Figure 12–1. Correct positioning of the child younger than 8 years for optimal airway alignment: a folded sheet or towel is placed beneath the shoulders to accommodate the occiput and align the oral, pharyngeal, and tracheal airways.
Figure 12–1. Correct positioning of the child younger than 8 years for optimal airway alignment: a folded sheet or towel is placed beneath the shoulders to accommodate the occiput and align the oral, pharyngeal, and tracheal airways.
2. Perform the head tilt/chin lift or jaw thrust maneuver (Figure 12–2). Lift the chin upward while avoiding pressure on the submental triangle, or lift the jaw by traction upward on the angle of the jaw. Head tilt/chin lift must not be done if cervical spine injury is possible. (See section Approach to the Pediatric Trauma Patient, later.)
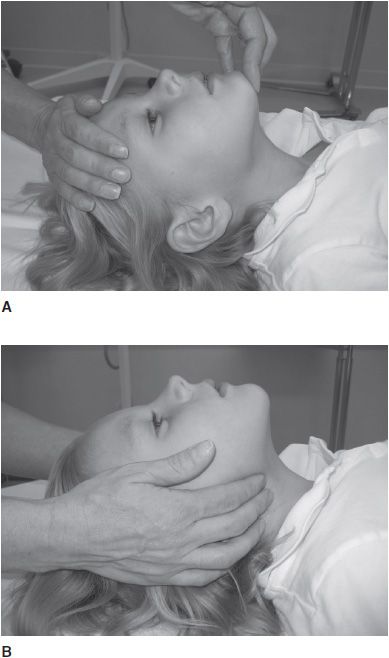
 Figure 12–2. A: Opening the airway with the head tilt and chin lift in patients without concern for spinal trauma: gently lift the chin with one hand and push down on the forehead with the other hand. B: Opening the airway with jaw thrust in patients with concern for spinal trauma: lift the angles of the mandible; this moves the jaw and tongue forward and opens the airway without bending the neck.
Figure 12–2. A: Opening the airway with the head tilt and chin lift in patients without concern for spinal trauma: gently lift the chin with one hand and push down on the forehead with the other hand. B: Opening the airway with jaw thrust in patients with concern for spinal trauma: lift the angles of the mandible; this moves the jaw and tongue forward and opens the airway without bending the neck.
3. Assess airway for foreign material. Suction the mouth; use Magill forceps to remove visible foreign bodies. Visualize by means of a laryngoscope if necessary. Blind finger sweeps should not be done.
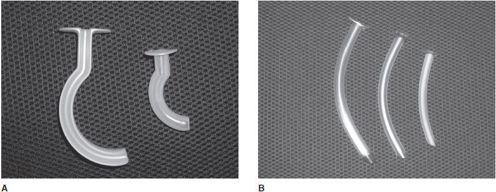
4. If airway obstruction persists, first attempt to reposition the head, then proceed with insertion of an airway adjunct, such as the oropharyngeal or nasopharyngeal airway (Figure 12–3). Such adjuncts relieve upper airway obstruction due to prolapse of the tongue into the posterior pharynx, the most common cause of airway obstruction in unconscious children. The correct size for an oropharyngeal airway is obtained by measuring from the upper central gumline to the angle of the jaw (Figure 12–4) and should be used only in the unconscious victim. Proper sizing is paramount, as an oropharyngeal airway that is too small will push the tongue further into the airway while one that is too large will mechanically obstruct the airway. Nasopharyngeal airways should fit snugly within the nares and should be equal in length to the distance from the nares to the tragus (Figure 12–5). This airway adjunct should be avoided in children with significant injuries to the midface due to the risk of intracranial perforation through a damaged cribriform plate.
 Figure 12–3. A: Oropharyngeal airways of various sizes. B: Nasopharyngeal airways of different sizes.
Figure 12–3. A: Oropharyngeal airways of various sizes. B: Nasopharyngeal airways of different sizes.
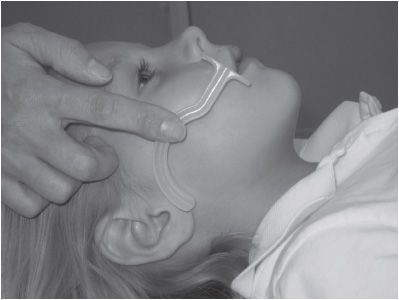
 Figure 12–4. Size selection for the oropharyngeal airway: hold the airway next to the child’s face and estimate proper size by measuring from the upper central gumline to the angle of the jaw.
Figure 12–4. Size selection for the oropharyngeal airway: hold the airway next to the child’s face and estimate proper size by measuring from the upper central gumline to the angle of the jaw.

 Figure 12–5. Size selection for the nasopharyngeal airway: hold the airway next to the child’s face and estimate proper size by measuring from the nares to the tragus.
Figure 12–5. Size selection for the nasopharyngeal airway: hold the airway next to the child’s face and estimate proper size by measuring from the nares to the tragus.
Breathing
Assessment of respiratory status is largely accomplished by inspection. Look for adequate and symmetrical chest rise and fall, rate and work of breathing (eg, retractions, flaring, and grunting), accessory muscle use, skin color, and tracheal deviation. Note the mental status. Pulse oximetry measurement and end-tidal CO2 determination, if available, are highly desirable. Listen for adventitious breath sounds such as wheezing. Auscultate for air entry, symmetry of breath sounds, and rales. Feel for subcutaneous crepitus.
If spontaneous breathing is inadequate, initiate positive-pressure ventilation with bag-valve mask ventilation (BMV) and 100% oxygen. Assisted ventilations should be coordinated with the patient’s efforts, if present. Effective BMV is a difficult skill that requires training and practice. To begin, ensure a proper seal by choosing a mask that encompasses the area from the bridge of the nose to the cleft of the chin. Form an E–C clamp around the mask to seal the mask tightly to the child’s face. The thumb and index finger form the “C” surrounding the mask, while the middle, ring, and small fingers lift the jaw into the mask (Figure 12–6). Use only enough force and volume to make the chest rise visibly. In the patient with a perfusing rhythm, administer one breath every 3–5 seconds (12–20 breaths/min). To more easily achieve this rate, recite the pneumonic “squeeze-release-release” in a normal speaking voice. Two-person ventilation using this technique is optimal. When proper technique is used, BMV is effective in the vast majority of cases.
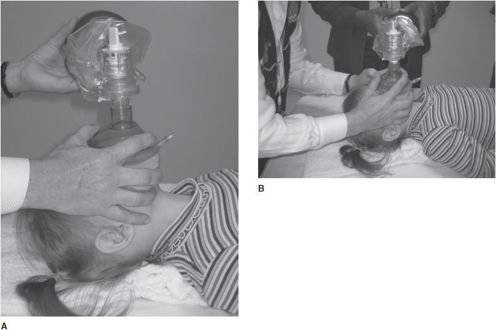
 Figure 12–6. A: Bag-valve-mask ventilation, one-person technique: the thumb and index finger form the “C” surrounding the mask, while the middle, ring, and little fingers lift the jaw into the mask. B: Bag-valve-mask ventilation, two-person technique: the first rescuer forms the “C” and “E” clamps with both hands; the second rescuer provides ventilation.
Figure 12–6. A: Bag-valve-mask ventilation, one-person technique: the thumb and index finger form the “C” surrounding the mask, while the middle, ring, and little fingers lift the jaw into the mask. B: Bag-valve-mask ventilation, two-person technique: the first rescuer forms the “C” and “E” clamps with both hands; the second rescuer provides ventilation.
Adequacy of ventilation is reflected in adequate chest movement and auscultation of good air entry bilaterally. Take care to avoid hyperventilation. Excessive ventilation leads to barotrauma, increased risk of aspiration, and a decreased likelihood that return of spontaneous circulation will be achieved during cardiac arrest. If the chest does not rise and fall easily with bagging, reposition the airway and assess for foreign material as previously described. The presence of asymmetrical breath sounds in a child in shock or in severe distress suggests pneumothorax and is an indication for needle thoracostomy. In small children, the transmission of breath sounds throughout the chest may impair the ability to auscultate the presence of a pneumothorax. Note: Effective oxygenation and ventilation are the keys to successful resuscitation.
Cricoid pressure (Sellick maneuver) during positive-pressure ventilation may decrease gastric inflation; however, it has not been shown to reduce the risk of aspiration and should only be used if it does not interfere with ventilation or the speed and ease of intubation. Advanced airway management techniques are described in the references accompanying this section. (See also section Approach to the Pediatric Trauma Patient.)
Circulation
The methodical assessment of perfusion is critical to the diagnosis of shock, which results from inadequate perfusion of vital organs. This diagnosis should be made rapidly by clinical examination detailed as follows.
A. Pulses
Check adequacy of peripheral pulses. Pulses become weak and thready only with severe hypovolemia. Compare peripheral pulses with central pulses. In the infant, central pulses should be checked at the brachial artery.
B. Heart Rate
Compare with age-specific norms. Tachycardia can be a nonspecific sign of distress; bradycardia for age is a sign of imminent arrest and necessitates aggressive resuscitation.
C. Extremities
Extremities become cooler from distal to proximal, as shock progresses. A child whose extremities are cool distal to the elbows and knees is in severe shock.
D. Capillary Refill Time
When fingertip pressure is applied to a patient’s distal extremity and then released, blood should refill the area in less than 2 seconds. A prolonged capillary refill time in the setting of other signs of shock indicates a compensated shock state. It is important to recognize that capillary refill time is influenced by ambient temperature, limp position, site, age of the patient, and room lighting.
E. Mental Status
Hypoxia, hypercapnia, or ischemia will result in altered mental status. Other important treatable conditions may also result in altered mental status, such as intracranial hemorrhage, meningitis, and hypoglycemia.
F. Skin Color
Pallor, gray, mottled, or ashen skin colors all indicate compromised circulatory status.
G. Blood Pressure
It is important to remember that shock may be present before the blood pressure falls below the normal limits for age. As intravascular volume falls, peripheral vascular resistance increases. Blood pressure is maintained until there is 35%–40% depletion of blood volume, followed by precipitous and often irreversible deterioration. Shock represents a continuum that progresses if left untreated. Shock that occurs with any signs of decreased perfusion but normal blood pressure is compensated shock. When blood pressure also falls, decompensated (hypotensive) shock is present. Blood pressure determination should be done manually, using an appropriately sized cuff, because automated machines can give erroneous readings in children.
MANAGEMENT OF SHOCK
IV access is essential but can be difficult to establish in children with shock. Peripheral access, especially via the antecubital veins, should be attempted first, but central cannulation should follow quickly if peripheral access is unsuccessful. Alternatives are percutaneous cannulation of femoral, subclavian, or internal or external jugular veins; cutdown at antecubital, femoral, or saphenous sites; or intraosseous (IO) lines (Figure 12–7). IO needle placement is an acceptable alternative in any severely ill child when venous access cannot be established rapidly (within 10 seconds). Both manual and automated insertion devices are available for pediatric patients. Increasing evidence suggests that automated devices result in faster, more successful IO placement compared to manual devices. Decisions on more invasive access should be based on individual expertise as well as urgency of obtaining access. Use short, wide-bore catheters to allow maximal flow rates. Two IV lines should be started in severely ill children. In newborns, the umbilical veins may be cannulated. Consider arterial access if beat-to-beat monitoring or frequent laboratory tests will be needed.

 Figure 12–7. Interosseous (IO) cannulation technique. The IO line is inserted by grasping the needle hub firmly with the palm of the hand and angling the needle tip perpendicular to the anterior tibial surface approximately two fingerbreadths distal to the tibial plateau. With a firm, twisting motion, advance the needle until a sudden lessening of resistance is felt as the needle enters the marrow space. Aspiration of blood and marrow confirms IO placement.
Figure 12–7. Interosseous (IO) cannulation technique. The IO line is inserted by grasping the needle hub firmly with the palm of the hand and angling the needle tip perpendicular to the anterior tibial surface approximately two fingerbreadths distal to the tibial plateau. With a firm, twisting motion, advance the needle until a sudden lessening of resistance is felt as the needle enters the marrow space. Aspiration of blood and marrow confirms IO placement.
