great blood vessels, and is returned to the ESU via a neutral electrode (ground plate), which is also connected by a copper wire to the ESU (Fig. 5–1). A bipolar circuit consists of two wires leaving the ESU; the first wire is connected through a two-part electrode to the portion that serves as the active electrode. The second portion, which serves as the return or neutral electrode, is connected to the second wire, which returns the current to the ESU. The advantage of the bipolar system is obvious. Electrical current flows only between active and neutral electrodes. Tissue action is observed only between the electrodes. Thus no current will traverse the patient’s entire body, as is the case with monopolar circuits (Fig. 5–2). Cutting versus coagulation waveforms can be visualized on an oscilloscope (Fig. 5–3). Cutting is distinguished by (unmodulated) sine wave form characterized by high current flow, low peak-to-peak voltage, and rapid attainment of high tissue temperatures (e.g., 100°C) with attendant cellular vaporization. The best cutting and least coagulation artifacts occur with peak voltages ranging from 200 to 600 volts (Fig. 5–4A, B). In contrast, electrocoagulation is modulated and exhibits lower current flow and higher voltages (Fig. 5–5). During coagulation, heating occurs less rapidly and at lower temperatures (60°C–70°C), rendering the cell dried or desiccated, because ions and water are driven out of the cells; resistance to flow increases as the cells lose conducting ions. Fulguration (spray coagulation) occurs when the coagulating electrode is held close to the tissue target but does not touch the tissue. Here very high voltages are required to allow the spark to jump across the air space and coagulate the cells. Typically, fulguration creates superficial coagulation as opposed to deeper penetrating contact coagulation (Fig. 5–6). FIGURE 5–1 This illustration shows the electrical current flow with a monopolar circuit. Active current leaves the electrosurgical unit (ESU) and flows through the grasping forceps to create high current density where the forceps jaws close on the tissue (inset). The current is conducted through the patient’s body to exit over a large surface area (ground plate) and return to the ESU. FIGURE 5–2 This illustrates a bipolar circuit. The current form in the electrosurgical unit (ESU) flows through an insulated conductor of the bipolar forceps to exert its thermal action on the tissue (inset). The current flows from the active jaw (electrode) to the inactive (neutral) jaw of the electrode. The current flows back to the ESU via the insulated neural limb of the bipolar forceps. Note that current flow to tissue is limited to that which is enclosed between active and neutral electrodes (forceps jaws). FIGURE 5–3 A typical oscilloscopic pattern for “cutting current.” Note that the peak-to-peak voltage is relatively low and there is no modulation of amplitude. Current flow is high. FIGURE 5–4 A. As voltage increases, the relative size of the electrical spark also increases. The effect on tissue of increased voltage is an increase in the area of coagulation artifact. B. A cutting loop electrode is illustrated here cutting into the cervix. The electrosurgical unit (ESU) foot pedal is activated just before the loop makes contact with the cervix. This creates an open circuit. Relatively high voltages are created as the electrode encounters the cervix. This is notable by high resistance and high thermal temperatures, thereby creating carbon formation (black). As voltage is diminished, current flow is picked up and the tissue is vaporized with little coagulation artifact. When the electrode exits, high temperatures again create thermal artifact.
Energy Devices
Electrosurgery—Laser—Harmonic Scalpel
Electrosurgery



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree