Background
Cervical length at midtrimester is a powerful predictor of preterm birth in twin gestations. However, given the fact that, in some cases, cervical shortening may become evident only later during the second trimester, it seems reasonable that serial monitoring of cervical length may improve the detection of preterm birth in women with twins. However, data in support of such a practice are limited and conflicting. The contradictory results may be related to the fact that in most of these studies, the analysis of the predictive value of serial measurements of cervical length was limited to data derived from only two sequential measurements of cervical length, while data on the predictive value of multiple (>2) measurements are scarce.
Objective
We sought to determine whether serial measurements of cervical length can improve the prediction of preterm birth in asymptomatic women with twin gestations compared with a single measurement of cervical length at midgestation.
Study Design
This was a retrospective cohort study of women with twin pregnancies followed up in a tertiary medical center from 2012 through 2014. All participants underwent routine measurement of cervical length at midgestation and every 2-3 weeks thereafter until 28-32 weeks. For each patient, cervical length was determined at the following time periods: 18+0 to 21+6 weeks (period 1, routine exam), 22+0 to 24+6 weeks (period 2), 25+0 to 27+6 weeks (period 3), and 28+0 to 32+0 weeks (period 4). Measurements of cervical length at periods 2-4 were analyzed in the form of either absolute length (in millimeters) or percent shortening relative to cervical length at period 1. The performance of a stepwise algorithm that incorporated serial measurements of cervical length for the prediction of preterm birth was compared to that achieved with a single measurement of cervical length at period 1.
Results
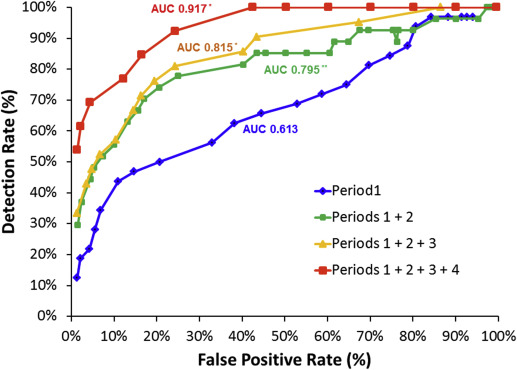
Overall, 441 women with twin pregnancies who were eligible for the study underwent a total of 2374 cervical length measurements. The association of a short cervix (<10th percentile) with preterm birth at <32 weeks persisted in each of the 4 periods of gestation [odds ratio (95% confidence interval): 7.2 (3.1–16.5), 15.3 (6.4–36.7), 10.3 (4.4–24.3), and 23.1(8.3–64.1), respectively]. Compared with a single measurement of cervical length at midgestation (period 1), a stepwise algorithm integrating serial cervical length measurements from all 4 successive gestational age periods resulted in a significant increase in the area under the receiver operating characteristic curve (0.917 vs 0.613, P < .001). Similarly, when a target false-positive rate of 5% was used, the same stepwise algorithm was associated with a higher detection rate (69% vs 28%, P < .001), higher positive likelihood ratio (14.54 vs 5.12), and lower negative likelihood ratio (0.32 vs 0.76) for preterm birth at <32 weeks compared with a single measurement of cervical length at period 1.
Conclusion
Integration of serial measurements of cervical length using a stepwise algorithm in asymptomatic women with twin gestations can improve the detection of women at risk of preterm birth. Prospective studies are needed to validate these findings, and to investigate whether improved risk assessment performance is sufficient to offset the additional costs associated with serial cervical length measurements.
Introduction
Preterm birth (PTB) is the main cause of neonatal mortality and morbidity in twin pregnancies. Although current interventions for the prevention of PTB in women with twins are of limited success, early prediction of PTB in these pregnancies can assist care providers in identifying those women with twin gestation who are at the highest risk of PTB and who may benefit from closer monitoring and administration of antenatal corticosteroids for fetal lung maturation. Furthermore, identification of patients at risk is a prerequisite for testing interventions to reduce the rate of PTB.
Cervical length (CL) at midtrimester, as measured by transvaginal ultrasound, is a powerful predictor of PTB in both singleton and twin gestations. However, given the fact that, in some cases, cervical shortening may become evident only later during the second trimester, it seems reasonable that serial monitoring of CL may improve the overall detection of women who are at high risk of PTB. In an effort to improve the predictive accuracy of CL, measurement of CL is often repeated during the second and early third trimester. However, evidence that serial measurements of CL improve the prediction of PTB is limited, and the results of available studies are conflicting. In a recent systematic review and meta-analysis on the predictive accuracy of changes in sonographic CL over time in singleton and twin pregnancies, Conde-Agudelo and Romero found that the shortening of CL over time had only a low to moderate predictive accuracy for PTB. The contradictory results may be related to the limitations of some of the studies, which have been subject to systematic review and meta-analysis. For example, some studies have a small sample size, and there is variability in the timing of CL measurement, the definition of cervical shortening, and the cutoff of CL used to define a short cervix. In addition, in most of these studies, the analysis of the predictive value of serial measurements of CL was limited to data derived from only 2 sequential measurements of CL.
The aim of the current study was to determine whether the integration of information obtained from serial measurements of CL can improve the prediction of PTB in asymptomatic women with twin gestations compared to a single measurement of CL at 18+0 to 21+6 weeks of gestation.
Materials and Methods
Study population
This was a retrospective study of all women with twin gestations who were followed up in the twins clinic in a single referral center from January 2012 through December 2014. Pregnancies complicated by any of the following conditions were excluded: <3 measurements of CL during gestation, cervical cerclage, uncertain pregnancy dating, indicated preterm delivery at <34 weeks for maternal or fetal indications, birthweight of either twin <500 g, gestational age at delivery <24 weeks, stillbirth of one or both fetuses, monoamniotic twins, monochorionic twins complicated by twin-to-twin transfusion syndrome, or genetic or structural anomalies. The rationale for the exclusion of women who gave birth <24 weeks is that in most cases these women would not have multiple measurements of CL (which is the focus of the current study). In addition, these women most likely represent a different subgroup of pregnancies resulting in late miscarriage or previable PTB for which the cervical changes will be seen very early and will be very evident, and so the contribution of serial monitoring of CL in these cases is expected to me minor. The study was approved by the Sunnybrook Health Sciences Center Research Ethics Board.
Monitoring of CL
All women were followed up by a single physician in the twins clinic of the Sunnybrook Health Sciences Center during the study period. All women followed up in this clinic undergo serial transvaginal measurement of CL every 2-3 weeks between 14-18 weeks and 28-32 weeks of gestation. Progesterone was not used in the management of women with twins and a short cervix given the lack of solid evidence regarding the benefit of progesterone in this context. Cervical cerclage was performed in selected cases of women with suspected mechanical cervical insufficiency (N = 18), and these cases were excluded from the analysis. Women who were noted to have a short cervix were recommended to decrease the level of activity, although it was advised to avoid strict bed rest. There was no standardized protocol with respect to activity restriction. All sonographic measurements included in the study involved only asymptomatic women. Women with preterm labor and women receiving tocolysis for premature contractions were not included in the analysis. The obstetrician in the twins clinic was not blinded to the results of CL measurement.
All sonographic examinations were performed by experienced sonographers. Sonographic CL measurement was performed transvaginally with an empty bladder, according to a standard technique. Briefly, the measurement of CL was performed in a sagittal plane, visualizing the full length of the cervical canal from the internal os to the external cervical os while exerting as little pressure with the transducer as possible. Unless there was evidence of severe cervical shortening, the measurement of CL is repeated following fundal pressure or the Valsalva maneuver. At least 3 measurements were obtained and the shortest measurement was recorded.
Data collection
Data were extracted from the medical charts and included demographic and obstetrical characteristics, chorionicity, validation of gestational age by first-trimester ultrasound, pregnancy complications, presence of cervical cerclage, and neonatal outcome. The reports of all ultrasound examinations performed during pregnancy were reviewed in detail for information on CL.
Predictive value of CL at each period
For each patient, CL was determined at 4 time periods along gestation: 18+0 to 21+6 weeks (period 1), 22+0 to 24+6 weeks (period 2), 25+0 to 27+6 weeks (period 3), and 28+0 to 32+0 weeks (period 4). When >1 measurement of CL was available within any of these periods, the value that was recorded for that period was the average of all CL measurements performed for the individual patient within this time period. The degree of cervical shortening between 2 given time periods was calculated as follows: ([CL in later period – CL in earlier period]/CL in earlier period) × 100. Thus, lower (more negative) values reflect greater cervical shortening.