Differentiation of Shock States & Initial Therapy
Therapy for inadequate circulation is determined by the cause of circulatory failure.
A. Hypovolemic Shock
The most common type of shock in the pediatric population is hypovolemia. Frequent causes include dehydration, diabetes, heat illness, hemorrhage, and burns. Normal saline or lactated Ringer solution (isotonic crystalloid) is given as initial therapy in shock and should be initiated even in normotensive patients. There is no advantage to the early administration of colloid (albumin). Give 20 mL/kg body weight and repeat as necessary, until perfusion normalizes. Children tolerate large volumes of fluid replacement and frequent reassessment is necessary. Typically, in hypovolemic shock, no more than 60 mL/kg is needed, but more may be required if ongoing losses are severe. Appropriate monitoring and reassessment will guide your therapy. Packed red blood cell transfusion is indicated in trauma patients not responding to initial crystalloid bolus fluid replacement; however, there is insufficient evidence to determine the volume required. Pressors are not required in simple hypovolemic states.
B. Distributive Shock
Distributive shock results from increased vascular capacitance with normal circulating volume. Examples are sepsis, anaphylaxis, and spinal cord injury. Initial therapy is again isotonic volume replacement with crystalloid, but pressors may be required if perfusion does not normalize after delivery of two or three 20-mL/kg boluses of crystalloid. If necessary, pressors may be initiated through a peripheral line until central access is obtained. Outcomes improve when threshold heart rates, normalized blood pressure, and a capillary refill in less than 2 seconds are achieved within the first hour of symptom onset. Children in distributive shock must be admitted to a pediatric intensive care unit.
The most recent clinical practice parameters from the American College of Critical Care Medicine emphasized four key concepts when faced with the pediatric or neonatal patient in septic shock. When compared to adults, infants and children are more likely to require (1) proportionally more fluid; (2) early inotrope or vasodilator therapy; (3) hydrocortisone for absolute adrenal insufficiency (caused by severe illness); (4) ECMO (extracorporeal membrane oxygenation) for refractory shock.
C. Cardiogenic Shock
Cardiogenic shock can occur as a complication of congenital heart disease, myocarditis, dysrhythmias, ingestions (eg, clonidine, cyclic antidepressants), or as a complication of prolonged shock due to any cause. The diagnosis is suggested by any of the following signs: abnormal cardiac rhythm, distended neck veins, rales, abnormal heart sounds such as an S3 or S4, friction rub, narrow pulse pressure, rales, or hepatomegaly. Chest radiographs may show cardiomegaly and pulmonary edema. An initial bolus of crystalloid may be given, but pressors, and possibly afterload reducers, are necessary to improve perfusion. Giving multiple boluses of fluid is deleterious. Comprehensive cardiopulmonary monitoring is essential. Children in cardiogenic shock must be admitted to a pediatric intensive care unit.
D. Obstructive Shock
Obstructive shock is rare in the pediatric population and involves extracardiac obstruction of blood flow and/or obstruction of adequate diastolic filling. Examples include cardiac tamponade, tension pneumothorax, massive pulmonary embolism, or a critical coarctation of the aorta after closure of the ductus arteriosus. Management is directed toward resolution of the obstruction. In the case of a critical coarctation, management should include prostaglandin initiation to reopen the ductus arteriosus while awaiting surgical repair.
 Observation & Further Management
Observation & Further Management
Clinically reassess physiologic response to each fluid bolus to determine additional needs. Serial central venous pressure determinations or a chest radiograph may help determine volume status. Place an indwelling urinary catheter to monitor urine output.
Caution must be exercised with volume replacement if intracranial pressure (ICP) is potentially elevated, as in severe head injury, diabetic ketoacidosis, or meningitis. Even in such situations, however, normal intravascular volume must be restored in order to achieve adequate mean arterial pressure and thus cerebral perfusion pressure.
SUMMARY OF RESUSCITATING THE ACUTELY ILL INFANT OR CHILD
Assess the ABCs in sequential fashion and, before assessing the next system, immediately intervene if physiologic derangement is detected. It is essential that each system be reassessed after each intervention to ensure improvement and prevent failure to recognize clinical deterioration.
