FIGURE 34-1 A: Radiographs of mildly displaced scaphoid fracture that occurred 2 months before. B: CT scan confirms mild humpback deformity, fracture with minor cystic changes.
CLINICAL QUESTIONS
- Do nondisplaced distal radial metaphyseal buckle fractures require cast treatment?
- Is there an outcome difference between long-arm and short-arm cast immobilization for distal radius fractures treated with CR?
- How much and over what time can a distal radius fracture remodel?
- What are the indications for CRPP of distal radius fractures?
- What are the indications for ORIF of distal radius fractures?
- When should ulnar styloid fractures be acutely fixed?
- What is the risk of growth arrest in a distal radius physeal fracture?
- What are the indications for an ulnar shortening osteotomy?
- Which scaphoid fractures should be treated with cast immobilization in children and adolescents?
- What are the indications for percutaneous scaphoid screw fixation?
- Should every scaphoid nonunion in the pediatric age group be treated surgically?
- What is the surgical approach for an acute transscaphoid perilunate dislocation?
THE FUNDAMENTALS
Etiology and Epidemiology
The distal radius (in isolation or with a distal ulna fracture) is the most common site of a pediatric fracture.1–4 Distal radius fractures occur most commonly in adolescent patients, almost exclusively secondary to a fall. A fracture during a sporting event is a common occurrence, in particular skateboarding, snowboarding, and soccer goalkeeping, among others.5–7 Protective wrist guards are of benefit in reducing fracture risk in these sports.8 Children with obesity and poor bone mineralization are at more risk for a fracture with a routine fall.9–12 Repetitive stress loading of the wrist, such as with gymnastics, can lead to a distal radial physeal stress fracture (see Chapter 39).13–16 Triangular fibrocartilage complex (TFCC) tears (see Chapter 42) are more common with positive ulnar variance, and Kienbock disease (avascular necrosis [AVN] of the lunate) (Figure 34-2) is more common with negative ulnar variance.
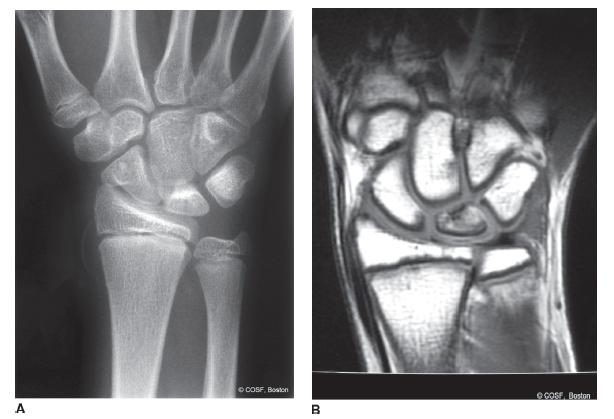
FIGURE 34-2 A: Mild Kienbock disease anteroposterior (AP) radiograph and (B ) confirmed on magnetic resonance imaging (MRI) scan.
Clinical Evaluation
Children and adolescents with a distal radius fracture will present with localized pain and restricted motion. Nondisplaced fractures in the young may have minimal pain or restrictions due to periosteal stabilization. Displaced fractures of the distal radius and ulna will have obvious deformity. With markedly displaced fractures, neurovascular (NV) compromise can occur. Open fractures do occur and are more at risk for NV impairment.
Distal forearm fractures are classified radiographically by location of fracture (metaphyseal or physeal), direction (volar or dorsal) and degree of displacement, and bone involved (radius, ulna, or both). Metaphyseal fractures are further defined as torus/buckle (one cortex and therefore stable), both cortices (potentially unstable), and complete, displaced fractures. Most distal forearm fractures extend due to the fall on an outstretched wrist mechanism of injury. A variant is the pediatric Galeazzi fracture dislocation: a displaced distal radial metaphyseal fracture with either a distal ulnar physeal fracture or distal radioulnar joint (DRUJ) dislocation. Transphyseal fractures are less common than metaphyseal fractures and are defined by standard Salter-Harris classification.17 Salter-Harris type II, followed by Salter-Harris type I, injuries are the most common displaced distal radial physeal fractures. Intra-articular fractures are uncommon with an open physis (Salter-Harris type III) but are more and more common with skeletally mature adolescents during their highly competitive sports participation. Classification of intra-articular distal radius fractures is similar to adults. The use of CT scans is necessary to define displacement, number of fracture fragments, and operative indications.
Scaphoid fractures are more subtle than distal radius and ulna fractures by history and exam.18,19 Snuffbox tenderness, scaphoid tubercle tenderness, and axial compression of the thumb are all sensitive physical exam findings for an acute scaphoid fracture or chronic nonunion, but axial compression is the most specific. Plain radiographs need to include a 30-degree ulnar deviation AP view (scaphoid view). Scaphoid fractures are defined by location of the fracture (waist, proximal, or distal pole) and displacement (non-displaced, <2 mm, >2 mm). Proximal pole fractures have the highest risk of AVN. The use of CT scans is often necessary to define operative indications (displaced fractures >2 mm) but need to be taken in the longitudinal plane of the scaphoid to be accurate.20,21 The use of MRI scans is appropriate for patients with snuffbox tenderness, scaphoid tubercle tenderness, and/or thumb axial compression pain but normal plain radiographs22–25 (Figure 34-3). Scaphoid nonunions usually present long after the fracture and often with lack of treatment since the time of injury. The pain is usually mild, worse with wrist extension and axial loading activities, and often not debilitating. There is generally limited wrist extension and scaphoid-specific pain on physical exam. X-rays will reveal the nonunion and possible AVN of the proximal pole with scaphoid collapse (dorsal intercalary segment instability [DISI] pattern with the distal pole of the scaphoid flexed and lunate extended on the lateral radiographic image).

FIGURE 34-3 A: Original radiographs of the scaphoid were interpreted as negative for fracture. B: MRI 3 weeks later reveals scaphoid fracture. C: Percutaneous scaphoid screw fixation was the treatment of choice for this patient with radiographic healing noted.
Trans-scaphoid perilunate dissociations are the most common type of acute perilunate carpal dislocations. These dislocations are rare and secondary to a high-velocity injury in extreme wrist dorsiflexion. An acute median neuropathy is common with a complete perilunate dislocation. There is usually marked swelling, deformity, and pain. Inexplicably, some of these patients present days after injury, which heightens the risk of AVN of the scaphoid proximal pole and/or dislocated lunate. The force of a perilunate dislocation starts radially either through the scaphoid as a fracture or through the scapholunate ligament; it then extends between the lunate and capitate dissociating the proximal and distal carpal rows; and finally it returns to the ulnocarpal joint in a clockwise fashion through the lunotriquetral joint (Figure 34-4). In a complete injury, the lunate usually ends up volar in the carpal canal, and the radius and capitate become colinear.
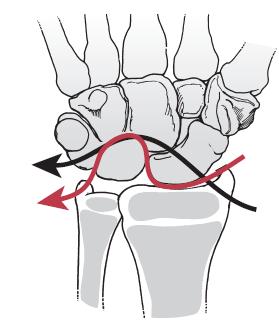
FIGURE 34-4 Disruption pattern of a trans-scaphoid perilunate dislocation (black line) or pure perilunate dislocation (red line) noted by illustration. (From Beaty JH, Kasser JR.Rockwood & Wilkins Fractures inChildren. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2010.)
Surgical Indications
All displaced fractures and dislocations of the distal forearm and wrist require treatment. The major defining factors for treatment type closed reduction (CR), closed reduction percutaneous pinning (CRPP), or open reduction and internal fixation (ORIF) for distal radius and/or ulna fractures is the age of the patient, degree and direction of displacement, and any articular involvement. If the child is young (>2 years of growth remaining), the fracture is extra-articular and displaced in the plane of motion of the joint and has <20 degrees of malangulation without malrotation, then the bone will eventually remodel. Using CR and cast treatment is appropriate with close follow-up.26–28 Some fractures treated with CR will redisplace and require either repeat CR or CRPP (Figure 34-5).
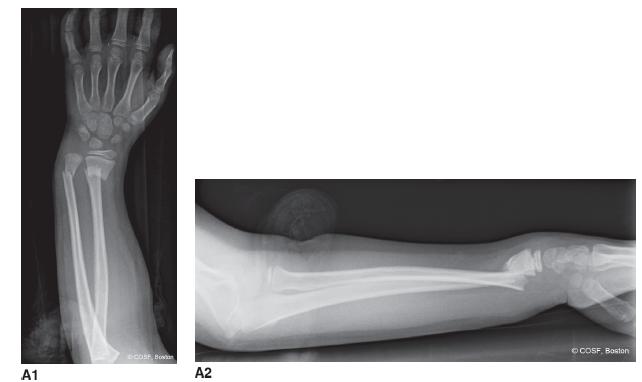
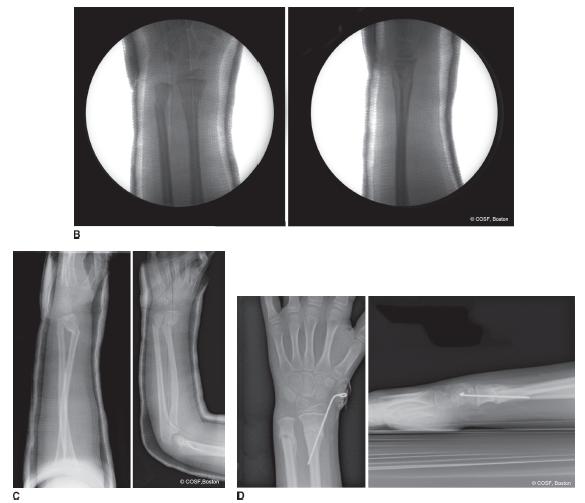
FIGURE 34-5 A: Injury films of displaced distal radius and ulna fractures. B: Conscious sedation reduction in emergency department is near-anatomic reduction. C: Loss of reduction in cast is noted on radiographs 13 days later. D: CRPP to anatomic alignment and healed fractures just before pin removal in office.
In skeletally mature adolescent patients, CRPP or ORIF is indicated for displaced fractures to restore radial inclination, physiologic ulnar variance, and DRUJ alignment. All displaced intra-articular fractures require anatomic reduction and rigid fixation.
Displaced scaphoid fractures29 and scaphoid nonunions require anatomic reduction and fixation. Nondisplaced, acute fractures without bone loss, and proximal pole scaphoid fractures, can be treated with percutaneous screw fixa-tion.30 Acute fractures and chronic nonunions with bone loss require ORIF with bone graft to restore carpal alignment and expedite healing.31–34
All displaced perilunate dislocations require operative reduction and stabilization. Although there is debate about the method of treatment (CRPP or ORIF) and surgical approach with open reduction (volar, dorsal, or combined), there is no debate about the need for reduction and stabilization for the best results.
SURGICAL PROCEDURES
 Closed Treatment of Stable Fractures
Closed Treatment of Stable Fractures
Nondisplaced unicortical fractures of the distal radius and/ or ulna metaphysis are stable injuries. A removable Velcro splint, posterior plaster or fiberglass splint, or bivalve cast immobilization have all been successful forms of treatment.35,36 There is some evidence that these patients may not need to return for follow-up appointments and still have uncomplicated outcomes.37 The only potential problem is mistaking a bicortical, unstable fracture for a stable injury. The bicortical fractures may have been more displaced at the time of injury and can redisplace in nonrestrictive immobilization. Nondisplaced metaphyseal distal radius and/or ulna fractures are usually clinically healed by 3 to 4 weeks, at which time the immobilization can either be discontinued at home by patient and family or in the office by medical personnel. Repeat radiographs are often not obtained.
 CR of Distal Radius and Ulna Fractures
CR of Distal Radius and Ulna Fractures
Displaced distal radius and/or ulna fractures usually require reduction to realign the bones and joints and lessen the risk of further displacement over the next 3 weeks of healing. The reductions are generally performed in the emergency room with conscious sedation. Conscious sedation is performed by the emergency room attending staff with in-hospital anesthesia attending as backup. Once the patient is adequately sedated, the CR is achieved in a series of steps. For metaphyseal fractures with bayonet apposition, the deformity is initially accentuated (Figure 34-6A). The degree of deformity accentuation needed to unhinge a bayonet apposition fracture can be extreme, to the point of instilling nausea in the observing health care personnel. Once the fracture is unhinged and the dorsal periosteum is relaxed, the fracture fragment is “walked” distally with the extension deformity maintained. This maneuver will get the fracture out to length, but it takes very strong intrinsics and thumbs for most fractures. Many fall short with these first two maneuvers. Then the distal fracture fragment is reduced onto the proximal fragment metaphysis (Figure 34-6B) with dorsal to volar thumb pressure. Complete reduction may take several back and forth maneuvers until the fracture is anatomic. Anything less than anatomic will have a higher risk of redisplacement over the next 3 weeks. Anatomic reduction can be felt by dorsal bony alignment, seen by loss of obvious deformity, and confirmed by fluoroscopy. Following anatomic reduction, the choice is well-molded cast immobilization or CRPP. Irreducible fractures require an open reduction by volar approach to extract interposed periosteum and/or pronator quadratus (PQ).38–40
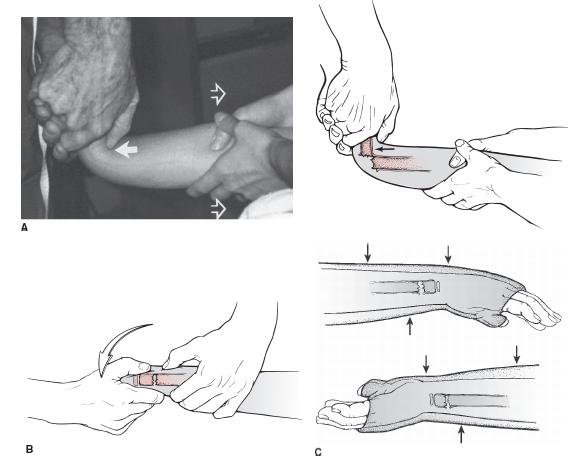
FIGURE 34-6 Illustrations of CR of distal radial metaphyseal fracture note the accentuation of the deformity (A ) followed by reduction of the fracture by bringing the dorsal, distal fragment over the top of the volar, proximal fragment. B, C: Three-point molding is performed with cast application. (From Beaty JH, Kasser JR.Rockwood & Wilkins Fractures in Children. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2010.)
Displaced physeal fractures require a gentler reduction. This can usually be performed with finger trap distraction and dorsal to volar finger reduction (Figure 34-7). The reduction is again performed under conscious sedation. Avoiding additional injury to the distal radius physis with reduction is imperative. This is usually not a difficult reduction. The reduction can also be done under hema-toma block but does require a noncombative patient to prevent shear and compression stress injury to the physis. Anatomic reduction is confirmed by fluoroscopic images.
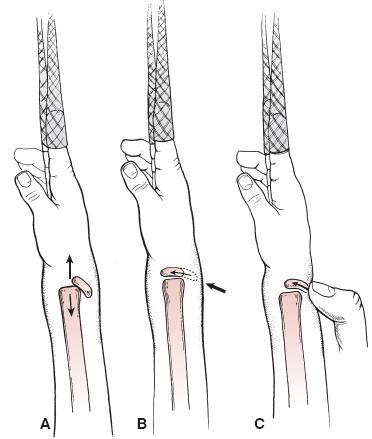
FIGURE 34-7 Illustration of distal radial physeal fracture reduction. Longitudinal traction (A ) is followed by gentle dorsal-to-volar pressure on the distal epiphysis (B ), usually preformed by the surgeon’s thumb (C ). The reduction should be atraumatic to lessen the risk of growth arrest. Finger trap distraction and stabilization with a few pounds can help. (From Beaty JH, Kasser JR.Rockwood & Wilkins Fractures inChildren. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2010.)
In both metaphyseal and physeal fractures, the dorsal periosteum acts as a tension band in helping maintain reduction. The wrist is positioned in slight (∼20 degrees) palmar flexion to provide dorsal periosteal tension. Cast padding and molding are key to providing external support for maintaining reduction. A dorsal mold directly over the fracture and a more proximal volar mold provide three-point fixation (Figure 34-6C). The dorsal mold cannot be too distal, or it will lead to venous congestion due to outflow obstruction on the dorsum of the hand. A straight ulna border and anatomic radial bow mold of the forearm are required. The results of long-arm and short-arm cast immobilization are equivalent,26,28 including prospective randomized studies.41,42 The most important factor is the quality, not the length, of the cast. The quality of the cast molding can be measured by the cast index, which is the sagittal diameter divided by the coronal diameter at the fracture site. A value of 0.7 or less defines a well-molded cast and carries less risk of loss of reduction (Figure 34-8A).

FIGURE 34-8 A: Markedly displaced distal radial physeal fracture treated with CR cast immobilization with excessive wrist flexion mold on lateral radiograph. B: CR of radius and ulna metaphyseal fractures with a poor cast index noted. The obvious loss of reduction is evident.
Even with acceptable reductions and casts, there is a high rate of loss of reduction in distal radial metaphyseal fractures.43–49 On average, the incidence of loss of reduction is 20% to 30%. Higher rates of fracture instability occur with isolated distal radial metaphyseal fractures,49incomplete fracture reduction,44,45 and initial displacement >30 degrees, and the highest rates occur with complete displacement.50 The decision for the surgeon then is to allow the fracture to remodel; do a repeat CR and new cast application; or perform a CRPP. Ultimately, the choice among these options is dependent on the age of patient; degree of deformity; amount of fracture healing; and patient, parent, and surgeon preferences. Physeal fractures will remodel remarkably and are at risk for growth arrest if a repeat reduction is performed after 5 days from injury.51
 CRPP of Distal Radius Fractures
CRPP of Distal Radius Fractures
Due to the high rate of loss of reduction for distal radius metaphyseal fractures treated with CR cast immobilization, many centers perform CRPP as the primary approach for the fractures with complete displacement.52 Evidence by prospective study of distal radial metaphyseal fractures47,48 reveals that the results of CRPP and CR cast immobilization are equivalent at 2 years postinjury if (1) there is sufficient growth remaining for remodeling and (2) repeat reductions are performed when the fracture redisplaces in a cast. The surgeon, patient, and family can choose what is the best treatment for the patient (i.e., there is clinical equipoise). In older patients, there is not sufficient time for remodeling, so CRPP or ORIF is indicated in the skeletally mature or near skeletally mature patient with an unstable, displaced fracture (Figure 34-9).

FIGURE 34-9 A: Injury films reveal markedly displaced distal radial physeal and ulnar metaphyseal fractures. B: The radial physeal fracture was treated with CRPP and the ulna fracture with CR. C: Healed fractures at 2 months post-CRPP. Epiphyseal and metaphyseal pin tracks still evident, but no physeal arrest is present.
In addition, distal radial physeal fractures with median neuropathy are candidates for CRPP to avoid NV compromise and/or unacceptable loss of reduction.53,54 Loss of reduction after initial CR cast immobilization of metaphyseal fractures can be treated with CRPP, but be careful about late reduction (more than 5 days postfracture) in physeal fractures due to risk of growth arrest. Finally, open fractures are candidates for CRPP, external fixation, or ORIF after operative washout of the contaminated bone and soft tissues.
The technique for the CR in the operating room under general anesthesia is the same as described by CR under conscious sedation in the emergency room. Once the fracture is aligned in the AP and lateral planes, sterile prep-ping and draping are performed. The arm is abducted onto a fluoroscopic arm table. Confirmation of the anatomic reduction on the fluoroscopic images is again obtained prior to pinning. Single or double pin techniques are used depending on the age of the patient and stability of the fracture. Blind pinning is avoided to prevent injury to the radial sensory nerve and/or extensor tendons. The first, and sometimes only, pin is placed obliquely from distal to proximal and radial to ulnar. Outlining the desired trajectory of the pin with a skin marker is helpful. A small incision is made distal to the radial styloid if the epiphysis is the entry site (distal physeal fractures and metaphyseal fractures with a short distal metaphyseal segment). The incision is more proximal with a larger distal metaphyseal segment, so the pin can avoid the physis and pass exclusively in the metaphysis. Skin and subcutaneous dissection down to the bone is performed, and retractors are placed to protect the neighboring extensor tendons and radial sensory nerve. The pin is placed against the bone to match the planned trajectory marked on the skin. Fluoroscopic images are used to confirm the pin entry site, projected path, and to avoid false entry into the joint or surrounding important soft tissues. The pin is passed on oscillation with power to prevent entanglement of the soft tissues on the pin. The proximal ulnar cortex is penetrated proximal to the fracture site. The stability of the fracture is tested manually and with fluoroscopy. If the single pin is sufficient, then the CRPP is complete. If there are instability concerns, then a second indentllel radial pin or a crossed pin is placed.
An additional crossed pin may be placed from distal ulnar to proximal radial with the entry point between the fourth (extensor digitorum communis) and fifth (extensor digiti quinti) dorsal wrist compartments. The pin(s) is(are) left out of the skin, bent and cut, and dressed sterilely in a bulking fashion to prevent irritation, infection, or migration (Figure 34-10). Even some intra-articular fractures can be treated with CRPP (Figure 34-11).

FIGURE 34-10 Small incision noted with pins left out of skin for removal at 4 weeks.
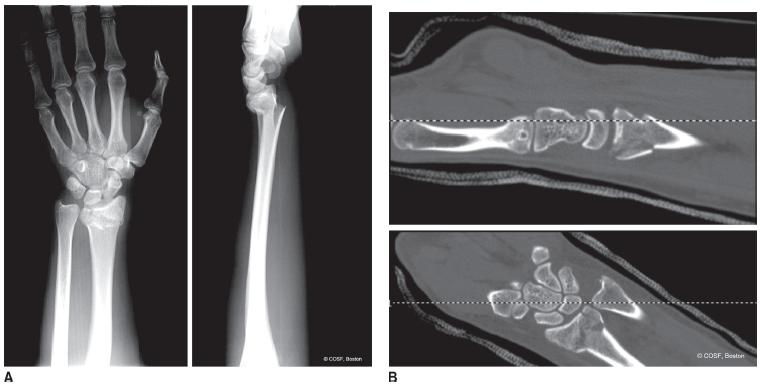
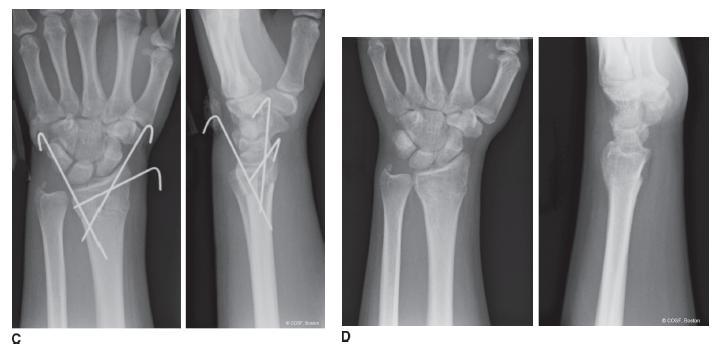
FIGURE 34-11 A: Injury films of displaced metaphyseal fracture with intra-articular extension. B: CT images of articular alignment. C: CRPP with stabilization of fracture fragments. D: Healed fracture with pins out.
 ORIF of Distal Radius Fractures
ORIF of Distal Radius Fractures
If winning isn’t everything, why do they keep score?
—Vince Lombardi
There are many different techniques for ORIF of an adolescent distal radial fracture. Volar and dorsal plating; locked, neutralization, and compression plating; segmental fixation systems; and pin fixation have all been used successfully.55,56
The choice of surgical approach and instrumentation is often fracture and patient specific (Figure 34-12). The goals are the same regardless of implant choice: anatomic, stable reduction of both the extra-articular and intra-articular fracture fragments that allows for full rehabilitation. That said, like the adult, the present volar distal radius locked, segmental fixation systems are effective for the adolescent displaced, unstable fracture that requires ORIF (Figure 34-13).
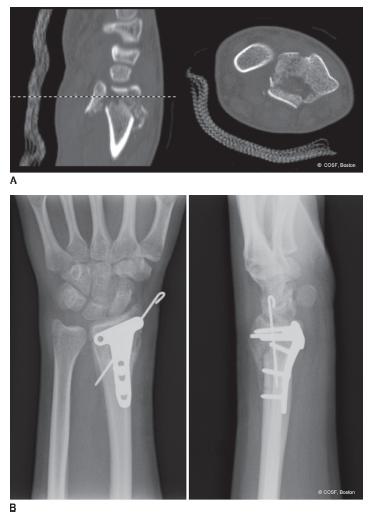
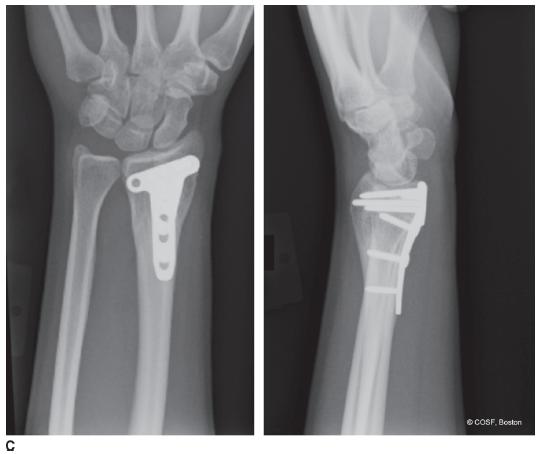
FIGURE 34-12 ORIF of distal radius with T plate and supplemental pin fixation. A: Injury CT scan revealing intra-articular displacement. B: ORIF with T buttress plate and supplemental styloid pin 1 month postoperative. C: One year after ORIF with anatomic alignment and asymptomatic hardware.


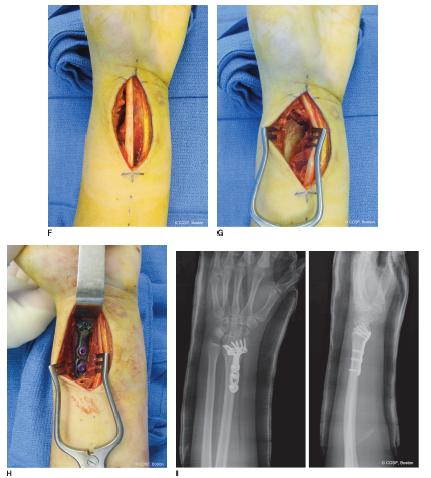
FIGURE 34-13 A: Displaced distal radius metaphyseal and intra-articular fracture. B: Emergency department postreduction radiographs in cast. C: Representative postreduction CT scan images revealing joint displacement. D: Clinical appearance after decreased swelling over 5 days preoperatively. E: Planned plate for fracture fragment specific volar fixation. F: Volar approach via FCR tendon sheath. G: Exposed fracture site with reduction. H: Plate fixation of fracture anatomically. I: Radiographs of ORIF with volar plating system.
A volar approach to the distal radius is used.57,58 The flexor carpi radialis (FCR) tendon sheath is incised and the radial artery protected. The FCR tendon is mobilized. The digital flexors are swept ulnarly off the PQ. A moist sponge followed by a deep retractor is very effective. Crossing vascular channels are cauterized. The PQ is elevated off the radius with a deep linear incision to bone. If there is intra-artic-ular involvement, the pronator is elevated with an upside-down “L” incision all the way to the ulnar side of the radius. Subperiosteal retractors are placed radially and ulnarly after full subperiosteal exposure is performed of the bone and fracture site. This approach and technique are now commonplace for the modern-day orthopaedic trainee, as so many of the adult distal radius fractures are now plated volarly.
The fracture is cleansed of hematoma and reduced using saline irrigation, suction, dental picks, and elevators. Temporary small, smooth wire fixation is used to align the extra-articular and, if present, intra-articular fracture fragments. Often these wires can be placed through the designated holes in the plate. Confirmation of the reduction is obtained with fluoroscopic imaging. A plate with appropriate side (left or right) and size (length and width) is chosen and fixed to the bone with smooth wires through the guide holes proximal and distal to the fracture site. Final confirmation of proper positioning on the radius in terms of proximal-distal, radial-ulnar, and plate angle orientation is obtained with direct and fluoroscopic visualization. The proximal slotted screw is placed first. Finally, tinkering of the distal alignment is performed if necessary, and then the distal pegs or screws are placed. In most adolescent fractures, nonlocking screws are appropriate, though pegs and locking screws can clearly be used as needed. Anatomic reduction and rigid internal fixation are obtained, which allows for early motion and protected rehabilitation while the bone and soft tissues are healing.
 Galeazzi Fracture Dislocations
Galeazzi Fracture Dislocations
Galeazzi fracture dislocations are defined as a fracture of the distal radius and DRUJ dislocation. In children, the injury is more commonly a distal ulna physeal injury than a DRUJ ligamentous disruption and is called a Galeazzi equivalent lesion.59–65 Galeazzi fracture dislocations are rare injuries and are classified by the type (incomplete or complete) and direction of displacement of the radius fracture (volar or dorsal). Most lesions have dorsal displacement of the radius fracture. Incomplete injuries can be successfully closed reduced. The more common apex volar, dorsally displaced incomplete fracture is a supination deformity as well. Pronation and dorsal-to-volar pressure will reduce the fracture and align the DRUJ. The opposite reduction maneuver is performed for the apex volar, pronation deformity: The forearm is supinated and volar-to-dorsal pressure is applied to reduce the radius fracture, ulnar physeal fracture, or DRUJ. If the DRUJ is unstable with a true Galeazzi, then indentllel, transverse, percutaneous pinning of the ulna to the radius is performed to reduce the DRUJ anatomically.
With complete radius fractures, ORIF of the radius is performed (Figure 34-14). The volar approach to the radius through the FCR sheath is utilized. The PQ and origin of the flexor pollicis longus are elevated off the radius subperiosteally. The fracture is debrided of hematoma and callus. The radius fracture is anatomically reduced with bone- and plate-holding clamps. Compression plating is performed. The ulnar physeal fracture or DRUJ is anatomically reduced before plating, and then the stability tested after plating. If stable, then the forearm is held in pronation for apex volar fractures and supination for apex dorsal fractures. If the DRUJ is unstable, two transverse smooth pins are placed from ulna to radius below the physes to maintain anatomic ligament positioning during soft tissue and bony healing (Figure 34-15). The pins are removed in the office at 4 weeks when the cast is changed from long to short arm. A total of 6 weeks of immobilization is performed. In the case of displaced ulnar physeal fractures, a radiograph at 6 months is recommended to identify a growth arrest before deformity occurs.

FIGURE 34-14 A: Injury film with diaphyseal radius fracture and displaced DRUJ. B: ORIF of radius fracture with stable closed reduced DRUJ that healed anatomically. Full, stable range of forearm, wrist, and elbow motion was restored.

FIGURE 34-15 A: Multiple trauma motor vehicle accident patient with open ankle fracture, closed chest trauma, and displaced distal radius and ulna physeal (Salter-Harris type III) fractures as noted by injury radiographs. B: CRPP of radius performed with cross pin stabilization of DRUJ.
 ORIF of Acute Displaced Scaphoid Fractures and ORIF of Scaphoid Nonunion with Bone Graft
ORIF of Acute Displaced Scaphoid Fractures and ORIF of Scaphoid Nonunion with Bone Graft
Winning is overrated. The only time it is really important is in surgery and war.
—Al McGuire
All scaphoid nonunions require open repair. There are some acute and subacute scaphoid fractures that are displaced and require reduction and stabilization. Use of CT scans will distinguish these operative fractures from nonoperative or percutaneous fixation fractures. The sagittal views will reveal a flexed scaphoid (“humpback” deformity) and an extended lunate (DISI) pattern. There may be volar comminution that will require supplemental bone graft, like a nonunion, to restore anatomic carpal alignment. Without operative reduction and fixation, these fractures are at risk for nonunion and eventual arthrosis.66 All established scaphoid nonunions will require bone graft to restore carpal alignment. In the adolescent population, nonvascularized bone graft (iliac crest) is highly effective, so vascularized grafting is rare in this age group.67,68 Any persistent nonunion will eventually result in wrist arthrosis (scaphoid nonunion advanced collapse [SNAC] wrist) if restoration of carpal alignment and scaphoid bony healing is not achieved.
Although smooth pins have been successfully used for fixation in both acute fractures and nonunions, the standard now is an intraosseous screw (Acutrak, Acumed, Hillsboro, OR; Herbert, Zimmer, Inc., Warsaw, IN; or Synthes, West Chester, PA). Volar and dorsal surgical approaches have been used successfully. Our preference is a volar approach to directly visualize the fracture or nonunion site; assess fracture reduction or nonunion defect; and, if necessary, exactly measure the bone defect and size of graft needed to restore anatomic alignment.69 In cases with DISI deformity, a temporary oblique smooth wire (0.62″) is placed from the radial styloid across the lunate into the distal carpal row to colinearly align the lunate fossa, lunate, and capitate. By anatomically positioning the lunate, the volar defect of the scaphoid is precisely measurable.
A volar curvilinear approach, centered over the scaphoid tubercle, is used. The distal FCR sheath is incised and the tendon mobilized. Distally the dorsal edge of the thenars is elevated while protecting any radial sensory nerve cutaneous branches that may cross the operative field. The volar branch of the radial artery is isolated and protected. A preoperative Allen test to identify the patient with an incomplete carpal vascular arch is mandatory in case the volar artery branch is ligated or used as a pedicle graft in nonunion surgery.70 The wrist capsule is incised over the waist of the scaphoid while protecting the FCR tendon. The displaced fracture or nonunion site is identified. Often the radioscaphocapitate ligament can be preserved. If it is incised, it is repaired with wound closure. Capsular elevation off the scaphoid distal pole, scaphotrapezial joint, and radial trapezium is performed. The entry site for the cannulated smooth pin and screw is isolated. At times, proper pin alignment in the “1-1” position (exactly centered on the AP and lateral scaphoid fluoroscopic images) requires rongeur removal of the radial, volar trapezium. Smooth curved retractors (either from the system or Freer elevators) are placed in the radioscaphoid joint to elevate the scaphoid and allow full visualization of the entire scaphoid. Distraction of the thumb ray by an assistant or your nondominant hand is very helpful. Small towel rolls under the wrist allow for more extension and ulnar deviation to better visualize the scaphoid waist and align the proximal and distal poles.
The fracture is anatomically reduced. If there is a volar defect, the appropriate amount of radial or iliac crest autograft, allograft, or bone morphogenetic protein (BMP) is used (Figure 34-16). Our preference is structural autograft, both for healing and prevention of collapse with screw compression. In the cases of nonunion, the proximal and distal poles are debrided of fibrous tissue back to bleeding bone. Measurement of the volar defect is made. A tricortical iliac crest graft is obtained (see Sidebar). The bone graft is meticulously trimmed to be an exact fit with dorsal-to-volar and radial-to-ulnar tilting of the trapezoidal graft. The cortex of the graft is set to align with the proximal and distal pole cortices. Once the acute fracture or nonunion graft is impacted in place, the “1-1” positioned cannulated wire is passed from the distal pole into the proximal scaphoid. Pin measurement is made from the instrumentation system used, but you need to take into account the length loss with screw compression. In most systems, a 2- to 4-mm reduction in screw length from the cannulated pin length measurement is necessary to prevent screw penetration into the joint. Depending on the system, drilling over the wire is performed. The graft needs to be either manually stabilized or held in place with a second smooth wire during drilling and screw placement. The appropriate-length screw is placed over the wire while inspecting intermittent fluoroscopic images. The screw needs to be completely buried in the bone, without proximal extrusion or distal penetration into the joint. Compression across the fracture or nonunion site is necessary while restoring anatomic scaphoid alignment. All of this is confirmed by fluoroscopic images (Figure 34-17). If a translunate wire was placed to restore carpal alignment, that smooth pin is now removed. The lunate should stay in neutral alignment at rest and with wrist motion. The scaphoid should move as a single, stable unit. No crepitus should be heard or felt with full wrist motion. If there is, then the screw is too long and needs to be changed. The graft should be stable and not impinge with full radial deviation or flexion. If it protrudes volarly and impinges, the graft edges need to be gently trimmed with small rongeur without destabilizing the graft or fixation. Capsular closure including any incised volar ligaments is performed with absorbable suture. Layered closure is completed while protecting the radial artery. A bivalved short-arm thumb spica cast is applied.


FIGURE 34-16 A: Scaphoid nonunion is exposed and defect measured. B: Iliac crest is inset before screw fixation. C: Healed scaphoid nonunion with screw in desired location.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