To determine whether CL has a predictive role at each of the 4 periods, the following measures of accuracy were determined for CL and percent shortening of CL at each of the 4 periods: (1) association of short cervix (<10th percentile within each specific period) with delivery <32 weeks using logistic regression analysis; (2) correlation between CL and gestational age at birth (using Pearson correlation coefficient); and (3) area under the receiver operating characteristic curve (AUC) for delivery <32 weeks.
Integration of serial measurements of CL
To determine whether integration of serial measurements of CL can improve the predictive accuracy for PTB compared with a single measurement of CL at period 1, we compared the performance of 4 models/algorithms that integrated increasing numbers of CL measurements using a stepwise approach ( Supplemental Figure ): (1) CL period 1 < threshold 1 mm ( Supplemental Figure , A); (2) CL period 1 < threshold 1 mm OR CL period 2 < threshold 2 mm ( Supplemental Figure , B); (3) CL period 1 < threshold 1 mm , CL period 2 < threshold 2 mm , OR CL period 3 < threshold 3 mm ( Supplemental Figure , C); and (4) CL period 1 < threshold 1 mm , CL period 2 < threshold 2 mm , CL period 3 < threshold 3 mm , OR CL period 4 < threshold 4 mm ( Supplemental Figure , D).
These models/algorithms were designed using a pragmatic stepwise approach that can be easily applied to clinical practice. Once CL at any given period was below the threshold for that specific period, that result of the model was classified as positive, and no further CL measurements were required. If all CL measurements included in the model were equal or above their corresponding thresholds, the result of the model was classified as negative. Women who had missing CL measurements in the later periods because they gave birth prematurely (eg, women who gave birth at 27 weeks of gestation and therefore could not have a CL measurement in period 4) were classified as either true positive (if any of the previous CL measurements were below their corresponding threshold) or false negative (if all of the previous CL measurements prior to the premature birth were equal or above their corresponding threshold) ( Supplemental Figure ). Women for whom information on CL in ≥1 periods was missing for reasons other than PTB were not included in the calculation of the performance of models that were based on CL measurements in these periods. For this reason, the number of women used for the calculation of the performance of the 4 models was highest for model 1 and lowest for model 4.
To facilitate comparison of the detection rate of the different models, the predictive accuracy of each of the 4 models was determined for the same target false-positive rate (2% and 5%). Practically, the only way on to maintain such a fixed false-positive rate for models that integrate serial measurements of CL was through the use of lower CL threshold values for the early periods (ie, periods 1 and 2) in these models compared with the threshold values used during the same periods for models that integrate only 1 or 2 measurements of CL (ie, models 1 and 2). Thus, for example, the threshold of CL used in period 1 was highest in the case of model 1 and lowest in the case of model 4. An iteration process was used to identify the set of thresholds of CL at each of the periods that yields the highest detection rate for the target false-positive rate for each of the 4 models.
The following measures of predictive accuracy for PTB were calculated for each of the models: (1) AUC, (2) detection rate (or sensitivity), (3) false-positive rate (or 1-specificity), (4) positive and negative predictive values, and (5) positive likelihood ratios (LR+) and negative likelihood ratios (LR–). LR+ >10 and LR– <0.1 were considered to provide strong predictive evidence; LR+ of 5-10 and LR– of 0.1-0.2 were considered to reflect moderate predictive value; and LR+ <5 and LR– >0.2 were considered to reflect only low predictive value.
The same process described above was performed for another set of 4 models that similarly integrated an increasing number of CL measurements but analyzed the percent shortening of CL rather than absolute CL: (1) CL period 1 < threshold 1 mm ; (2) CL period 1 < threshold 1 mm OR percent shortening periods 1→2 < threshold 2 % ; (3) CL period 1 < threshold 1 mm , percent shortening periods 1→2 < threshold 2 % OR percent shortening periods 1→3 < threshold 3 % ; and (4) CL period 1 < threshold 1 mm , percent shortening periods 1→2 < threshold 2 % , percent shortening periods 1→3 < threshold 3 % OR percent shortening periods 1→4 < threshold 4 % .
Statistical analysis
Student t test was used for comparison of mean CL at each of the 4 periods in women who did or did not deliver at <32 weeks. The McNemar test for correlated proportions was used to compare the detection rate of the different models using the model that is based on a single measurement of CL at period 1 (model 1) as reference. The AUC of the different models were compared based on the method of Hanley and McNeil and using the AUC of the model that is based on a single measurement of CL at period 1 (model 1) as reference.
Statistical analysis was performed with software (SPSS v21.0; IBM Corp, Armonk, NY). Results were considered significant when the P value was <.05.
Materials and Methods
Study population
This was a retrospective study of all women with twin gestations who were followed up in the twins clinic in a single referral center from January 2012 through December 2014. Pregnancies complicated by any of the following conditions were excluded: <3 measurements of CL during gestation, cervical cerclage, uncertain pregnancy dating, indicated preterm delivery at <34 weeks for maternal or fetal indications, birthweight of either twin <500 g, gestational age at delivery <24 weeks, stillbirth of one or both fetuses, monoamniotic twins, monochorionic twins complicated by twin-to-twin transfusion syndrome, or genetic or structural anomalies. The rationale for the exclusion of women who gave birth <24 weeks is that in most cases these women would not have multiple measurements of CL (which is the focus of the current study). In addition, these women most likely represent a different subgroup of pregnancies resulting in late miscarriage or previable PTB for which the cervical changes will be seen very early and will be very evident, and so the contribution of serial monitoring of CL in these cases is expected to me minor. The study was approved by the Sunnybrook Health Sciences Center Research Ethics Board.
Monitoring of CL
All women were followed up by a single physician in the twins clinic of the Sunnybrook Health Sciences Center during the study period. All women followed up in this clinic undergo serial transvaginal measurement of CL every 2-3 weeks between 14-18 weeks and 28-32 weeks of gestation. Progesterone was not used in the management of women with twins and a short cervix given the lack of solid evidence regarding the benefit of progesterone in this context. Cervical cerclage was performed in selected cases of women with suspected mechanical cervical insufficiency (N = 18), and these cases were excluded from the analysis. Women who were noted to have a short cervix were recommended to decrease the level of activity, although it was advised to avoid strict bed rest. There was no standardized protocol with respect to activity restriction. All sonographic measurements included in the study involved only asymptomatic women. Women with preterm labor and women receiving tocolysis for premature contractions were not included in the analysis. The obstetrician in the twins clinic was not blinded to the results of CL measurement.
All sonographic examinations were performed by experienced sonographers. Sonographic CL measurement was performed transvaginally with an empty bladder, according to a standard technique. Briefly, the measurement of CL was performed in a sagittal plane, visualizing the full length of the cervical canal from the internal os to the external cervical os while exerting as little pressure with the transducer as possible. Unless there was evidence of severe cervical shortening, the measurement of CL is repeated following fundal pressure or the Valsalva maneuver. At least 3 measurements were obtained and the shortest measurement was recorded.
Data collection
Data were extracted from the medical charts and included demographic and obstetrical characteristics, chorionicity, validation of gestational age by first-trimester ultrasound, pregnancy complications, presence of cervical cerclage, and neonatal outcome. The reports of all ultrasound examinations performed during pregnancy were reviewed in detail for information on CL.
Predictive value of CL at each period
For each patient, CL was determined at 4 time periods along gestation: 18+0 to 21+6 weeks (period 1), 22+0 to 24+6 weeks (period 2), 25+0 to 27+6 weeks (period 3), and 28+0 to 32+0 weeks (period 4). When >1 measurement of CL was available within any of these periods, the value that was recorded for that period was the average of all CL measurements performed for the individual patient within this time period. The degree of cervical shortening between 2 given time periods was calculated as follows: ([CL in later period – CL in earlier period]/CL in earlier period) × 100. Thus, lower (more negative) values reflect greater cervical shortening.
To determine whether CL has a predictive role at each of the 4 periods, the following measures of accuracy were determined for CL and percent shortening of CL at each of the 4 periods: (1) association of short cervix (<10th percentile within each specific period) with delivery <32 weeks using logistic regression analysis; (2) correlation between CL and gestational age at birth (using Pearson correlation coefficient); and (3) area under the receiver operating characteristic curve (AUC) for delivery <32 weeks.
Integration of serial measurements of CL
To determine whether integration of serial measurements of CL can improve the predictive accuracy for PTB compared with a single measurement of CL at period 1, we compared the performance of 4 models/algorithms that integrated increasing numbers of CL measurements using a stepwise approach ( Supplemental Figure ): (1) CL period 1 < threshold 1 mm ( Supplemental Figure , A); (2) CL period 1 < threshold 1 mm OR CL period 2 < threshold 2 mm ( Supplemental Figure , B); (3) CL period 1 < threshold 1 mm , CL period 2 < threshold 2 mm , OR CL period 3 < threshold 3 mm ( Supplemental Figure , C); and (4) CL period 1 < threshold 1 mm , CL period 2 < threshold 2 mm , CL period 3 < threshold 3 mm , OR CL period 4 < threshold 4 mm ( Supplemental Figure , D).
These models/algorithms were designed using a pragmatic stepwise approach that can be easily applied to clinical practice. Once CL at any given period was below the threshold for that specific period, that result of the model was classified as positive, and no further CL measurements were required. If all CL measurements included in the model were equal or above their corresponding thresholds, the result of the model was classified as negative. Women who had missing CL measurements in the later periods because they gave birth prematurely (eg, women who gave birth at 27 weeks of gestation and therefore could not have a CL measurement in period 4) were classified as either true positive (if any of the previous CL measurements were below their corresponding threshold) or false negative (if all of the previous CL measurements prior to the premature birth were equal or above their corresponding threshold) ( Supplemental Figure ). Women for whom information on CL in ≥1 periods was missing for reasons other than PTB were not included in the calculation of the performance of models that were based on CL measurements in these periods. For this reason, the number of women used for the calculation of the performance of the 4 models was highest for model 1 and lowest for model 4.
To facilitate comparison of the detection rate of the different models, the predictive accuracy of each of the 4 models was determined for the same target false-positive rate (2% and 5%). Practically, the only way on to maintain such a fixed false-positive rate for models that integrate serial measurements of CL was through the use of lower CL threshold values for the early periods (ie, periods 1 and 2) in these models compared with the threshold values used during the same periods for models that integrate only 1 or 2 measurements of CL (ie, models 1 and 2). Thus, for example, the threshold of CL used in period 1 was highest in the case of model 1 and lowest in the case of model 4. An iteration process was used to identify the set of thresholds of CL at each of the periods that yields the highest detection rate for the target false-positive rate for each of the 4 models.
The following measures of predictive accuracy for PTB were calculated for each of the models: (1) AUC, (2) detection rate (or sensitivity), (3) false-positive rate (or 1-specificity), (4) positive and negative predictive values, and (5) positive likelihood ratios (LR+) and negative likelihood ratios (LR–). LR+ >10 and LR– <0.1 were considered to provide strong predictive evidence; LR+ of 5-10 and LR– of 0.1-0.2 were considered to reflect moderate predictive value; and LR+ <5 and LR– >0.2 were considered to reflect only low predictive value.
The same process described above was performed for another set of 4 models that similarly integrated an increasing number of CL measurements but analyzed the percent shortening of CL rather than absolute CL: (1) CL period 1 < threshold 1 mm ; (2) CL period 1 < threshold 1 mm OR percent shortening periods 1→2 < threshold 2 % ; (3) CL period 1 < threshold 1 mm , percent shortening periods 1→2 < threshold 2 % OR percent shortening periods 1→3 < threshold 3 % ; and (4) CL period 1 < threshold 1 mm , percent shortening periods 1→2 < threshold 2 % , percent shortening periods 1→3 < threshold 3 % OR percent shortening periods 1→4 < threshold 4 % .
Statistical analysis
Student t test was used for comparison of mean CL at each of the 4 periods in women who did or did not deliver at <32 weeks. The McNemar test for correlated proportions was used to compare the detection rate of the different models using the model that is based on a single measurement of CL at period 1 (model 1) as reference. The AUC of the different models were compared based on the method of Hanley and McNeil and using the AUC of the model that is based on a single measurement of CL at period 1 (model 1) as reference.