APLS (the pediatric emergency medicine resource): http://www.aplsonline.com.
Brierley J, Carcillo JA, Choong K et al: Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med 2009; 37(2):666–688 [PMID: 19325359].
Chameides L et al (eds): PALS Provider Manual. American Heart Association; 2011.
ECC Committee, Subcommittees and Task Forces of the American Heart Association: Part 13: pediatric basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S862–S875 [PMID: 20956229].
ECC Committee, Subcommittees and Task Forces of the American Heart Association: Part 14: pediatric advanced life support: 2010 American Heart Association guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122;S876–S908 [PMID: 20956230].
Tobias JD, Ross AK: Intraosseous infusions: a review for the anesthesiologist with a focus on pediatric use. Anesth Analg 2010;110(2):391–401 [PMID: 19897801].
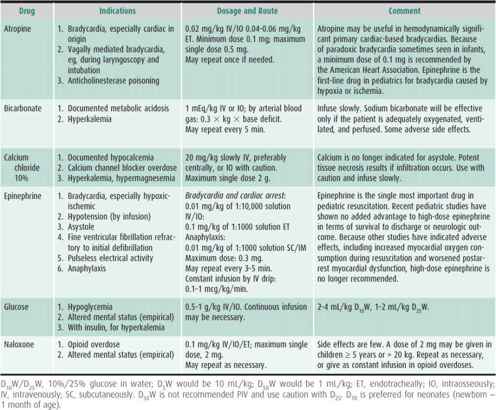
EMERGENCY PEDIATRIC DRUGS
Although careful attention to airway and breathing remains the mainstay of pediatric resuscitation, medications are often needed. Rapid delivery to the central circulation, which can be via peripheral IV catheter, is essential. Infuse medications close to the catheter’s hub and flush with saline to achieve the most rapid systemic effects. In the rare instance that no IV or IO access is achievable, some drugs may be given by endotracheal tube (Table 12–1). However, the dose, absorption, and effectiveness of drugs given via this route are either unknown or controversial. The use of length-based emergency measuring tapes that contain preprinted drug dosages, equipment sizes, and IV fluid amounts (Broselow tapes) or preprinted resuscitation drug charts is much more accurate than estimation formulas and helps minimize dosing errors. Selected emergency drugs used in pediatrics are summarized in Table 12–2.
Table 12–1. Emergency drugs that may be given by endotracheal tube.
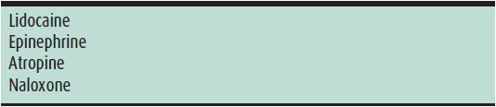
Table 12–2. Emergency pediatric drugs.
APPROACH TO THE ACUTELY ILL INFANT OR CHILD
An unstable patient may present with a known diagnosis or in cardiorespiratory failure of unknown cause. The initial approach must rapidly identify the injuries, prioritize management, and reverse life-threatening conditions.
PREPARATION FOR EMERGENCY MANAGEMENT
Resuscitation occurs simultaneously at two levels: rapid cardiopulmonary assessment, with indicated stabilizing measures, while venous access is gained, and cardiopulmonary monitoring initiated. The technique of accomplishing these concurrent goals is outlined as follows:
1. If advance notice of the patient’s arrival has been received, prepare a resuscitation room and summon appropriate personnel and subspecialty expertise as needed.
2. Assign team responsibilities, including a team leader plus others designated to manage the airway, perform chest compressions, achieve access, draw blood for laboratory studies, place monitors, gather additional historical data, and provide family support.
