Diseases of the Vulva and Vagina
Amelia M. Jernigan
Robert L. Giuntoli II
Vulvar and vaginal disease should be understood by its presentation, etiology, location, and associated systemic and laboratory findings. Clinicians should have a low threshold to biopsy any suspicious vulvar abnormalities because the appearance of malignant lesions is often similar to that of benign processes. The majority of patients with vulvar cancer experience symptoms for at least months prior to diagnosis. Early biopsy of suspicious lesions is preferable in order to make a diagnosis of vulvar and vaginal malignancies, if present, and to potentially avoid progression to advanced disease.
ANATOMY OF THE VULVA AND VAGINA
The vulva is that area of skin encompassing the labia majora to the hymen. See Chapter 26.
The vulva is bordered laterally by the genitocrural folds, anteriorly by the mons pubis, and posteriorly by the perineal body. The medial side of the labia minora to the hymen is known as the vulvar vestibule or introitus.
Hart line is the thin zone of color and texture change between the labia minora and the vestibule, marking the transition from the skin of the external genitalia to the mucosa of the vestibule.
Within the vestibule lie the urethral meatus, vaginal introitus, ostia of Bartholin glands (major vestibular glands), minor vestibular glands, and Skene ducts.
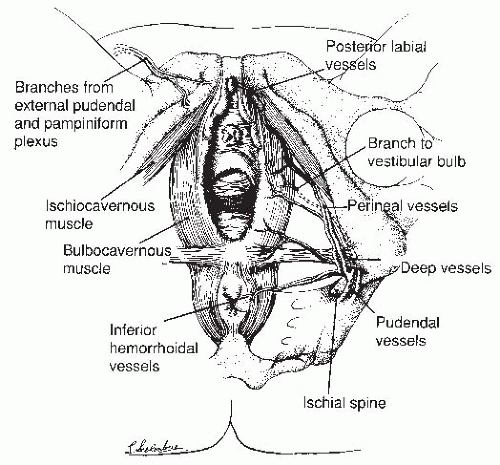
Branches of the external and internal pudendal arteries provide the vascular supply to the vulva (Fig. 44-1).
Sensory innervation of the anterior vulva is via the genitofemoral nerve and the cutaneous branch of the ilioinguinal nerve, whereas the posterior vulva and the clitoris are innervated by the pudendal nerve.
The medial group of superficial inguinal nodes collects the lymphatic drainage of the vulva (Fig. 44-2).
The vagina is a hollow viscus extending from the hymenal ring to the vaginal fornices surrounding the proximal cervix; it is lined by hormone-responsive nonkeratinized stratified squamous epithelium.
The vascular supply of the vagina is provided by the vaginal branch of the internal iliac artery and extensions of the uterine artery that form an anastomotic plexus along the lateral vaginal sulci.
The distal vagina also receives blood from pudendal vessels, and the posterior wall receives contributions from the middle rectal artery.
The vagina is innervated by fibers from the pudendal nerves and the vaginal plexus, which arises from the hypogastric plexus (sacral rami S2 to S4).
The primary sites of lymphatic drainage for the vagina are the hypogastric, obturator, and external iliac lymph nodes via the lateral perivaginal plexus.
The distal third of the vagina may also drain to the inguinofemoral nodes, and the posterior vagina may drain to the inferior gluteal, presacral, or perirectal lymph nodes.
INFECTIOUS DISEASES OF THE VULVA
Sexually transmitted, viral, and fungal infections and parasite infestations of the vulva and vagina are discussed separately in Chapter 28.
Bacterial skin infections of the vulva include folliculitis and furunculosis, most frequently caused by Staphylococcus, and cellulitis secondary to infection with Staphylococcus or Streptococcus.
Treatment of initial infection: warm compresses three times a day (tid) and cephalexin 500 mg orally (PO) four times a day (qid) or dicloxacillin 500 mg PO qid or clindamycin 300 to 450 mg PO tid
For recurrent infections: Add to previous regimen Hibiclens washes + 2% mupirocin ointment tid × 10 days.
DERMATOSES AND INFLAMMATORY CONDITIONS
Behçet Syndrome
Behçet syndrome is a rare chronic disease characterized by a triad of relapsing oral ulcers, genital ulcers, and ocular inflammation. The disease is most common in Japan and the Middle East.
Other findings include acne, cutaneous nodules, thrombophlebitis, and colitis.
Genital ulcers are small, painful, and deep and may result in fenestration of the labia. Ulcers generally heal in 7 to 10 days.
Treatment options include topical (betamethasone valerate ointment 0.1%), intralesional (triamcinolone, 3 to 10 mg/mL, injected into ulcer base), or systemic corticosteroids (prednisone 1 mg/kg for severe involvement, especially central nervous system).
Hidradenitis Suppurativa
Hidradenitis suppurativa is a chronic, painful apocrine gland disorder resulting from chronic occlusions of follicles that causes deep, suppurated subcutaneous nodules that form sinus tracts and confluent masses. The axillae and anogenital region are most frequently involved. The lesions wax and wane; flares are common with menstruation. The lesions ulcerate, resulting in draining sinuses and extensive scarring.
The severity of this disease varies, and it can be graded by the Hurley clinical staging system:
Stage I: single or multiple abscesses but no sinus tracts or scarring
Stage II: recurrent abscesses, tract formation and scarring, widely separated lesions
Stage III: diffuse or near diffuse involvement or multiple interconnected sinus tracts and abscesses across the entire area
Superinfection of hidradenitis suppurativa is polymicrobial and cultures help guide treatment. The effectiveness of medical therapy wanes as deeper tissues become involved.
Treatment options are extensive and are approached in stepwise fashion.
Advise patients to wear loose, light clothing; avoid manipulation of lesions or trauma to the area (e.g., with loofah sponges); keep the area dry; and use gentle, nonirritating cleansers.
Stage I disease: Topical therapy with clindamycin 1% twice a day (bid) with or without intralesional corticosteroids may be a useful initial approach to stage I (mild) disease. After this, 7 to 10 days of doxycycline, minocycline, clindamycin, or amoxicillin clavulanate are sometimes recommended.
Stage II disease: Oral tetracyclines (tetracycline, doxycycline, or minocycline) for several weeks are often used for 8 to 12 weeks or until lesions resolve. If disease persists, clindamycin (300 mg PO bid) with rifampin (600 mg PO daily) has shown promising results. For its antiandrogenic properties, some suggest that an oral contraceptive containing drospirenone or norgestimate with spironolactone may be helpful. Surgery is reserved for cases resistant to medical management.
Stage III or refractory disease of any stage sometimes requires surgical debridement. This must be extensive; simple incision and drainage is not adequate. Postoperative recurrences at previously affected and new sites can occur and close surveillance is indicated. Medical therapies that are potentially helpful in severe or refractory disease include tumor necrosis factor-α inhibitors, interleukin-12/23 inhibitors, oral retinoid, or systemic immunosuppressants or glucocorticoids.
Fox-Fordyce Disease
Fox-Fordyce disease is a rare disease characterized by papular eruption caused by the occlusion of apocrine sweat glands in the axilla and anogenital region. Patients present with flesh-colored or dark dome-shaped papules in clusters that are intensely pruritic, often leading to lichenification. It predominantly affects African Americans. Exacerbations tend to occur before and during menses. Symptoms regress during pregnancy.
Treatment is with oral contraceptives (high estrogen content), topical estrogen ointment (1 mg estrone in peanut oil [Theelin] per ounce of petrolatum), or antiacne topical agents.
Atrophic Vulvovaginitis
The hypoestrogenic state of menopause produces atrophy of the vulvar and vaginal epithelium leading to dryness, pain, burning, pruritus, dyspareunia, and dysuria. The mucosa becomes friable and easily irritated and is more prone to infection. The diagnosis is clinical.
On physical examination, the labia majora appear lax, whereas the labia minora are significantly atrophied. The mucosa is thin, pale, and smooth with loss of the normal rugae of the vagina. Fissures may be present.
Avoid use of harsh soaps and hygiene products. Treatment with estrogen replacement therapy, either topical or oral, helps relieve symptoms.
Contact Dermatitis
Soaps, detergents, hygiene products, vaginal creams, and clothing can all produce a local reaction on the vulva, which may last days to weeks.
On physical examination, symmetric eczematous lesions are seen at the area of contact.
Identify and remove the offending agent. Oatmeal soaks and sitz baths can be used to help control symptoms, and for severe reactions, a mild steroid ointment may be used sparingly.
Psoriasis
Psoriasis typically appears as erythematous plaques with silvery, thick scales. However, the scales are often more difficult to identify on the vulva.
Lichen Simplex Chronicus
Lichen Simplex Chronicus is characterized by intense and persistent pruritus. The rash often involves the perineum.
Continual scratching of the vulva leads to lichenification, producing a thickened, leathery appearance with prominent skin markings and scaling (hyperkeratosis).
Foci of atypical hyperplasia or cancer can develop, with a 3% chance of developing invasive squamous cell carcinoma.
Evaluation should include colposcopy and full-thickness biopsy.
Initial treatment with topical tricyclic/antipruritic ointments (doxepin 5% ointment), antihistamines (hydroxyzine 25 to 50 mg nightly), or an anxiolytic/sedative may relieve pruritus. For more difficult cases, topical corticosteroid preparations covered by continuous dry occlusive gauze dressings (betamethasone valerate ointment 0.1%) or intralesional corticosteroids (triamcinolone 3 mg/mL) are effective.
Lichen Planus
Lichen planus is an uncommon, papulosquamous eruption that can affect the genitalia and oral mucosa. The pathophysiology is thought to involve T-cell autoimmunity to basal keratinocytes.
Patients present with complaints of itching, pain, and burning of the vulva.
White papules in a linear or reticular pattern are often seen on the vulva (Wickham striae).
A wide range of morphologies are seen, the most common and most difficult to treat is the erosive form. When the erosive disease progresses, the vulva and vagina become denuded and scarred with loss of the clitoris and labia minora. Introital stenosis is present in severe disease.
Lichen planus is a chronic recurrent disease; hence, complete control is not typical and spontaneous remission is unlikely. The use of ultrapotent topical steroids is first-line treatment. Surgery is not curative and is reserved for treatment of postinflammatory sequelae, such as labial adhesions and introital stenosis.
Lichen Sclerosus
Lichen sclerosus is of unknown etiology and is characterized by white, wrinkled, atrophic lesions associated with severe vulvar pruritus, atrophy, and scarring, with gradual loss of the labia minora and prepuce of the clitoris. The perirectal area is often involved.
This chronic disease occurs at any age but most commonly affects postmenopausal white women.
Women with lichen sclerosus have a 20% risk of having other autoimmune disease, most frequently alopecia areata, vitiligo, or thyroid disease.
Patients have a 5% chance of developing vulvar squamous cell carcinoma, although lichen sclerosus is usually not considered a premalignant lesion.
Vulvar punch biopsies should be performed to confirm the diagnosis.
Treatment includes chronic use of ultrapotent topical corticosteroid (0.05% clobetasol propionate ointment). Topical estrogen (0.01% estradiol cream) is indicated for atrophic symptoms. Periodic clinical examinations should be performed and patients should return for biopsy if ulcerations persist or new lesions appear. Surgery is reserved for management of malignancy and postinflammatory sequelae, such as labial adhesions and introital stenosis.
VULVAR PAIN SYNDROMES
See also Chapters 30 and 42.
Vulvodynia
Vulvodynia is defined as chronic vulvar discomfort, occurring in the absence of relevant visible findings or a specific identifiable neurologic disorder. The pain is often described as burning, stinging, or throbbing. These symptoms interfere with the ability of women to have vaginal intercourse, wear tight clothing, exercise, or even sit down. Vulvodynia affects roughly 15% of the female population.
Symptoms may be generalized, localized, provoked, unprovoked, or mixed.
The cotton swab test has been described to systematically map affected areas of the vestibule, perineum, and inner thigh for initial evaluation, to differentiate localized from generalized vulvodynia, and to gauge treatment success.
Vulvodynia is a diagnosis of exclusion and thorough evaluation is needed to rule out other pathologies.
Often, a combination of multiple treatments may be required to improve symptoms of vulvodynia.
These include general vulvar care, topical local anesthetics and estrogen creams, oral medications (e.g., tricyclic antidepressants, gabapentin, carbamazepine), trigger point injections with combined steroids and local anesthetics, dietary changes, cognitive behavioral therapy, biofeedback and physical therapy, and surgery for resistant localized pain.
Vulvar Vestibulitis Syndrome
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree