Background
Menopause is associated with increased risk of cardiovascular disease and the causal factors have been proposed to be the loss of estrogen and the subsequent alterations of the hormonal milieu. However, which factors contribute to the deterioration of cardiometabolic health in postmenopausal women is debated as the menopausal transition is also associated with increased age and fat mass. Furthermore, indications of reduced cardiometabolic adaptations to exercise in postmenopausal women add to the adverse health profile.
Objective
We sought to evaluate risk factors for type 2 diabetes and cardiovascular disease in late premenopausal and early postmenopausal women, matched by age and body composition, and investigate the effect of high-intensity training.
Study Design
A 3-month high-intensity aerobic training intervention, involving healthy, nonobese, late premenopausal (n = 40) and early postmenopausal (n = 39) women was conducted and anthropometrics, body composition, blood pressure, lipid profile, glucose tolerance, and maximal oxygen consumption were determined at baseline and after the intervention.
Results
At baseline, the groups matched in anthropometrics and body composition, and only differed by 4.2 years in age (mean [95% confidence limits] 49.2 [48.5-49.9] vs 53.4 [52.4-54.4] years). Time since last menstrual period for the postmenopausal women was (mean [95% confidence limits] 3.1 [2.6-3.7] years). Hormonal levels (estrogen, follicle stimulation hormone, luteinizing hormone) confirmed menopausal status. At baseline the postmenopausal women had higher total cholesterol ( P < .001), low-density lipoprotein-cholesterol ( P < .05), and high-density lipoprotein-cholesterol ( P < .001) than the premenopausal women. The training intervention reduced body weight ( P < .01), waist circumference ( P < .01), and improved body composition by increasing lean body mass ( P < .001) and decreasing fat mass ( P < .001) similarly in both groups. Moreover, training resulted in lower diastolic blood pressure ( P < .05), resting heart rate ( P < .001), total cholesterol ( P < .01), low-density lipoprotein-cholesterol ( P < .01), total cholesterol/high-density lipoprotein-cholesterol index ( P < .01), and improved plasma insulin concentration during the oral glucose tolerance test ( P < .05) in both groups.
Conclusion
Cardiovascular risk factors are similar in late premenopausal and early postmenopausal women, matched by age and body composition, with the exception that postmenopausal women have higher high- and low-density lipoprotein-cholesterol levels. A 3-month intervention of high-intensity aerobic training reduces risk factors for type 2 diabetes and cardiovascular disease to a similar extent in late premenopausal and early postmenopausal women.
Introduction
The menopausal transition is accompanied by metabolic changes and increasing prevalence of metabolic syndrome (MetS), which is defined as copresence of abdominal obesity, hypertension, dyslipidemia, and insulin resistance. MetS is associated with development of type 2 diabetes (T2D) (relative risk [RR] 5.0), cardiovascular disease (CVD) (RR 2.35), and all-cause mortality (RR 1.86), and globally it is estimated that 30-55% of postmenopausal women fulfill the diagnostic criteria for MetS. It is debated whether the increased prevalence of MetS after menopause is due to hormonal changes, a normal phenomenon of aging, or a consequence of gain in weight and fat-mass during and after the menopausal transition. It is therefore highly relevant to evaluate factors associated with MetS in nonobese premenopausal and postmenopausal women matched by age and body composition.
Physical exercise increases cardiorespiratory fitness and reduces the risk of MetS but the ability of postmenopausal women to respond to exercise training has been debated. Some cross-sectional studies suggest that postmenopausal women have a reduced fitness level compared to premenopausal women and a blunted response to exercise-induced central and peripheral cardiovascular modulations. Another study finds similar beneficial effects of brisk walking on body composition and glucose metabolism, irrespective of menopausal status, in overweight to obese women and a review, investigating the effects of exercise training in early postmenopausal women, found increases in ˙V
V ˙
o 2max (ranging from 4-32%), diverse effects of exercise on blood pressure (BP) in normotensive women but a lowering effect in hypertensive women, as well as reductions in plasma lipids in dyslipidemic but not in normolipidemic women. However, very few studies have compared the effect of physical activity on the risk of MetS in premenopausal vs postmenopausal women. The aim of this study was therefore to investigate the effect of a well-controlled high-intensity aerobic training program on risk factors predisposing to T2D and CVD in nonobese, early postmenopausal women and to compare the effect of the training intervention to the effect in late premenopausal women differing, on average, only by 4 years of age.
Materials and Methods
Overall study design
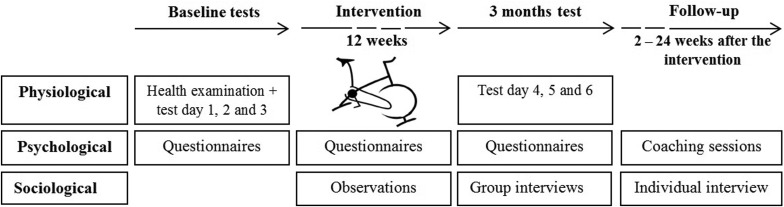
The work was carried out as part of the research program Copenhagen Women Study (cws.ku.dk) funded by the University of Copenhagen Excellence Program for Interdisciplinary Research. This article presents data from work package II where late premenopausal and early postmenopausal women were assigned to 3 months of high-intensity aerobic training, performed as spinning. All participants underwent a health examination before inclusion as well as examinations at baseline and after 3 months, comprising physiological, psychological, and sociological tests ( Figure 1 ). All women participated in the general tests on day 1 and 2 at baseline and test day 4 and 5 after 3 months. At test day 3 (baseline) and 6 (3 months) specific investigations of either cardiovascular function (n = 42 women) or adipose tissue and skeletal muscle metabolic function (n = 41 women) were conducted. This article covers the results of the general physiological tests, and all presented outcomes were a priori defined as secondary outcomes in clinicaltrials.gov , registration number: NCT02135575 .
Recruitment
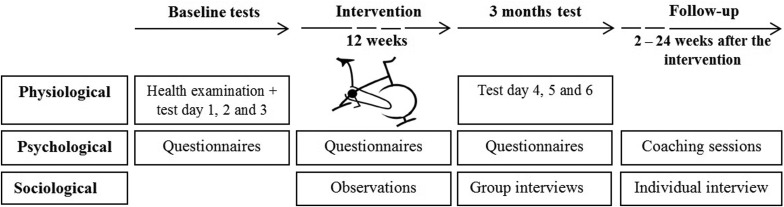
Late premenopausal (n = 43) and early postmenopausal (n = 40) women were recruited from the Copenhagen area through newspaper advertisements. Eligibility was assessed upon first contact by telephone or mail, secondly by evaluation of an online questionnaire, and finally at a health examination ( Figure 2 ). Recruitment was conducted through 4 rounds from August 2013 through August 2015, and an almost equal number of premenopausal and postmenopausal women were recruited in each round to prevent seasonal and investigator-dependent variations. All participants received written and oral information about the study, including risks and discomforts associated with participation, before they gave their written consent to participate. The study was conducted according to the Helsinki Declaration and approved by the ethical committee in the capital region of Denmark, protocol no. H-1-2012-150.
Participants
Inclusion criteria were healthy, sedentary, normal-weight to overweight (body mass index [BMI] 18.5-30 kg/m 2 ) women, 45-57 years of age, who were either late premenopausal (regular bleeding and plasma estradiol [E 2 ] in the normal fertile range; follicular phase 0.05-0.51 nmol/L, mid cycle 0.32-1.83 nmol/L, luteal phase 0.16-0.78 nmol/L, and plasma follicle-stimulating hormone [FSH] <20 IU/L) or early postmenopausal (no bleeding for at least 1 year, E 2 <0.20 nmol/L and FSH 22-138 IU/L). Being sedentary was defined as performing <2 hours of physical activity per week during the last 2 years, and the definition was also supported by a V ˙ o 2max <40 mL O 2 /min/kg. Exclusion criteria were smoking, use of hormonal contraception, excessive alcohol intake, diagnosis of hypertension or any other chronic disease, daily intake of medication, or blood samples (screening for liver, kidney, and bone-marrow function) outside of normal range. Characteristics of the participants are presented in Table 1 .
| Variables | Premenopausal | Postmenopausal | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | n | 3 months | n | Baseline | n | 3 mo | n | |
| Anthropometrics | ||||||||
| Age, y a | 49.2 (48.5–49.9) | 39 | – | 53.4 (52.4–54.4) | 38 | – | ||
| Height, m | 1.68 (1.66–1.70) | 38 | – | 1.67 (1.65–1.69) | 37 | – | ||
| Weight, kg b | 67.7 (65.5–70.0) | 38 | 67.1 (64.9–69.3) | 38 | 66.4 (63.6–69.1) | 38 | 65.8 (62.9–68.7) | 37 |
| BMI, kg/m 2 b | 23.9 (23.2–24.7) | 38 | 23.7 (23.0–24.4) | 38 | 23.7 (22.9–24.4) | 37 | 23.5 (22.6–24.3) | 37 |
| Waist circumference, cm b | 80 (78–82) | 32 | 79 (77–81) | 32 | 79 (76–81) | 32 | 78 (76–81) | 31 |
| Body composition | ||||||||
| Lean body mass, kg b | 43.5 (42.0–44.9) | 38 | 44.1 (42.7–45.5) | 38 | 42.7 (41.3–44.1) | 38 | 43.2 (41.7–44.7) | 37 |
| Fat mass, kg b | 24.3 (22.8–25.7) | 38 | 23.0 (21.5–24.5) | 38 | 23.6 (21.8–25.5) | 38 | 22.6 (20.6–24.6) | 37 |
| Fat, % b | 35.7 (34.2–37.1) | 38 | 34.1 (32.7–35.6) | 38 | 35.3 (33.7–36.9) | 38 | 33.9 (32.1–35.7) | 37 |
| Android fat, % b | 38.4 (35.8–41.0) | 38 | 36.4 (33.7–39.0) | 38 | 35.9 (32.8–39.1) | 38 | 34.3 (30.9–37.6) | 37 |
| Gynoid fat, % b | 41.5 (40.0–43.0) | 38 | 39.4 (38.0–40.9) | 38 | 41.9 (40.5–43.2) | 38 | 39.7 (38.1–41.4) | 37 |
| Android-gynoid fat ratio | 0.92 (0.87–0.98) | 38 | 0.92 (0.86–0.98) | 38 | 0.85 (0.79–0.91) | 38 | 0.85 (0.79–0.92) | 37 |
| Hormones | ||||||||
| P-estradiol, nmol/L | 0.61 (0.28–1.13) | 39 | 0.54 (0.37–0.98) | 32 | 0.04 (0.04–0.32) | 38 | 0.04 (0.04–0.09) | 32 |
| P-follitropin [FSH], IU/L a , b , c | 8.5 (5.3–16.3) | 39 | 8.3 (5.4–13.8) | 32 | 90.0 (74.2–112.0) | 38 | 79.8 (65.5–103.0) | 32 |
| P-lutropin [LH], IU/L a , c | 11.4 (8.6–15.2) | 39 | 11.0 (8.0–15.1) | 32 | 38.3 (35.0–41.9) | 38 | 33.8 (30.1–38.1) | 32 |
| Blood pressure | ||||||||
| Systolic, mm Hg d | 107 (99–117) | 39 | 108 (103–118) | 38 | 111 (103–120) | 38 | 107 (99–120) | 37 |
| Diastolic, mm Hg b | 70 (66–75) | 39 | 70 (66–76) | 38 | 71 (66–79) | 38 | 70 (65–75) | 37 |
| Mean arterial pressure, mm Hg d | 82 (76–88) | 39 | 82 (78–90) | 38 | 84 (79–92) | 38 | 82 (77–88) | 37 |
| Resting heart rate, beats/min –1 b | 66 (61–72) | 38 | 65 (58–71) | 38 | 64 (59–68) | 38 | 61 (56–66) | 37 |
| Maximal heart rate, beats/min –1 b | 176 (172–180) | 35 | 175 (172–177) | 38 | 175 (171–180) | 36 | 173 (169–176) | 34 |
a Statistically significant ( P ≤ .05) difference between premenopausal and postmenopausal group. Effort of intervention was assessed by 2-way analysis of variance
b Statistically significant ( P ≤ .05) difference from baseline to 3 mo
c Statistically significant ( P ≤ .05) difference between premenopausal and postmenopausal group
d Statistically significant ( P ≤ .05) interaction between time and menopausal status, meaning that 2 groups responded differently to intervention.
Exercise training intervention
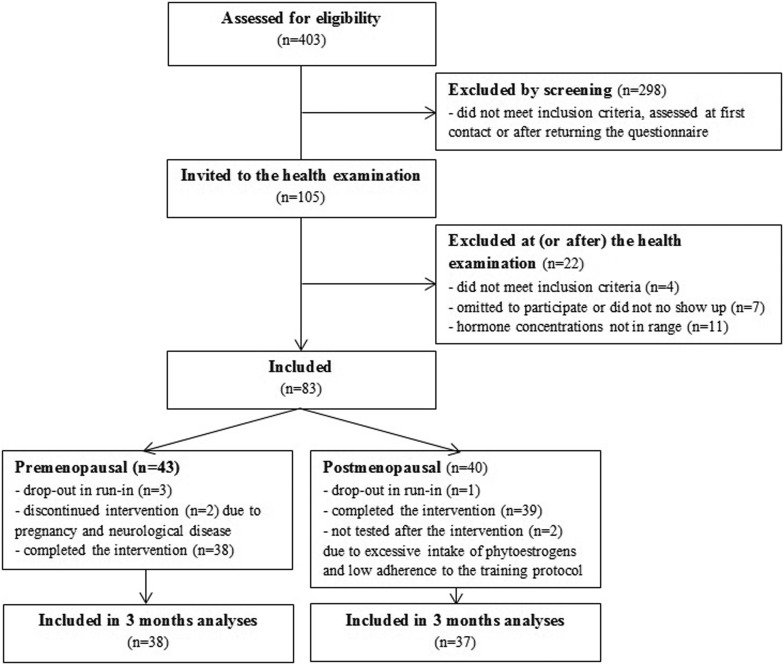
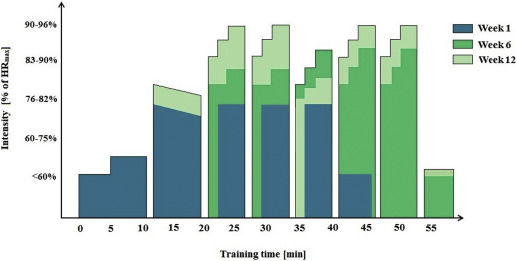
The intervention consisted of 3 months of high-intensity aerobic training (spinning), conducted 3 times/wk for approximately 1 hour. Two weekly sessions were conducted in our exercise training facility by instructors from our research group and in the beginning of every round, a medical doctor attended the spinning classes. The sessions comprised a warm-up, 3 blocks of varying intervals, with multiple periods of maximum performance, followed by a cool-down period ( Figure 3 ). The intensity of the training sessions increased gradually during the 3-month period. During the sessions, the instructor and the participants were able to monitor their own and their peers’ heart rate (HR) on a big screen, given as a percentage of their individual maximal HR (HR max ). One weekly session took place in a local fitness center. During all training sessions the participants wore HR monitors (FT2; Polar, Kempele, Finland).
Measurements and analyses
Anthropometrics were assessed using a tape measure for hip and waist circumference and a stadiometer for height. Body composition was assessed by dual x-ray absorptiometry scanning (Lunar iDXA; GE Healthcare, Little Chalfont, United Kingdom) at Department of Clinical Physiology, Nuclear Medicine, and Positron Emission Tomography, Rigshospitalet, Glostrup, Denmark, by an investigator blinded for menopausal status. All scans were performed by the same investigator at baseline and after 3 months. Blood samples were obtained from the antecubital vein by a BD Vacutainer system (Becton-Dickinson, Plymouth, United Kingdom) and analyzed at Department of Clinical Biochemistry, Rigshospitalet, Copenhagen, Denmark, by investigators blinded for menopausal status. Plasma E 2 was analyzed by competitive electrochemiluminescence immunoassay (ECLIA), and FSH and luteinizing hormone were analyzed by sandwich ECLIA (Cobas 8000, e602 module; F. Hoffmann-La Roche Ltd, Rotkreuz, Switzerland). Plasma high-density lipoprotein (HDL)-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), total cholesterol, and triglyceride were measured by enzymatic absorption photometry (Cobas 8000, c702 module; F. Hoffmann-La Roche Ltd). Screening samples, used for evaluation of liver, kidney, and bone-marrow function, were analyzed by standard methods at Department of Clinical Biochemistry, Rigshospitalet, Copenhagen, Denmark.
Oral glucose tolerance test
The participants arrived at the laboratory after an overnight fast and an intravenous catheter (Vasofix Safety, 20G; B. Braun Melsungen AG, Melsungen, Germany) was placed in an antecubital vein. Blood was obtained from the catheter, put into EDTA-precoated tubes, and immediately centrifuged (Ole Dich Instrumentmakers ApS, Hvidovre, Denmark) at 4000 rpm for 2 minutes, and plasma was stored at –80°C until analysis. After oral intake of 82.5 g monohydrate glucose dissolved in 250 mL of water, blood samples were collected at 15, 30, 45, 60, 90, and 120 minutes and handled as described above. Glucose was assessed by photometric measurement (Cobas 8000, c702 module), and insulin and C-peptide were determined by sandwich ECLIA (Cobas 8000, e602 module).
Calculations
The Matsuda index was calculated as a surrogate measure of insulin sensitivity during the oral glucose tolerance test (OGTT) using the formula :
BP was measured using an upper arm, automatic BP monitor (M2 HEM-7121-E; Omron, Hoofddorp, The Netherlands) with the participant in a supine position, after at least 15 minutes of rest. The reported values are means of 7 consecutive measurements.
VO 2 -max
Maximal oxygen consumption was assessed during an incremental bicycle ergometer protocol (839E; Monark Exercise AB, Vansbro, Sweden) using an automated online system, measuring breath-by-breath pulmonary oxygen uptake and carbon-dioxide production (Oxycon Pro, Intramedic, Gentofte, Denmark). Before the test, the bicycle ergometer and the Oxycon Pro were calibrated and the saddle and handlebars were adjusted to fit the participant. HR monitor (Team2 Transmitter, Polar) was placed, and the mask was fitted. The participant was informed about the test, told to remain seated during the entire test, and to keep a pace of 60-70 rpm. Before the test was started, there was an 8-minute warm-up period with a workload of 50 W. The test workload started at 50 W and was increased by 25 W every minute, until exhaustion. The test was approved if 2 of 3 criteria were fulfilled: plateau in V ˙ o 2 despite an increasing workload, respiratory exchange ratio >1.1, and HR >90% of predicted value, calculated as 220 minus age in years. The maximal watt load was registered at the end of the test.
Statistical methods
Statistical calculations were performed using software (SAS Enterprise Guide 7.1; SAS Institute Inc, Cary, NC). Descriptive statistics for parametric data are given as means (95% confidence limits) and for nonparametric data as median (25th-75th percentile). Baseline comparisons were made using independent t tests. The effects of menopausal status and exercise training were assessed using a 2-way repeated measures analysis of variance. Alpha was set to 0.05.
Materials and Methods
Overall study design
The work was carried out as part of the research program Copenhagen Women Study (cws.ku.dk) funded by the University of Copenhagen Excellence Program for Interdisciplinary Research. This article presents data from work package II where late premenopausal and early postmenopausal women were assigned to 3 months of high-intensity aerobic training, performed as spinning. All participants underwent a health examination before inclusion as well as examinations at baseline and after 3 months, comprising physiological, psychological, and sociological tests ( Figure 1 ). All women participated in the general tests on day 1 and 2 at baseline and test day 4 and 5 after 3 months. At test day 3 (baseline) and 6 (3 months) specific investigations of either cardiovascular function (n = 42 women) or adipose tissue and skeletal muscle metabolic function (n = 41 women) were conducted. This article covers the results of the general physiological tests, and all presented outcomes were a priori defined as secondary outcomes in clinicaltrials.gov , registration number: NCT02135575 .