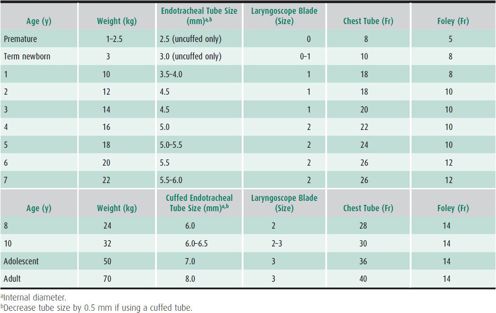
3. Age-appropriate equipment (including laryngoscope blade, endotracheal tubes, nasogastric or orogastric tubes, IV lines, and an indwelling urinary catheter) and monitors (cardiorespiratory monitor, pulse oximeter, and appropriate blood pressure cuff) should be assembled and readily available. Use a length-based emergency tape if available. See Table 12–3 for endotracheal tube sizes. Cuffed endotracheal tubes are acceptable during the inpatient setting for children and infants beyond the newborn period. Cuff inflation pressures must be carefully monitored and maintained below 20 cm H2O. In certain circumstances, such as poor lung compliance or high airway resistance, the use of cuffed tubes may be preferable in controlled settings.
RECEPTION & ASSESSMENT
Upon patient arrival, the team leader begins a rapid assessment as team members perform their assigned tasks. If the patient is received from prehospital care providers, careful attention must be paid to their report, which contains information that they alone have observed. Interventions and medications should be ordered only by the team leader to avoid confusion. The leader should refrain from personally performing procedures. A complete timed record should be kept of events, including medications, interventions, and response to intervention.
All Cases
In addition to cardiac compressions and ventilation, ensure that the following are instituted:
1. Hundred percent high-flow oxygen.
2. Cardiorespiratory monitoring, pulse oximetry, and end-tidal CO2 if the patient is intubated.
3. Vascular (peripheral, IO, or central) access; two lines preferred.
4. Blood drawn and sent. Bedside blood glucose determination is essential.
5. Full vital signs.
6. Clothes removed.
7. Foley catheter and nasogastric or orogastric tube inserted.
8. Complete history.
9. Notification of needed consultants.
10. Family support.
11. Law enforcement or security activation and emergency unit lockdown for cases involving potential terrorism, gang violence, or threats to staff or family.
As Appropriate
1. Immobilize neck.
2. Obtain chest radiograph (line and tube placement).
3. Insert central venous pressure and arterial line.
Kleinman ME et al: Pediatric basic and advanced life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Pediatrics 2010;126(5):e1261–e1318 [PMID: 20956433].
Mandt MJ, Rappaport LD: Update in pediatric resuscitation. Adv Pediatr 2009;56:359–385 [PMID: 19968956].
Waltzman ML, Mooney DP: Chapter 105: Major trauma. In: Fleisher GR et al (eds): Textbook of Pediatric Emergency Medicine, 6th ed. Lippincott Williams & Wilkins; 2010:1244–1255.
APPROACH TO THE PEDIATRIC TRAUMA PATIENT
Traumatic injuries, including motor vehicle crashes, falls, burns, and immersions, account for the greatest number of deaths among children older than 1 year; injury exceeds all other causes of death combined. A team approach to the severely injured child, using assigned roles as outlined in the preceding section, will optimize outcomes. A calm atmosphere in the receiving area will contribute to thoughtful care. Analgesia and sedation must be given to stable patients. Parents are often anxious, angry, or guilty, requiring ongoing support from staff, social workers, or child life workers (therapists knowledgeable about child development).
To provide optimal multidisciplinary care, regional pediatric trauma centers provide dedicated teams of pediatric specialists in emergency pediatrics, trauma surgery, orthopedics, neurosurgery, and critical care. However, most children with severe injuries are not seen in these centers. Primary care providers must be able to provide initial assessment and stabilization of the child with life-threatening injuries before transport to a verified pediatric trauma center.
MECHANISM OF INJURY
Document the time of occurrence, the type of energy transfer (eg, hit by a car, rapid deceleration), secondary impacts (if the child was thrown by the initial impact), appearance of the child at the scene, interventions performed, and clinical condition during transport. The report of emergency service personnel is invaluable. Forward all of this information with the patient to the referral facility if secondary transport occurs.
Trauma in children is predominantly blunt, with penetrating trauma occurring in 10% of cases. Head and abdominal injuries are particularly common and important.
INITIAL ASSESSMENT & MANAGEMENT
The vast majority of children who reach a hospital alive survive to discharge. As most deaths from trauma in children are due to head injuries, cerebral resuscitation must be the foremost consideration when treating children with serious injuries. Strict attention to the ABCs (airway, breathing, circulation) ensures optimal oxygenation, ventilation, and perfusion, and ultimately, cerebral perfusion.
The primary and secondary survey is a method for evaluating and treating injured patients in a systematic way that provides a rapid assessment and stabilization phase, followed by a head-to-toe examination and definitive care phase.
PRIMARY SURVEY
The primary survey is designed to immediately identify and treat all physiologic derangements resulting from trauma.
Airway, with cervical spine control
Breathing
Circulation, with hemorrhage control
Disability (neurologic deficit)
Exposure (maintain a warm Environment, undress the patient completely, and Examine)
If the patient is apneic or has agonal breaths, the sequence becomes the CABs (chest compressions, open the airway, provide two rescue breaths). Please refer to pediatric advanced life support guidelines for further information. Refer to preceding discussion regarding details of the ABC assessment. Modifications in the trauma setting are added as follows.
Airway
Failure to manage the airway appropriately is the most common cause of preventable morbidity and death. Administer 100% high-flow oxygen to all patients. Initially, provide cervical spine protection by manual inline immobilization, not traction. A hard cervical spine collar is applied after the primary survey.
Breathing
Most ventilation problems are resolved adequately by the airway maneuvers described earlier and by positive-pressure ventilation. Sources of traumatic pulmonary compromise include pneumothorax, hemothorax, pulmonary contusion, flail chest, and central nervous system (CNS) depression. Asymmetrical breath sounds, particularly with concurrent tracheal deviation, cyanosis, or bradycardia, suggest pneumothorax, possibly under tension. To evacuate a tension pneumothorax, insert a large-bore catheter-over-needle assembly attached to a syringe through the second intercostal space in the midclavicular line into the pleural cavity and withdraw air. If a pneumothorax or hemothorax is present, place a chest tube in the fourth or fifth intercostal space in the anterior axillary line. Connect to water seal. Insertion should be over the rib to avoid the neurovascular bundle that runs below the rib margin. Open pneumothoraces can be treated temporarily by taping petrolatum-impregnated gauze on three sides over the wound, creating a flap valve.
A child with a depressed level of consciousness (Glasgow Coma Scale [GCS] score < 9), a need for prolonged ventilation, severe head trauma, or an impending operative intervention requires endotracheal intubation after bag-mask preoxygenation. Orotracheal intubation is the route of choice and is possible without cervical spine manipulation. Nasotracheal intubation may be possible in children 12 years of age or older who have spontaneous respirations, if not contraindicated by midfacial injury.
Supraglottic devices, such as the laryngeal mask airway (LMA), are being used with increasing frequency, in both the prehospital and hospital settings. The device consists of a flexible tube attached to an inflatable rubber mask (Figure 12–8). The LMA is inserted blindly into the hypopharynx and is seated over the larynx, occluding the esophagus. Advantages to its use include ease of insertion, lower potential for airway trauma, and higher success rates. Patients remain at higher risk for aspiration with LMA use compared with orotracheal intubation; therefore, the LMA should not be used for prolonged, definitive airway management. Rarely, if tracheal intubation cannot be accomplished, particularly in the setting of massive facial trauma, cricothyroidotomy may be necessary. Needle cricothyroidotomy using a large-bore catheter through the cricothyroid membrane is the procedure of choice in patients younger than 12 years. Operative revision to a tracheostomy is necessary.
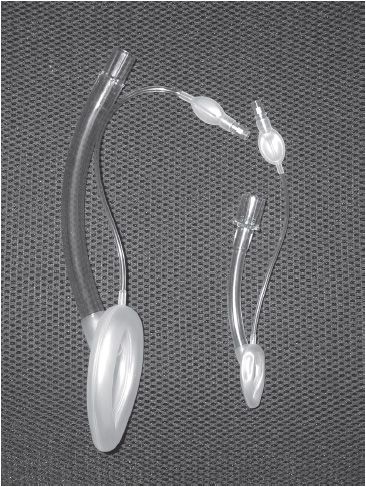
 Figure 12–8. Laryngeal mask airways of various sizes.
Figure 12–8. Laryngeal mask airways of various sizes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree