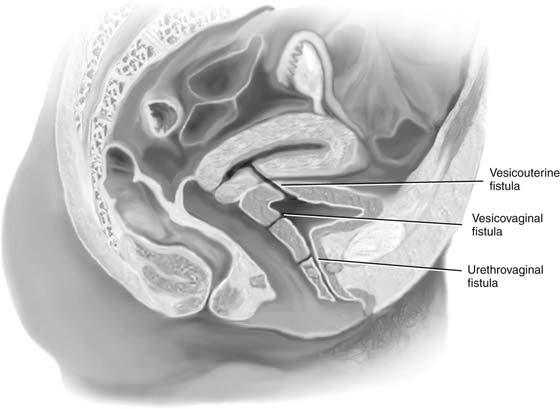
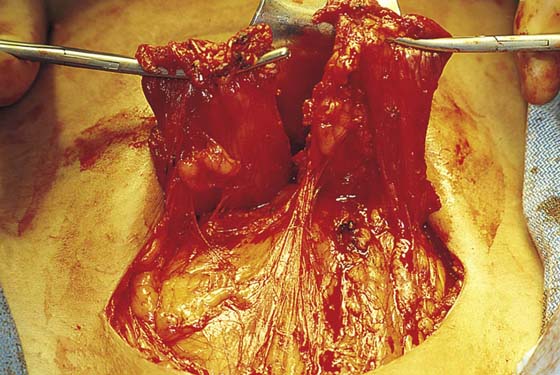
CHAPTER 89 Lower urinary tract fistulas can communicate with the vagina or the uterus (Fig. 89–1). Although the indications for abdominal repair of vesicovaginal fistula are somewhat controversial, certain conditions involving the bladder are best approached via an abdominal route. These include high and inaccessible fistulas, multiple fistulas, involvement of uterus or bowel, and the need for ureteral reimplantation. A midline or transverse skin incision can be made. A midline incision will allow easier access to the abdomen for retrieval and mobilization of omentum. If a transverse incision is utilized, often a muscle-splitting incision such as a Maylard or Cherney incision (Fig. 89–2) will facilitate exposure. Once the peritoneum has been opened, the bowel is packed posteriorly and usually a self-retaining retractor is placed. The bladder is then exposed, and a high extraperitoneal intentional cystotomy is made (see previous section on opening and closing the bladder). The fistulous tract is then visualized from the inside of the bladder (Figs. 89–3 and 89–4). If it is in close proximity to the ureteral orifices, ureteral stents should be placed (Fig. 89–5). They can be placed via a cystoscopic approach or intraoperatively via a transvesical approach. The bladder incision is then taken down along the back of the bladder all the way to the fistulous tract (Figs. 89–6 and 89–7). The fistulous tract is completely excised, and the vagina is sharply mobilized off the back of the bladder (Fig. 89–8). A pack or EEA (end-to-end anastomosis) sizer placed in the vagina will produce vaginal distention and facilitates countertraction, which assists the dissection. Traction and countertraction on the vagina and bladder facilitate sharp accurate separation of these two surfaces (Fig. 89–9). It is important to proceed with this dissection well beyond any scarification produced by the fistula (see Figs. 89–9 and 89–10). The vagina is then closed with interrupted 2-0 absorbable sutures, preferably in two layers (see Figs. 89–10 and 89–11). The bladder is closed with 3-0 absorbable sutures in a running fashion or with interrupted sutures. The bladder is also preferably closed in two layers (see Figs. 89–10 through 89–12). It is usually advantageous to mobilize a piece of omentum down to the site of the fistula repair. It is sutured to the anterior wall of the vagina or the posterior wall of the bladder to thus give additional blood supply and a tissue barrier between the suture lines (Figs. 89–13 and 89–14). Fig. 89–15 shows the inside of the bladder after closure and repair of the fistula. Fig. 89–16 is a drawing of the completed repair. Fig. 89–17 reviews again, in a stepwise fashion, the abdominal repair of a vesicovaginal fistula. Catheter drainage may be accomplished with a transurethral or suprapubic catheter (or both), depending on the extent and circumstances of the repair. FIGURE 89–1 Lower urinary tract fistulas can communicate with the vagina or the uterus. The extent of the fistula and the anatomic location are important factors to be considered when deciding whether to approach the repair vaginally or transabdominally. FIGURE 89–2 Low transverse muscle-cutting incision of the Cherney variety. Note that the muscle is detached from the pubic bone very low near its insertion. The peritoneum is then usually opened transversely. FIGURE 89–3
Abdominal Repair of Vesicovaginal and Vesicouterine Fistula
Abdominal Repair of Vesicovaginal Fistula
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree