KEY POINTS
• Placental pathology is determined by the dominant physiologic processes of pregnancy, vascular biology, immunology, and development.
• Adverse outcomes and recurrence risks can be explained and subclassified according to the underlying placental pathology.
BACKGROUND
Structure: The placenta is an invasive fetal organ that absorbs nutrients from a reservoir of maternal blood accumulating within its confines in the uterus (1,2):
• Maternal–trophoblastic placenta: Trophoblasts are the only fetally derived cells in direct contact with the mother. Trophoblast is separated into two main types:
• Villous trophoblast: covers the placental villi and mediates gas exchange and transport of nutrients from maternal blood in the intervillous space
• Extravillous trophoblast: infiltrates the uterus and its blood vessels attaching the placenta to the mother (basal plate), allowing maternal blood to enter the intervillous space, and separating the amniotic fluid from the uterus
• Fetal stromal–vascular placenta: Vascularized fetal connective tissue that transmits fetal blood to and from the placenta via the umbilical cord, chorionic plate, and villous trees.
• Placental membranes: Portion of the nonvascularized placenta lying outside the perimeter of the disc, which contains the amniotic fluid.
• Umbilical cord: Tubular structure composed of the major arteries and veins that connect the fetus to the placenta, a surrounding protective extracellular matrix (Wharton jelly), and covered by a surrounding simple squamous epithelium.
• Basal plate
• Uterine implantation: Extravillous trophoblast from the periphery of the blastocyst invades the inner one-third of the uterus and secretes a fibrinoid extracellular matrix that forms the floor of the placenta (known as the basal plate).
• Maternal arterial remodeling: Extravillous trophoblast first migrates upstream within the lumina of maternal spiral arteries, forming plugs that prevent uteroplacental blood flow in early pregnancy. Later, this extravillous trophoblast invades and remodels the spiral artery walls, enhancing perfusion of the placental intervillous space.
• Chorionic plate and villous trees
• Vasculogenesis/angiogenesis: Fetoplacental blood vessels are induced within the extraembryonic endo-/mesoderm by angiogenic factors primarily produced by villous trophoblast. This network of vessels later develops connections with large fetal blood vessels entering the placenta through the body stalk/umbilical cord. Several generations of vascular branching create the roof of the placenta (known as the chorionic plate) and the villous trees, which project downward into the intervillous space. The “trunks and large branches” of the villous tree are known as proximal villi, while the “twigs” are termed distal villi.
• Vasculosyncytial membranes: Specialized areas of close apposition between villous capillaries and trophoblast that form in the early third trimester at the tips of the distal villous tree (terminal villi) facilitating optimal uptake of nutrients.
• Membrane formation
• Regression of peripheral chorion: The placenta is initially spherical, not discoid. When uteroplacental blood flow is initiated by maternal spiral artery remodeling, areas with inadequate perfusion become atrophic (chorion regression), losing their fetal and maternal blood vessels and forming a thin membrane composed of connective tissue (former chorionic plate), chorion laevae trophoblast (remnants of the basal plate and villous tree), and decidua capsularis (underlying endometrium). The remainder of the placenta (chorion frondosum) forms the mature placental disc.
• Amniochorionic fusion: Amnion fuses with the membranous choriodecidual portion of the membranes at about 11 to 12 weeks’ gestation.
• Apposition and fusion with the opposing endometrium: Decidua capsularis fuses with the endometrial lining on the opposite side of the uterus (decidua vera) at about 18 to 19 weeks’ gestation to complete the definitive placental membrane unit.
• Body stalk/umbilical cord
• Vascular remodeling: Two fetal structures enter the primitive body stalk, the allantoic duct projecting from the dome of the bladder and the vitelline duct/yolk sac projecting from the midileum. Each is accompanied by paired veins and arteries. Only the allantoic vessels (one vein and two arteries) persist after embryogenesis in the human placenta.
• Umbilical cord formation: The body stalk becomes sheathed by a skin-like ectodermal covering as the embryo undergoes rostral, caudal, and lateral folding.
• Wharton jelly: A hydrated glycoprotein matrix accumulates around the large vessels in the body stalk/umbilical cord following enclosure by ectoderm.
GUIDELINES FOR SUBMISSION OF PLACENTA FOR PATHOLOGIC EVALUATION
Indications for Submission: College of American Pathologists Practice Guideline (6)
• Developed by a task force of pathologists, obstetricians, and neonatologists.
• Relatively liberal guidelines resulting in submission rate of 40% to 50% in a high-risk setting.
• Yield of significant placental findings with full compliance to guidelines = 64%.
• Indications are separated into three groups as listed below.
Maternal
• Delivery at less than 37 weeks or more than 42 weeks (accepted alternative is less than 34 weeks)
• Systemic disorders with concern for mother or infant (hypertension, diabetes, others)
• Peripartum fever or infection
• Unexplained or excessive third-trimester bleeding
• Unexplained or recurrent pregnancy complications
• Invasive procedures with suspected placental injury
• Thick or viscid meconium
• Severe oligohydramnios/polyhydramnios
Fetal/Neonatal
• Stillbirth or neonatal death
• NICU admission
• Small for gestational age (SGA)/large for gestational age (LGA) (less than 10th or greater than 90th percentile for gestational age)
• Birth depression/pH less than 7.0/Apgar less than 7 at 5 minutes/assisted ventilation greater than 10 min/hematocrit less than 35
• Neonatal seizures
• Suspected infection or sepsis
• Hydrops fetalis
• Multiple pregnancy (accepted alternative is all fused placentas, same sex twins, or discordant fetal growth)
Significant Gross Placental Abnormalities
• Structural abnormalities of the placental disc or membranes
• Suspected abnormal size or weight for gestational age
• Umbilical cord abnormalities (e.g., long/short/hypercoiled/abnormal insertion/single artery)
Placental storage for later submission: Infants may occasionally develop problems within the first few days after leaving the delivery suite. Storing all placentas (fresh refrigerated) for 1 week has been recommended by some to insure that all specimens from pregnancies with adverse outcome are examined.
Ancillary studies: Ancillary studies of placental tissue such as microbiologic culture, karyotype, molecular testing, and electron microscopy are rarely used for placental evaluation. A maternal blood sample for Kleihauer-Betke testing or flow cytometric fetal hemoglobin determination has been recommended in all cases of unexpected adverse outcome.
PLACENTAL PATHOLOGY IN SINGLETON PREGNANCIES (3,4)
Clinical information: The pathologist requires some basic clinical data to properly interpret placental findings. These include the indication(s) for submission, gestational age, maternal gravidity and parity, fetal weight, Apgar scores, and any more specific question that the submitting physician may have.
Gross examination: Placentas can be examined fresh either following refrigeration or after formalin fixation. Abnormalities of color, shape, and umbilical cord insertion site are documented along with any deformations, disruptions, or adherent clots. The trimmed placental disc is weighed and measured, and both the weight and fetoplacental weight ratio are compared with expected values for gestational age. Between three and five histologic sections are usually submitted for histologic analysis including samples of the umbilical cord, membranes and adjacent peripheral placenta, a full-thickness section of parenchyma at the umbilical cord insertion site, and sections of any pathologic lesion with adjacent normal parenchyma.
Selected Gross Abnormalities (See Subsequent Sections for Additional Detail)
• Abnormal shape: reflects reduced maternal perfusion and/or abnormal early fetal vascular branching
• Accessory (“succenturiate”) lobe (placental tissue completely separates from the main disc); bridging vessels can be torn (Fig. 36-1).
• Bilobate/multilobate and over 50% indentation (relatively benign).
• Thick: seen with severe maternal malperfusion and hydrops fetalis.
• Thin: placental atrophy (seen with chronically decreased intervillous perfusion).
• Decreased width (“short chorion”): associated with early marginal hypoxia.
• Abnormal color
• Green: meconium, severe chorioamnionitis, and chronic hemorrhage (biliverdin)
• Brown: chronic hemorrhage (hemosiderin) and stillbirth
• Abnormal weight for gestational age (see Kraus et al. (3) reference for table)
• Decreased: seen with maternal malperfusion, villitis of unknown etiology (VUE), and small fetus
• Increased: seen with diabetic mother, hydrops, and large fetus
• Abnormal cord length (see Kraus et al. (3) reference for table)
• Increased (greater than 70 cm): increased fetal movement and risk of entanglements
• Reduced: decreased fetal movements
• Excessive coiling: increased risk of vascular compromise
• Abnormal cord insertion: can cause acute or chronic fetal perfusion abnormalities
• Membranous: Cord inserts in membranes (risk of torsion/rupture) (Fig. 36-2).
• Furcate: Vessels separate from cord prior to insertion into disc (risk of torsion/rupture).
• Chorionic plate vessel anomalously traveling in membranes (risk of rupture).
• Tethered: Cord covered by a “hood” of amnion (risk of obstructed flow).
• Marginal/peripheral (“battledore”): Cord inserts less than 3 cm from margin (relatively benign).
• Placental mass
• Infarct: obstructed spiral artery (Fig. 36-3)
• Chorangioma: fetal capillary vascular tumor in large stem villus (Fig. 36-4)
• Perivillous fibrin plaque: localized increase in intervillous fibrin (relatively benign)
• Others: entrapped uterine tumors (leiomyoma, stromal nodule)
• Placental hematoma/blood clot
• Retroplacental and central with indentation: abruptio placenta
• Retroplacental and marginal/retromembranous: acute or chronic marginal abruption
• Intraplacental: fetomaternal hemorrhage with surrounding maternal clot
• Large fetal/umbilical vessel: ruptured vasa previa
• Cystic villi
• Septal cysts: intraplacental trophoblastic inclusion cyst (relatively benign)
• Mesenchymal dysplasia: molar villi without trophoblast hyperplasia
• Twin hydatidiform mole: high risk of persistent gestational trophoblastic disease (GTD)
• Partial mole: low risk of persistent GTD
• Trisomy 16: confined placental mosaicism (risk of occult fetal mosaicism)
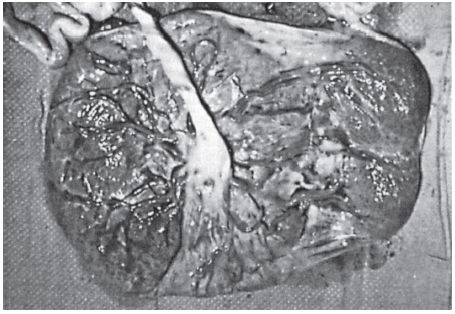
Figure 36-1. Accessory (“succenturiate”) lobe: Fetal vessels bridge membranes separating an island of placental tissue on the right from the main placental disc on the left.

Figure 36-2. Membranous insertion of the umbilical cord: Umbilical vessels separate from the umbilical cord before inserting into the membranes near the placental margin.
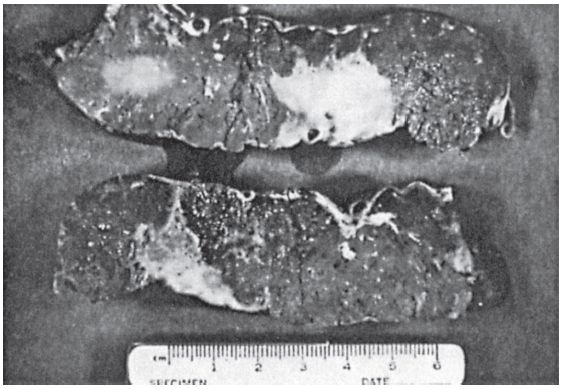
Figure 36-3. Villous infarcts: Firm, pale, granular lesions with their broadest base abutting the maternal surface are seen on cut section of the placenta.
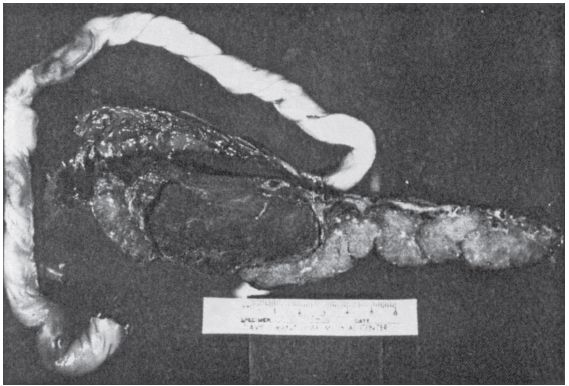
Figure 36-4. Chorangioma: Dark, rounded, smooth lesion incorporating a large chorionic vessel near the fetal surface is seen on cut section of the placenta.
Histologic Lesions (See Figs. 36-5 and 36-6) (2,7)
• Maternal–trophoblastic: Lesions in this category relate to abnormal trophoblast function in the early stages of pregnancy resulting in superficial implantation and damage to maternal arteries that can lead to vascular obstruction and/or rupture. They are most frequent with severe preeclampsia but may also be seen with idiopathic fetal growth restriction (FGR), preterm delivery, maternal obesity, essential hypertension, insulindependent diabetes, renal disease, thrombophilia, and collagen vascular diseases:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


