Destroyed Femoral Heads
Christopher G. Anton, MD
DIFFERENTIAL DIAGNOSIS
Less Common
Legg-Calvé-Perthes (LCP) Disease
Avascular Necrosis
Septic Arthritis
Juvenile Idiopathic Arthritis (JIA)
Slipped Capital Femoral Epiphysis (SCFE)
Rare but Important
Meyer Dysplasia
Idiopathic Chondrolysis
Epiphyseal Bone Tumors
Epiphyseal Dysplasias
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Age and clinical presentation
Need to exclude infection in child with hip pain and femoral head destruction
Helpful Clues for Less Common Diagnoses
Legg-Calvé-Perthes (LCP) Disease
Avascular necrosis of femoral head of unknown etiology
Age: 3-12 years old, peak 6-8 years old
Bilateral (10-20%)
Radiographs
Normal
Flattening, sclerosis, fragmentation of femoral head ± subchondral fracture (best seen on frog leg lateral view)
Bone scintigraphy: Earlier diagnosis than radiographs with decreased or absent perfusion
MR: Earlier diagnosis than radiographs with decreased perfusion; loss of fatty marrow signal T1WI within femoral head
Initial: Necrosis, vascular invasion, cartilage hypertrophy, overgrowth
Fragmentation: Necrotic/dead bone is resorbed, ± metaphyseal cysts (cartilage) and cartilage hypertrophy
Reparative: Healing and replacement of necrotic/dead bone
Key: Prognosis heavily depends on containment of femoral head
Femoral head grows laterally (extrusion of femoral head) with widening of medial joint space
Incongruency between femoral head and acetabulum
Avascular Necrosis
Most commonly located: Anterolateral weight bearing portion of femoral head but can occur anywhere within femoral head
T2WI: “Double line” sign
Many causes, including sickle cell disease, trauma, steroids, vasculitis, Gaucher disease, hemophilia
Children with acute lymphoblastic leukemia (ALL) and those treated with steroids particularly at risk
Septic Arthritis
Staphylococcus aureus most common
May extend into joint from femoral epiphysis, metaphysis, joint capsule, or acetabulum
Key: Early diagnosis and treatment
Ultrasound: Detect joint effusion (cannot distinguish infected vs. aseptic fluid)
Complications: Cartilage destruction (joint space narrowing), erosions, periosteal reaction, osteonecrosis, and soft tissue abscesses
Juvenile Idiopathic Arthritis (JIA)
a.k.a. juvenile rheumatoid arthritis (JRA)
< 16 years old and symptoms > 6 weeks in duration
Joint space narrowing is a late finding
Slipped Capital Femoral Epiphysis (SCFE)
Femoral head or joint destruction as complication in treatment
Acute or chronic presentations
Salter-Harris 1 femoral physeal fracture
More common in boys
Bilateral in up to 36%
When bilateral, contralateral SCFE usually occurs within 18 months
Age
Girls: 8-15 years old
Boys: 10-17 years old
Predisposition
Complications
Chondrolysis (10%)
Avascular necrosis (1%), increase in open reduction with fixation or pins across superolateral quadrant of femoral head ossification center
Pin penetration
Helpful Clues for Rare Diagnoses
Meyer Dysplasia
Age: 2-4 years old
Mostly boys
Bilateral (60%)
Asymptomatic
When clinical sign or symptoms present, consider early LCP disease
Idiopathic Chondrolysis
Destruction of articular cartilage of femoral head and acetabulum
Stiffness, limp, and pain around hip
Radiographs: Concentrically joint space narrowing, < 3 mm with osteopenia, pelvic tilt
MR: Rectangular hypointense T1 and hyperintense T2 signal abnormality of center 1/3 of femoral head, ± ill defined within acetabulum
Epiphyseal Bone Tumors
Chondroblastoma
1% of primary bone tumors
2nd decade of life, > 90% are seen in patients < 30 years old
M:F = 2:1
Well-defined, eccentric, lucent, sclerotic borders
Calcified matrix (50%)
Giant cell tumor
4-5% of primary bone tumors
Considered benign, but malignant in up to 10% (can metastasize to lungs)
Slight female predominance
After growth plate closure
Epiphyseal Dysplasias
Diastrophic dysplasia
Characteristic: “Hitchhiker thumb”
Cervical platyspondyly and kyphosis, clubfoot
Multiple epiphyseal dysplasia
Ribbing (milder form) or Fairbank forms
Should differentiate from LCP
Bilateral and symmetric changes, short limbs
Spondyloepiphyseal dysplasia
Congenita: Evident at birth; short trunk, mildly short limbs, pear-shaped vertebral body, atlantoaxial instability
Tarda: Presents at age 5-10; short trunks, disc spaces widened anteriorly and narrowed posteriorly, flattening vertebral bodies, dysplastic epiphyses
Image Gallery
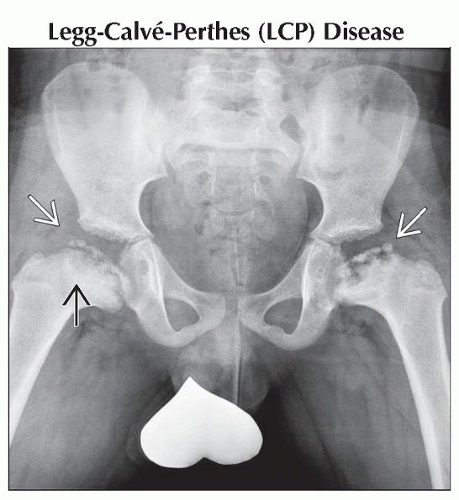 Anteroposterior radiograph shows fragmented, flattened, femoral head ossification centers
 . Notice the metaphyseal cysts (cartilage) . Notice the metaphyseal cysts (cartilage)  and femoral neck widening. and femoral neck widening.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|