Statistical analysis was performed with software (SPSS v21.0; IBM Corp, Armonk, NY). Results were considered significant when the P value was <.05.
Results
Characteristics of study population
A total of 586 women with twin pregnancies were identified during the study period, of whom 441 (75.3%) were eligible for the study and contributed 2374 measurements of CL ( Table 1 ). The rate of PTB at <34 and 32 weeks was 15.9% and 7.9%, respectively ( Table 1 ).
| Characteristic | Value |
|---|---|
| N | 441 |
| Maternal age, y | 32.9 ± 4.1 |
| Chorionicity | |
| DC/DA | 358 (81.2) |
| MC/DA | 83 (18.8) |
| No. of cervical length measurements | |
| Total | 2374 |
| Period 1: 18+0 to 21+6 wk | 688 |
| Period 2: 22+0 to 24+6 wk | 605 |
| Period 3: 25+0 to 27+6 wk | 620 |
| Period 4: 28+0 to 32+0 wk | 461 |
| GA at delivery, wk | 35.4 ± 2.4 |
| <34 wk | 70 (15.9) |
| <32 wk | 35 (7.9) |
| Birthweight, g | |
| Twin A | 2389 ± 557 |
| Twin B | 2333 ± 567 |
Relationship between CL at different periods of gestation and risk of PTB
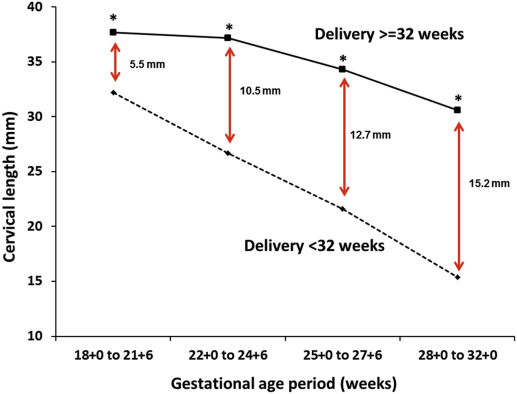
The first question that we addressed was whether measurement of CL at different periods of gestation can identify women who will give birth prematurely. Figure 1 presents the mean CL at each of the 4 periods of gestation in women who did or did not give birth <32 weeks of gestation. The mean CL was significantly lower in women who gave birth <32 weeks at each of the 4 gestational age periods and these differences increased with gestational age ( Figure 1 ). The fact that measurement of CL at any of the 4 periods is predictive of PTB is also reflected by the observation that a short cervix (<10th percentile) at each of the 4 periods was significantly associated with PTB <32 weeks, by the significant correlation between CL at each of the 4 periods and gestational age at birth, and by the AUC for PTB <32 weeks at each of the 4 periods ( Table 2 ).
| GA period | CL, mm, mean ± SD | CL 10th percentile, mm | Association of CL <10th percentile with delivery <32 wk, OR (95% CI) | Correlation with GA at delivery | Delivery <32 wk, AUC (95% CI) |
|---|---|---|---|---|---|
| Period 1: 18+0 to 21+6 wk | 37.3 ± 7.1 | 30 | 7.2 (3.1–16.5) | 0.166 a | 0.72 (0.55–0.88) |
| Period 2: 22+0 to 24+6 wk | 36.4 ± 8.7 | 25 | 15.3 (6.4–36.7) | 0.286 a | 0.85 (0.73–0.98) |
| Period 3: 25+0 to 27+6 wk | 33.5 ± 10.4 | 19 | 10.3 (4.4–24.3) | 0.290 a | 0.85 (0.71–0.98) |
| Period 4: 28+0 to 32+0 wk | 29.7 ± 11.4 | 13 | 23.1 (8.3–64.1) | 0.350 a | 0.89 (0.78–1.00) |
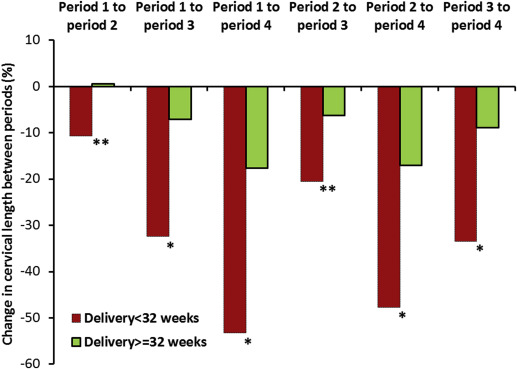
Relationship between cervical shortening and the risk of PTB
The value of serial CL measurements can also be analyzed by means of the relative degree of cervical shortening between successive periods rather than the absolute CL at each period. Similar to the absolute measurements of CL at each period of gestation, the degree of cervical shortening between successive periods (expressed as percent shortening) discriminated between women who did or did not give birth prematurely ( Figure 2 ). The fact that the degree of cervical shortening is predictive of PTB is also reflected by the significant association of a high degree of cervical shortening (<10th percentile) with PTB <32 weeks, by the significant correlation between percent shortening at each of the 4 periods and gestational age at birth, and by the AUC for PTB <32 weeks at each of the 4 periods ( Table 3 ).
| GA periods a | Cervical shortening, mean ± SD | Cervical shortening 10th percentile b | Association of shortening <10th percentile with delivery <32 wk b , OR (95% CI) | Correlation with GA at delivery | Delivery <32 wk, AUC (95% CI) |
|---|---|---|---|---|---|
| Change in CL between periods 1 → 2 | –0.2% ± 20.8% | –26.8% | 7.1 (3.0–17.1) | 0.178 c | 0.76 (0.59–0.94) |
| Change in CL between periods 1 → 3 | –8.6% ± 26.0% | –43.3% | 7.5 (3.0–18.9) | 0.215 c | 0.74 (0.55–0.92) |
| Change in CL between periods 1 → 4 | –19.8% ± 27.9% | –57.2% | 17.0 (6.0–48.0) | 0.301 c | 0.85 (0.71–0.99) |
| Change in CL between periods 2 → 3 | –7.0% ± 21.9% | –31.6% | 6.7 (2.7–17.6) | 0.132 d | 0.62 (0.44–0.80) |
| Change in CL between periods 2 → 4 | –18.5% ± 23.2% | –50.0% | 10.5 (3.2–34.1) | 0.258 c | 0.85 (0.73–0.97) |
| Change in CL between periods 3 → 4 | –10.3% ± 25.6% | –41.0% | 8.1 (2.8–23.3) | 0.124 c | 0.74 (0.57–0.91) |
a Calculated as follows: ([CL in later period – CL in earlier period]/CL in earlier period) × 100, thus, lower (more negative) values reflect greater cervical shortening
b Values <10th percentile reflect cases with greatest (most negative) cervical shortening
c Pearson correlation coefficient, P value <.01
Does the integration of serial measurements of CL improve the predictive accuracy for PTB?
Finally, given that measurement of CL at each of the 4 periods was found to be predictive of PTB, we questioned whether integration of serial measurements of CL at each of these periods using a stepwise algorithm can improve the prediction of PTB ( Supplemental Figure ).
We first addressed this question by comparing the predictive accuracy of models that integrated 2 (periods 1 and 2), 3 (periods 1, 2, and 3), and 4 (periods 1, 2, 3, and 4) successive measurements of CL with that achieved by a single measurement of CL at midgestation (period 1). The AUC for the prediction of PTB <32 weeks increased with the number of CL measurements included in the model (0.795, 0.815, and 0.917 for integration of 2, 3, and 4 measurements, respectively) and was significantly higher than that achieved with a single measurement of CL at period 1 (0.613, P < .005) ( Figure 3 ). Similarly, for a given target false-positive rate (2% or 5%), integration of each additional measurement of CL increased the detection rate and the LR+, and decreased the LR– for PTB <32 weeks ( Table 4 ). The detection rate achieved with a model that integrated all 4 measurements of CL was significantly higher than that achieved with a single measurement of CL at period 1 (for false-positive rate 2%: 62% vs 19%, P = .025; for false-positive rate 5%: 69% vs 28%, P = .019) ( Table 4 ). Measurement of CL at period 2 and period 4 had the largest relative contribution to the overall detection rate ( Table 4 ).