Mechanical Ventilation
INDICATION
The goal of mechanical ventilation, as for any respiratory support, is simply to achieve adequate gas exchange to maintain physiologic neutrality. Mechanical ventilation is indicated when noninvasive forms of respiratory support such as nasal continuous positive airway pressure (NCPAP) are inadequate to support the infant’s respiratory needs. This may manifest as hypoxia, hypercarbia, or apnea. Far less-common indications for mechanical ventilation include airway anomalies and central or pharmacologically induced apnea. Mechanical ventilation of the neonate can seem intimidating to even the most seasoned practitioner. This chapter provides a systematic approach to management of the ventilated neonate, addressing the basic physiology underlying neonatal pulmonary pathology.
In the neonate, the cause of respiratory distress does not change the mode of support to be employed, with the potential exception of air leak syndromes (pneumothorax, pulmonary interstitial emphysema [PIE]). The majority of neonatal patients requiring respiratory support have either an absolute or a functional deficiency of surfactant. Whether treating an infant with respiratory distress syndrome (true surfactant deficiency) or meconium aspiration or pneumonia (surfactant inactivation), we are faced with a lung with decreased compliance and prone to atelectasis.
Conventional, or tidal, ventilation is the most frequently used mode of respiratory support and is addressed in this chapter. Gas is delivered in positive pressure breaths, with exhalation occurring by the lung’s elastic recoil. Simply stated, breath goes in, breath comes out like the tide, hence the term tidal. One can think of conventional ventilation in terms of bulk flow gas exchange.
RESPIRATORY PHYSIOLOGY
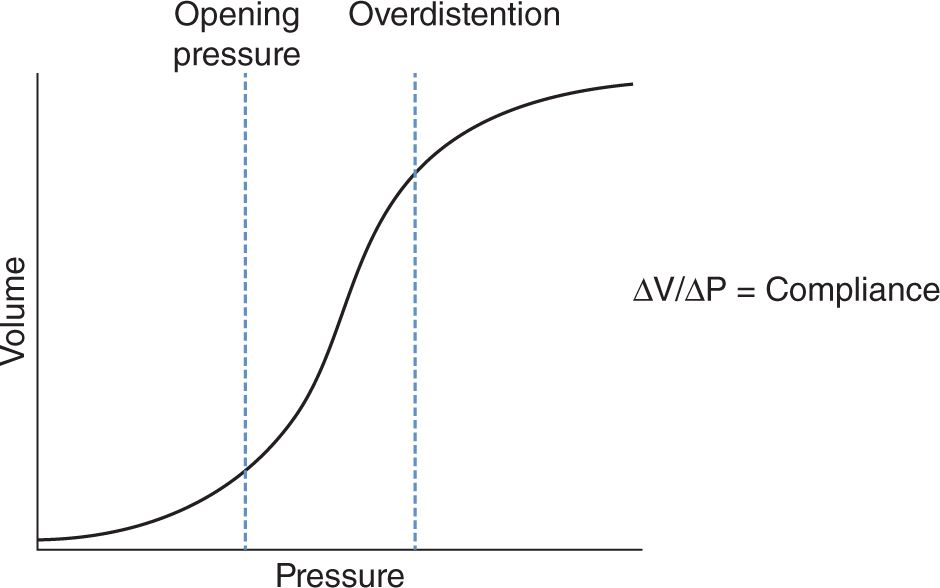
Before proceeding, it is worth simply reviewing the concept of compliance because this guides the decisions we make. The lung as a unit can be thought of as any other elastic spherical structure and will behave as shown in Figure 85-1.
FIGURE 85-1 Pressure/volume curve
Although overly simplistic and not entirely correct, the lung can be thought of as a balloon. Blowing up a balloon is something we all have experienced. There is a certain amount of work that must be done to inflate the balloon; often, the initial inflation is the hardest part of blowing it up. The first inflection point of the curve represents this, and we refer to this point of inflation as “opening pressure.” This point of the curve can also be thought of as our ideal functional residual capacity (FRC), as at this point we exert the minimal amount of pressure to maintain inflation. Maintaining this pressure will ensure that we avoid collapse and minimize work of breathing because at this point in the curve, additional volume can be achieved with little added pressure. The slope of the curve at any point is lung compliance. As you reach the point of overinflation, the balloon becomes relatively inelastic, and with further inflation, you risk rupture. This is represented by the “overdistention” segment of the curve. Here, a good amount of pressure is needed to achieve any additional volume, and in the case of a lung, this is a dangerous place to be.
All of the recommendations made regarding ventilator manipulations assume that we are functioning in the segment of the compliance curve between our opening pressure and overdistention.
METHOD
Getting Started
When placing a patient on a ventilator, a mode must first be selected. There are 3 simple modes to consider, although each ventilator manufacturer has multiple other “hybrid”-type modes available. It is critical for the practitioner to understand the basics of the mode, most notably what triggers a breath, how size of breath is determined (volume or pressure), and what will happen to the ventilator rate should the patient’s respiratory drive change. Other modes not mentioned tend to be some variation of the modes listed. If placing a patient on a mode of ventilation that you are not familiar with, it is essential to take the time with your respiratory therapist to understand exactly what the ventilator is delivering and how it is being triggered to do so. Without understanding this, choosing the proper ventilator change to make is impossible.
1. Intermittent mandatory ventilation (IMV): The ventilator divides a minute by the determined rate to set a cycle time and delivers that breath at the start of each cycle. If there is a set rate of 30, the ventilator delivers a breath every 2 seconds like clockwork (60 seconds/30 = 2). The breath is delivered independent of the infant’s respiratory cycle.
2. Synchronized intermittent mandatory ventilation (SIMV):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree