Background
Spontaneous abortion is the most commonly observed adverse pregnancy outcome. The angiogenic factors soluble Fms-like kinase 1 and placental growth factor are critical for normal pregnancy and may be associated to spontaneous abortion.
Objective
We investigated the association between maternal serum concentrations of soluble Fms-like kinase 1 and placental growth factor, and subsequent spontaneous abortion.
Study Design
In the prospective observational Odense Child Cohort, 1676 pregnant women donated serum in early pregnancy, gestational week <22 (median 83 days of gestation, interquartile range 71-103). Concentrations of soluble Fms-like kinase 1 and placental growth factor were determined with novel automated assays. Spontaneous abortion was defined as complete or incomplete spontaneous abortion, missed abortion, or blighted ovum <22+0 gestational weeks, and the prevalence was 3.52% (59 cases). The time-dependent effect of maternal serum concentrations of soluble Fms-like kinase 1 and placental growth factor on subsequent late first-trimester or second-trimester spontaneous abortion (n = 59) was evaluated using a Cox proportional hazards regression model, adjusting for body mass index, parity, season of blood sampling, and age. Furthermore, receiver operating characteristics were employed to identify predictive values and optimal cut-off values.
Results
In the adjusted Cox regression analysis, increasing continuous concentrations of both soluble Fms-like kinase 1 and placental growth factor were significantly associated with a decreased hazard ratio for spontaneous abortion: soluble Fms-like kinase 1, 0.996 (95% confidence interval, 0.995–0.997), and placental growth factor, 0.89 (95% confidence interval, 0.86–0.93). When analyzed by receiver operating characteristic cut-offs, women with soluble Fms-like kinase 1 <742 pg/mL had an odds ratio for spontaneous abortion of 12.1 (95% confidence interval, 6.64–22.2), positive predictive value of 11.70%, negative predictive value of 98.90%, positive likelihood ratio of 3.64 (3.07-4.32), and negative likelihood ratio of 0.30 (0.19-0.48). For placental growth factor <19.7 pg/mL, odds ratio was 13.2 (7.09-24.4), positive predictive value was 11.80%, negative predictive value was 99.0%, positive likelihood ratio was 3.68 (3.12-4.34), and negative likelihood ratio was 0.28 (0.17-0.45). In the sensitivity analysis of 54 spontaneous abortions matched 1:4 to controls on gestational age at blood sampling, the highest area under the curve was seen for soluble Fms-like kinase 1 in prediction of first-trimester spontaneous abortion, 0.898 (0.834-0.962), and at the optimum cut-off of 725 pg/mL, negative predictive value was 51.4%, positive predictive value was 94.6%, positive likelihood ratio was 4.04 (2.57-6.35), and negative likelihood ratio was 0.22 (0.09-0.54).
Conclusion
A strong, novel prospective association was identified between lower concentrations of soluble Fms-like kinase 1 and placental growth factor measured in early pregnancy and spontaneous abortion. A soluble Fms-like kinase 1 cut-off <742 pg/mL in maternal serum was optimal to stratify women at high vs low risk of spontaneous abortion. The cause and effect of angiogenic factor alterations in spontaneous abortions remain to be elucidated.
Introduction
Spontaneous abortion is the most common adverse outcome of pregnancy. Up to 60% of fertilized ova will be aborted in a preclinical stage, and of the 40% of remaining embryos/fetuses, 1 in 4 will miscarry. The etiology of spontaneous abortion is multifactorial, and predisposing factors include genetic, anatomical, endocrine, immunological, microbiological, and environmental parameters.
Spontaneous abortions can be identified by vaginal ultrasound examination, supplemented by measurements of human chorionic gonadotropin (hCG) concentration, which decreases rapidly in case of a spontaneous abortion. Low hCG concentrations in early pregnancy have been associated with spontaneous abortion and other adverse pregnancy outcomes and recent research suggested that serum progesterone concentrations could identify women with spontaneous abortion at the time of symptoms. Although both ultrasound and serial hCG values can, to some extent, identify women at risk of spontaneous abortion, research remains sparse on other biomarkers to prospectively identify at-risk pregnancies, before the onset of clinical symptoms.
The placenta plays a key role for implantation and tolerance of the fetus. Soluble Fms-like kinase (sFlt)-1 and placental growth factor (PlGF) are both involved in placental development and vascularization. The sFlt-1 is a scavenger receptor for vascular endothelial growth factor (VEGF)-A and PlGF, and acts as a negative, paracrine regulator of vasculogenesis in the placenta, contributing to correct morphology of the developing blood vessels. Membrane-bound Fms-like kinase (Flt)-1 and sFlt-1 is abundantly expressed in the developing placenta and fetus. Flt-1 knock-out mouse embryos die in utero, with endothelial cells assembled into abnormal vascular channels, suggesting that Flt-1 plays a key role in regulating cell-cell or cell-matrix interactions. Deletion of the membrane-spanning tyrosine kinase part of the Flt-1 receptor in mice resulted in live litters with an almost normal phenotype, suggesting that the soluble variant of Flt-1 is the most important for regulation of placental and fetal development. Moreover, up-regulation of sFlt-1 in early pregnancy has been associated with increased fetal weight in both mouse and human studies. PlGF concentrations in the first half of pregnancy are low compared to VEGF-A but increase toward term. PlGF and VEGF take part in a complex interplay and the activation of the Flt-1 and fetal liver kinase receptors, where PlGF potentiates the angiogenic effect of VEGF-A. Yet, PlGF-null mice are born with near-normal phenotypes, suggesting that PlGF is not essential for successful implantation and embryonic development. Lower PlGF concentrations in pregnancy are associated with development of subsequent preeclampsia.
Since angiogenic factors are critical for normal pregnancy and may be markers of successful intrauterine pregnancies, we investigated the association between sFlt-1 and PlGF concentrations, and the prospective occurrence of spontaneous abortion (until 22 weeks of gestation) in a large, population-based cohort.
Materials and Methods
Study population and participants
Briefly, Odense Child Cohort is a population-based cohort that included newly pregnant women from Jan. 1, 2010, through Dec. 31, 2012. All participants gave informed consent in writing.
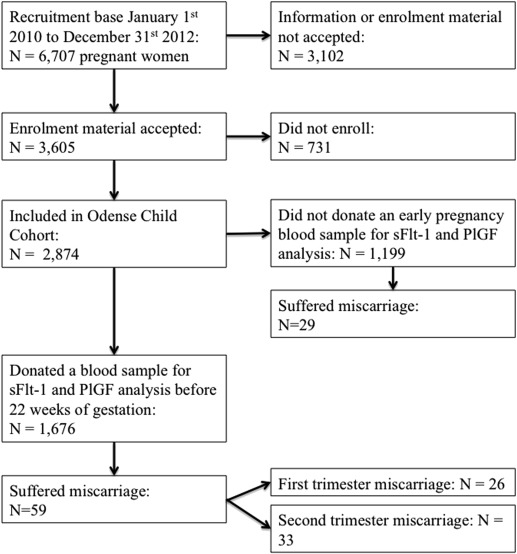
From a population base of 7032 pregnant women, 6707 were offered inclusion and a total of 2874 (42.9%) pregnant women enrolled in Odense Child Cohort up to Dec. 31, 2012 ( Figure 1 ). Of the participants, 1684 (58.6%) donated a blood sample in early pregnancy. Early pregnancy was defined as first trimester and early second trimester (until 22+0 completed weeks of gestation), as this constitutes the formal limit between defining a fetal loss as a spontaneous abortion and a stillbirth. A total of 1675 blood samples were available for analysis of sFlt-1 and PlGF. Spontaneous abortion was defined either as a missed abortion, a complete or incomplete spontaneous abortion, or a blighted ovum <22 completed weeks. The timing of spontaneous abortion was defined as the date of diagnosis by transvaginal ultrasound. At the time of blood sampling, most women in the cohort had not yet undergone first-trimester ultrasound examination, and thus, information was not available regarding the status of the embryo/fetus at time of blood sampling.
The date of the last menstrual period, pregestational body mass index (BMI), maternal age at the time of delivery, smoking habits, and parity were extracted from self-reported data at the first antenatal visit. Gestational age was calculated from first-trimester ultrasound data or from date of last menstrual period if ultrasound data were not available.
Description of assay methods
Measurements for Brahms sFlt-1 and PlGF KRYPTOR assays were performed on the fully automated KRYPTOR compact plus system (Thermo Scientific B·R·A·H·M·S Biomarkers, Thermo Fisher Scientific, Hennigsdorf, Germany) according to the manufacturer’s instructions as described in detail previously. The KRYPTOR sFlt-1 assay covered a measuring range of 22-90,000 pg/mL. The limit of detection is 22 pg/mL and the limit of quantization (functional sensitivity) is 29 pg/mL. The KRYPTOR PlGF assay covers a measuring range of 3.6-7.000 pg/mL. The limit of detection is 3.6 pg/mL and the limit of quantitation is 6.9 pg/mL. The intraassay and interassay variations at sFlt-1 concentration of 1540 pg/mL are 0.3% and 0.8%, respectively; at 2988 pg/mL, 0.5% and 1.1%, respectively; and at 9666 pg/mL, 0.5% and 1.0%, respectively. The intraassay and interassay variations at a PlGF concentration of 35 pg/mL are 4.6% and 7.3%, respectively; at 103 pg/mL, 2.1% and 3.1%, respectively; and at 430 pg/mL, 0.9% and 2.3%, respectively.
Statistical analyses
Variables were reported as mean ± SD or as median and interquartile range (IQR) as appropriate according to data distribution. Crude comparisons of angiogenic marker concentrations and maternal characteristics between spontaneous and nonspontaneous abortion groups were done with Student t test or Mann-Whitney test as appropriate. Correlation between concentrations of angiogenic markers and time from blood sampling until diagnosed spontaneous abortion was tested using linear regression.
A Cox proportional hazards regression model was constructed to analyze the time-dependent effect of continuous sFlt-1 and PlGF concentrations relative to risk of spontaneous abortion, with submodels specific for first-trimester spontaneous abortion and second trimester. All participants were censored at 22+0 weeks of gestation. Correlations between spontaneous abortion and sFlt-1 and PlGF were performed for the continuous variables, and the population median values overall and in first/second trimester, respectively. Adjusted analyses included maternal BMI, parity, and age as covariates.
Receiver operating characteristic (ROC) curves were employed for analysis of the predictive value of the biomarkers in spontaneous abortion. Tabulations of ROC results were employed for determinations of area under the curve (AUC), and predictive values were calculated at selected cut-off values with determination of diagnostic odds ratio (OR), specificity, sensitivity, positive predictive value (PPV), and negative predictive value (NPV) for spontaneous abortion. Since the investigated biomarkers change in concentrations with gestational age, we performed a sensitivity analysis between 54 spontaneous abortions and 216 normal pregnancies matched 1:4 on gestational age at blood sampling.
Software (STATA 12.0; StataCorp, College Station, TX) was used for all data analysis. Significance level was set at P < .05 using 2-sided tests.
Ethical approval
The study complied with the Helsinki Declaration and was approved by the Regional Scientific Ethical Committee for Southern Denmark, no. S-20150158.
Materials and Methods
Study population and participants
Briefly, Odense Child Cohort is a population-based cohort that included newly pregnant women from Jan. 1, 2010, through Dec. 31, 2012. All participants gave informed consent in writing.
From a population base of 7032 pregnant women, 6707 were offered inclusion and a total of 2874 (42.9%) pregnant women enrolled in Odense Child Cohort up to Dec. 31, 2012 ( Figure 1 ). Of the participants, 1684 (58.6%) donated a blood sample in early pregnancy. Early pregnancy was defined as first trimester and early second trimester (until 22+0 completed weeks of gestation), as this constitutes the formal limit between defining a fetal loss as a spontaneous abortion and a stillbirth. A total of 1675 blood samples were available for analysis of sFlt-1 and PlGF. Spontaneous abortion was defined either as a missed abortion, a complete or incomplete spontaneous abortion, or a blighted ovum <22 completed weeks. The timing of spontaneous abortion was defined as the date of diagnosis by transvaginal ultrasound. At the time of blood sampling, most women in the cohort had not yet undergone first-trimester ultrasound examination, and thus, information was not available regarding the status of the embryo/fetus at time of blood sampling.
The date of the last menstrual period, pregestational body mass index (BMI), maternal age at the time of delivery, smoking habits, and parity were extracted from self-reported data at the first antenatal visit. Gestational age was calculated from first-trimester ultrasound data or from date of last menstrual period if ultrasound data were not available.
Description of assay methods
Measurements for Brahms sFlt-1 and PlGF KRYPTOR assays were performed on the fully automated KRYPTOR compact plus system (Thermo Scientific B·R·A·H·M·S Biomarkers, Thermo Fisher Scientific, Hennigsdorf, Germany) according to the manufacturer’s instructions as described in detail previously. The KRYPTOR sFlt-1 assay covered a measuring range of 22-90,000 pg/mL. The limit of detection is 22 pg/mL and the limit of quantization (functional sensitivity) is 29 pg/mL. The KRYPTOR PlGF assay covers a measuring range of 3.6-7.000 pg/mL. The limit of detection is 3.6 pg/mL and the limit of quantitation is 6.9 pg/mL. The intraassay and interassay variations at sFlt-1 concentration of 1540 pg/mL are 0.3% and 0.8%, respectively; at 2988 pg/mL, 0.5% and 1.1%, respectively; and at 9666 pg/mL, 0.5% and 1.0%, respectively. The intraassay and interassay variations at a PlGF concentration of 35 pg/mL are 4.6% and 7.3%, respectively; at 103 pg/mL, 2.1% and 3.1%, respectively; and at 430 pg/mL, 0.9% and 2.3%, respectively.
Statistical analyses
Variables were reported as mean ± SD or as median and interquartile range (IQR) as appropriate according to data distribution. Crude comparisons of angiogenic marker concentrations and maternal characteristics between spontaneous and nonspontaneous abortion groups were done with Student t test or Mann-Whitney test as appropriate. Correlation between concentrations of angiogenic markers and time from blood sampling until diagnosed spontaneous abortion was tested using linear regression.
A Cox proportional hazards regression model was constructed to analyze the time-dependent effect of continuous sFlt-1 and PlGF concentrations relative to risk of spontaneous abortion, with submodels specific for first-trimester spontaneous abortion and second trimester. All participants were censored at 22+0 weeks of gestation. Correlations between spontaneous abortion and sFlt-1 and PlGF were performed for the continuous variables, and the population median values overall and in first/second trimester, respectively. Adjusted analyses included maternal BMI, parity, and age as covariates.
Receiver operating characteristic (ROC) curves were employed for analysis of the predictive value of the biomarkers in spontaneous abortion. Tabulations of ROC results were employed for determinations of area under the curve (AUC), and predictive values were calculated at selected cut-off values with determination of diagnostic odds ratio (OR), specificity, sensitivity, positive predictive value (PPV), and negative predictive value (NPV) for spontaneous abortion. Since the investigated biomarkers change in concentrations with gestational age, we performed a sensitivity analysis between 54 spontaneous abortions and 216 normal pregnancies matched 1:4 on gestational age at blood sampling.
Software (STATA 12.0; StataCorp, College Station, TX) was used for all data analysis. Significance level was set at P < .05 using 2-sided tests.
Ethical approval
The study complied with the Helsinki Declaration and was approved by the Regional Scientific Ethical Committee for Southern Denmark, no. S-20150158.
Results
Among the 2874 participating women, 88 (3.1%) had a spontaneous abortion. Of the 1676 women who donated a blood sample at gestation <22+0 weeks for sFlt-1 and PlGF analysis, 59 (3.5%) women had spontaneous abortions. In all, 26 occurred in first trimester and 33 in second trimester ( Figure 1 ). Of the 1190 participants who did not donate a blood sample at gestation <22+0 weeks, 29 (2.8%) had a spontaneous abortion.
The spontaneous abortion group had lower concentrations of sFlt-1 (median 528.0 [IQR 477.8] vs 1043.3 [IQR 596.0] pg/mL, P < .0001) and lower concentrations of PlGF (median 14.9 [IQR 8.8] vs 31.8 [IQR 35.1] pg/mL, P < .0001) compared to women who did not miscarry, with blood samples taken earlier (gestational age 69 vs 84 days, P < .0001) ( Table 1 ). The spontaneous abortion group did not differ from the background population with respect to maternal age, BMI, or parity. Women having spontaneous abortions within the first trimester of pregnancy had a trend toward lower concentrations of sFlt-1 (median 421.3 [IQR 407.6] vs 611.6 [IQR 549.7] pg/mL, P = .09), a trend toward lower PlGF (median 611.6 [IQR 549.7] vs 15.8 [IQR 9.1] pg/mL, P = .06), and earlier blood sampling compared to those having spontaneous abortions in the second trimester ( Table 1 ). Median time between blood sampling and spontaneous abortion diagnosis was 13 (IQR 9-20) days.
| No spontaneous abortion | Spontaneous abortion | P value | First-trimester spontaneous abortion | Second-trimester spontaneous abortion | P value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | 1617 | 59 | 26 | 33 | ||||||
| sFlt-1, pg/mL, median (IQR) | 1043.3 | (596) | 528 | (477.8) | <.0001 | 421.3 | (407.6) | 611.6 | (549.7) | .09 |
| PlGF, pg/mL, median (IQR) | 31.8 | (35.1) | 14.9 | (8.8) | <.0001 | 13.5 | (5.7) | 15.8 | (9.1) | .06 |
| GA blood sampling, d, median (IQR) | 84 | (32) | 69 | (12.5) | <.0001 | 65 | (7) | 74 | (9) | .001 |
| GA at time of spontaneous abortion, d, median (IQR) | – | – | 85.5 | (14) | – | 76 | (12) | 89.5 | (7) | <.0001 |
| Maternal age, y, mean (SD) | 30.2 | (4.5) | 30.6 | (5.8) | NS | 30.7 | (5.9) | 30.5 | (5.7) | NS |
| Maternal prepregnancy BMI, mean (SD) | 24.3 | (4.4) | 24.2 | (4.1) | NS | 24.1 | (3.7) | 24.3 | (4.4) | NS |
| Smoking in pregnancy, n (%) | 83 | (5.1) | 1 | (1.7) | NS | 1 | (3.8) | 0 | (0) | NS |
| Nullipara, n (%) | 915 | (56.6) | 30 | (50.8) | NS | 14 | (53.8) | 16 | (48.5) | NS |
PlGF concentrations were correlated to the number of days between blood sampling and subsequent spontaneous abortion, adjusted for gestational age at blood sampling (β = 0.26, P = .01), however sFlt-1 concentrations were not (β = 1.44, P = .3). Subanalyses demonstrated that concentrations of PlGF and sFlt-1 did not differ significantly between women who had complete or incomplete spontaneous abortions, respective to women with missed abortions. Furthermore, concentrations of the biomarkers were not significantly different between women with spontaneous abortion overall, and women with stillbirth >22 weeks’ gestation (n = 6) (data not shown).
Time-dependent effects
PlGF increased continuously with gestational age ( Figure 1 ). The median PlGF value was >10-fold lower in gestational week 8 (14.9 [IQR 12.6-19.3] pg/mL) relative to gestational week 21 (168.9 [IQR 134.4-292.0] pg/mL). The sFlt-1 also increased with gestational age until the end of first trimester. At gestational week 12, mean sFlt-1 was 1064.9 (IQR 814.2-1373.9) pg/mL compared with 1276.7 (IQR 956.1-1708.0) pg/mL in gestational week 21 ( Figure 2 ). In the Cox proportional hazards regression model adjusted for maternal covariates, both sFlt-1 and PlGF were significantly associated with a decreased hazard ratio for spontaneous abortion: sFlt-1, 0.996 (95% confidence interval [CI], 0.995–0.997), and PlGF, 0.89 (95% CI, 0.86–0.93) ( Supplemental Table 1 ).




