Diagnostic Approach to Renal Disease
John W. Foreman
CLINICAL PRESENTATION OF RENAL DISEASE
The symptoms and signs of childhood renal disorders vary widely. Diagnostic clues are provided from the history, which should include a description of the amount, frequency, and color of the urine. Changes in any of these may herald a renal disease. The presence of symptoms such as pain on urination (dysuria), urgency (difficulty holding urine in the bladder), incontinence, or dribbling of the urinary stream in boys are also helpful. Pain is not typical of most renal diseases. However, flank pain is common with renal stones and pyelonephritis. Pain from renal stones is excruciating and often radiates from the flank toward the groin. Loin pain may occur with acute glomerulonephritis. Recurrent episodes of dehydration occur in disorders that affect water reabsorption or sodium retention such as tubular disorders, obstructive uropathy, and renal dysplasia. A history of maternal oligohydramnios suggests that in utero renal function was impaired. The family history is sometimes informative, especially in children with heritable kidney disorders such as Alport syndrome, hypercalciuria, cystinosis, and polycystic kidney.
Renal disorders also may present with more insidious symptoms or signs. Chronic renal failure commonly presents with nonspecific symptoms such as fatigue, sleep disturbances, headaches, nausea, and anorexia. Children with severe hypertension (frequently related to renal disorders) can present with seizures and changes in mental status (see Chapter 479). Anemia may occur due to a lack of erythropoietin production by the kidney.
Physical findings of hypertension and edema are common with renal disorders. Periorbital or dependent edema is often an early symptom. The presence of an abdominal mass or genital abnormalities may suggest a renal disease. The kidneys are easily palpated in the first week of life, and renal abnormalities such as multicystic dysplasia, hydronephrosis, and agenesis can be detected by abdominal palpation.
EXAMINATION OF URINE
Urinalysis is one of the most useful procedures in evaluating patients who have suspected renal disease.1 However, some abnormalities on urinalysis are transient; therefore, repeated urinalyses is often useful to avoid more extensive and expensive evaluation.
 COLLECTION OR URINE
COLLECTION OR URINE
The most informative urine to examine is the first morning specimen, as this often is the most concentrated and acidified, and possible increases in urine protein associated with an upright posture will be minimized. Unfortunately, the practical aspects of collecting first-morning urine often delays the time between urine collection and examination. When obtaining a urine culture, the external genitalia should be cleansed, especially in girls, to minimize contamination by extraneous material, such as vaginal cells. The choice of cleansing agent is important. Betadine may interfere with the dipstick reagents, so the usual recommended agent is benzalkonium. Female patients should be instructed to wipe front to back, to spread the labia while voiding, and to collect the urine after some has been passed to minimize bacterial contamination. Sitting backward on a standard toilet is helpful in keeping the labia separated. Males should be instructed to retract the foreskin and clean the glans before voiding. For children unable to void on command, the urine (for urinalysis but not for culture) is obtained by placing an adherent plastic bag over the genitalia. Stroking the paraspinal area (Perez maneuver) can stimulate voiding in a prone infant. Suprapubic bladder puncture and urethral catheterization are the most accurate methods of collecting urine for culture but should almost never be used for routine examination, as either procedure can introduce blood into the urine. Both techniques are low risk in experienced hands. Suprapubic aspiration is used in children under 2 years of age, since the bladder is an abdominal organ in this age group and is easily accessible for puncture. It is best done after a period of time has elapsed from the last void or when percussion, palpation, or ultrasound demonstrates a full bladder. Urethral catheterization, especially in girls, is another relatively sterile way of obtaining urine for culture and is often more successful than suprapubic aspiration. The urine should be examined within 30 to 60 minutes of passage, because a rise in the pH, lysing of red cells, dissolution of casts, and logarithmic increases in bacterial counts occur if the urine is unrefrigerated.
 URINE DIPSTICK TESTING
URINE DIPSTICK TESTING
Dipsticks with small pads containing various reagents that turn a specific color depending on the concentration of the substance analyzed have become a standard part of the routine urinalysis. They can identify blood; and determine the pH; specific gravity; and the concentration of protein, ketones, glucose, nitrite, leukocyte esterase, and urobilinogen in the urine. Test accuracy varies, and all must be interpreted carefully, since they are subject to interference by substances commonly found in urine. Despite these limitations, the low cost and rapid results of urine dipsticks make them useful for screening purposes.
 URINE COLOR
URINE COLOR
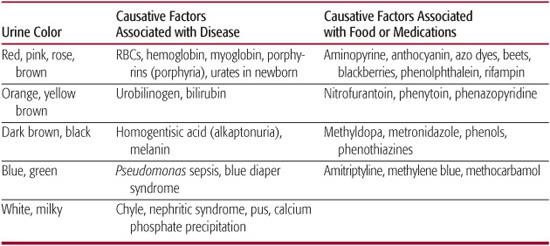
Table 467-1 lists some of the causes of abnormal urine color. The yellow color of normal urine is mainly from urochrome. Urine typically varies in color from nearly colorless to dark amber, depending on the concentration. Other pigments such as carotene, urobilin, and bilirubin can create an orange appearance. White, milky-appearing urine from precipitated calcium-phosphate is seen in normal children, especially if the urine is refrigerated, and is rarely from chyluria. Pinkish sediment in infant urine is common secondary to precipitated urates that may also cause “brick dust” staining of the diaper. Unusual colors often come from dyes or foods but can be associated with pigments excreted in various diseases. Urine in acute glomerulonephritis typically looks like tea and is variously described as rusty to cola-colored (eFig. 467.1  ). With frank hematuria, the urine varies from a light rosé color to grossly red.
). With frank hematuria, the urine varies from a light rosé color to grossly red.
 URINE CONCENTRATION
URINE CONCENTRATION
Specific gravity (the weight of 1 ml of urine compared to 1 ml H2O) can easily be measured and correlates roughly with osmolality, which measures the number of osmotically active particles in the urine. Glycosuria and heavy proteinuria increase the specific gravity out of proportion to the osmolality. The assessment of specific gravity by dipstick is not influenced by glucose or contrast media but is affected by protein. Specific gravity ranges from 1.001 to greater than 1.030. If specific gravity is above 1.030, a nonphysiological substance such as contrast media is likely to be present in the urine. Although urine osmolality is the more precise way of describing urine concentration or dilution, it requires special laboratory testing using an osmometer. In children older than 6 months of age, the urine osmolality (the number of osmotically active particles) varies from 50 to 1200 mOsm/kg H2O.
Table 467-1. Causes of Discolored Urine
 URINE PH
URINE PH
Urine pH varies from 4.5 to 8 and is dependent on the diet (the higher the protein content, the lower the urine pH), the acid-base status of the child, and the time from collection to testing. Acidic urine (pH < 6) is more likely to be observed after an overnight fast than after a meal. Urine pH rises with standing, especially at room temperature. If the urine is alkaline (pH > 6) in a patient with an acid blood pH, an impairment of bicarbonate reclamation or hydrogen ion excretion may be present. The urine pH indicator commonly found on the dipstick gives only an approximation of the true urine pH. More precise measurements using a pH meter are required for the diagnosis of renal tubular acidosis. Collection of fresh urine and transport under paraffin or in a sealed syringe at 4°C is important to ensure accurate measures.
 URINE PROTEIN
URINE PROTEIN
Urine normally contains a small amount of protein (< 100 mg/m2 per day). Forty percent is albumin, 15% are immunoglobulins, and 5% are other plasma proteins. The other 40% is uromodulin (or Tamm-Horsfall protein), which is the cleavage product of a glycosylphosphatidylinositol anchored to the luminal cell surface of the loop of Henle.2 Urine protein is commonly detected by a change in the color of tetrabromophenol blue impregnated on a dipstick pad and is reported as 0 to +4. This reaction is influenced by the urine concentration and pH (markedly alkaline urine will give a false-positive reaction). Chemically measuring the protein in a timed collection of urine, typically over 24 hours, is a more precise way of determining protein excretion but is difficult in young children. The urine protein-to-creatinine ratio can be used to screen for abnormal protein excretion without needing an accurately timed urine collection. Normal children under 2 years of age have a urine protein-to-creatinine (mg/mg) ratio that is less than 0.5, and older children and adults have a ratio that is less than 0.2.3,4 The urine protein-to-creatinine ratio can estimate the 24-hour urine protein excretion (24-hour urine protein excretion = 0.63 × urine protein/urine creatinine [mg/mg]) and is especially useful for following children with proteinuria in whom repetitive 24-hour urine collections are cumbersome.3
Immunochemical methods can detect concentrations of urine albumin (microalbuminuria) below the threshold of standard chemical methods.4,5 Microalbumin excretion rates on an overnight urine sample (normal < 30 μg/min or < 20 mg/g creatinine) have been used to detect early renal disease, especially that associated with diabetes mellitus.
Transient increases in urine protein excretion can be seen with fever, vigorous activity, and extreme cold.6 A positive reaction of +1 or greater is seen in healthy children transiently, especially if the urine is concentrated. Therefore, several urines should be examined for protein to confirm the persistence of proteinuria before an otherwise healthy child is further evaluated.
 URINE GLUCOSE
URINE GLUCOSE
The presence of detectable amounts of glucose in the urine is abnormal except in the premature infant. The standard dipstick method of examining urine for glucose utilizes the glucose oxidase reaction, which is quite specific for glucose and can detect 75 to 125 mg/dL of glucose. 
 URINE NITRITES AND LEUKOCYTE ESTERASE
URINE NITRITES AND LEUKOCYTE ESTERASE
The nitrite test is used to detect bacteriuria (Griess test).6 Typically, nitrate but not nitrite is present in urine. If present in urine, gram-negative organisms reduce nitrate to nitrite but this process takes several hours. Therefore, a negative result does not exclude bacteriuria. A high level of ascorbic acid interferes with a positive reaction. Leukocyte esterase is used to detect pyuria.6 Contamination of the urine from a vaginal discharge will give a positive reaction that is not indicative of a UTI or pyuria. Positive reactions should be confirmed with standard urine microscopy.
 HEMOGLOBIN, MYOGLOBIN, AND RED BLOOD CELLS (RBCS)
HEMOGLOBIN, MYOGLOBIN, AND RED BLOOD CELLS (RBCS)
Hemoglobin and myoglobin will react with the reagents impregnated on the dipstick to form a green to blue color, depending on the concentration. The pad also lyses intact RBCs to allow the intracellular hemoglobin to react with the reagents. The sensitivity of the reaction is reported as being between 5 and 20 RBCs/hpf or 0.015 mg/dL of hemoglobin. Trace reactions are very common and rarely correlated with disease. Positive reactions should be correlated with microscopy. The absence of RBCs on microscopy of the urinary sediment may indicate that the positive reaction is secondary to free hemoglobin or myoglobin but usually simply means that the urinary RBCs have lysed before the microscopic examination.
 URINE MICROSCOPY
URINE MICROSCOPY
Careful microscopic examination of the urinary sediment is quite useful in the diagnosis and management of individuals with renal disease. However, routine microscopic examination of the urinary sediment from healthy individuals with a negative dipstick for blood, leukocyte esterase, and protein is of limited value. 
Red and white cells in the urine may arise from anywhere in the urinary tract. Normal centrifuged urine contains fewer than three RBCs/hpf. Eumorphic red blood cells in urine resemble those in blood films, but in hypotonic urine, RBCs swell and lose their typical biconcave shape. RBCs that are dysmorphic with variations in size and, especially, blebs like “Mickey Mouse ears” on their outer cell membrane suggest a glomerular origin7 (eFig. 467.2  ). Normal urine contains fewer than five WBCs/hpf. Increased numbers of urinary WBCs may indicate infection, but pyuria can also be seen in noninfectious inflammation of both the glomerulus and the interstitium and in nonrenal disorders, including fever and dehydration.
). Normal urine contains fewer than five WBCs/hpf. Increased numbers of urinary WBCs may indicate infection, but pyuria can also be seen in noninfectious inflammation of both the glomerulus and the interstitium and in nonrenal disorders, including fever and dehydration.
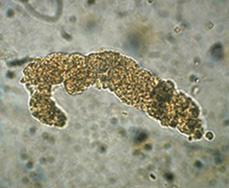
Casts are formed in the tubule and consist of a proteinaceous matrix with or without cells. Hyaline casts are the most common; are nearly transparent; and can be present in normal urine, after exercise, with dehydration, and with proteinuria. Red cell casts (Fig. 467-1) are almost pathognomonic of glomerulonephritis, although they can be seen with renal infarction, renal trauma, and renal vein thrombosis. RBC casts can appear yellow-brown in color rather than red. WBC casts in the setting of a UTI are indicative of pyelonephritis; they are also seen in other causes of interstitial inflammation and can be difficult to distinguish from epithelial cell casts (broad brown casts), which are seen with tubule injury. Granular casts and fatty casts are observed in nephrotic syndrome, and waxy casts are seen in renal failure.
Crystals are commonly observed in urinary sediment and often have little clinical significance. Uric acid can form a variety of shapes, such as diamonds and needles. Calcium oxalate crystals are octahedrons that appear as a square with an X through the center. Triple phosphate or magnesium ammonium phosphate crystals are prisms that have been likened to “coffin lids”; these can be seen in normal urine that is alkaline but are also seen in abundance with urinary tract infection with urea-splitting organisms such as Proteus. Cystine crystals are flat hexagons and are pathognomonic for cystinuria.
Bacteria can be observed in the sediment but are very hard to distinguish from amorphous phosphates and urates without a Gram stain. Urinalysis reports commenting on the number of bacteria per hpf are usually questionable. The diagnosis of a UTI should rest on bacterial culture results and not on the urinalysis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


