Methods
We performed a retrospective cohort study that included all singleton pregnancies delivered in the state of California from 2005–2008. The data were derived from linked mother-infant datasets from the California Vital Statistics Birth Certificate Data, infant Vital Statistics Death Certificate Data, California Patient Discharge Data, and Vital Statistics Fetal Death File. Data linkage is performed by the California Office of Statewide Health Planning and Development Healthcare Information Resource Center, under the California Health and Human Services Agency, which used a unique “record linkage number” specific to the mother-infant pair. The state of California maintains these linked datasets that include health information from maternal antepartum and postpartum hospital records for the 9 months before delivery and 1 year after delivery, as well as birth records and all infant admissions that occur within the first year of life. We obtained human subjects approval from the Institutional Review Board at Oregon Health & Science University, the California Office of Statewide Health Planning and Development, and the Committee for the Protection of Human Subjects. The linked dataset did not contain potential patient privacy/identification information, so informed consent was exempted.
Our primary exposure of interest was a diagnosis of SCD in pregnancy. The following International Classification of Diseases, 9th Revision (ICD-9) codes were used: 282.60 (sickle cell disease, unspecified), 282.61 (Hg-S disease), 282.62 (Hg-S with crisis), 282.64 (Hg-S with vaso-occlusive pain). Three hundred forty-four cases were compared with 2,026,979 control pregnancies. Patients with sickle trait and other hemoglobinopathies were excluded, as were deliveries at <24or >42 6/7 weeks of gestation. To avoid the confounding of complications linked to multifetal gestations, we excluded these pregnancies for both the cases and the controls. Analyses were conducted with Stata software (version 12; Stata Corporation, College Station, TX). Outcomes of interest that were examined were also determined retrospectively through the use of ICD-9 codes and included preeclampsia, severe preeclampsia, eclampsia, abruption, IUFD, PTD <37 weeks of gestation, PTD <32 weeks of gestation, SGA, gestational diabetes mellitus, neonatal death, and infant death.
Our analytic approach was first to conduct bivariate analyses of women with and without the exposure of interest for each of the outcomes of interest. Statistical comparisons of categoric variables were made with the use of chi-squared tests. We then conducted multivariable logistic regression models to control for potential confounding. Potential confounders that were assessed included maternal age (≥35 years old and <20 years old), maternal education (>12 years vs ≤12 years), insurance status (private insurance vs public insurance or no insurance), race/ethnicity, parity, diabetes mellitus mellitus, chronic hypertension, and gestational diabetes mellitus. Additionally, we excluded those variables that were used as the outcome of interest when appropriate. For example, we did not adjust for preeclampsia when evaluating preeclampsia as an outcome. Adjusted odds ratios were calculated for all outcomes of interest. Statistical significance was determined by a probability value of <.05 and/or 95% confidence intervals.
Results
A total of 2,027,323 pregnancies met inclusion criteria, among which 344 cases of SCD were identified. Maternal demographic characteristics are shown in Table 1 . The prevalence of SCD was 0.017%. Compared with control subjects, women with SCD were more likely to be African American (76.7% vs 5.1%; P <.001), to be nulliparous (46.2% vs 39.8%; P =.011), to have underlying chronic hypertension (2.3% vs 1.1%; P =.038), and to have limited prenatal care, as defined by <5 visits (7.4% vs 3.8%; P =.001). A trend toward higher rates of public insurance was noted in the SCD group, although this was not statistically significant (53.2% vs 48.4%; P =.07). Maternal educational status and the relative percentages of women aged <20 years or ≥35 years at time of delivery were also similar between groups.
| Characteristic | Sickle cell disease (n=344), n (%) | Control (n=2,026,979), n (%) | P value |
|---|---|---|---|
| Maternal age, y | .08 | ||
| ≤20 | 31 (9.0) | 191,244 (9.4) | |
| 21-34 | 266 (77.3) | 1,485,717 (73.3) | |
| ≥35 | 47 (13.7) | 350,018 (17.3) | |
| Maternal race | <.001 | ||
| African American | 264 (76.7) | 103,359 (5.1) | |
| White | 13 (3.8) | 538,457 (26.6) | |
| Hispanic | 43 (12.5) | 1,102,700 (54.5) | |
| Asian/Pacific Islander | 10 (2.9) | 241,760 (11.9) | |
| Other/unknown | 14 (4.1) | 38,370 (1.9) | |
| Highest education level | .13 | ||
| High school or less | 170 (49.4) | 1,085,946 (53.6) | |
| Some college or graduate degree | 165 (48.0) | 882,097 (43.5) | |
| Unknown | 9 (2.6) | 58,936 (2.9) | |
| Nulliparous | 159 (46.2) | 806,593 (39.8) | .011 |
| Limited prenatal care | 26 (7.4) | 77,392 (3.8) | .011 |
| Public insurance | 183 (53.2) | 981,322 (48.4) | .076 |
| Tobacco use | 7 (2.0) | 13,039 (0.6) | .001 |
| Chronic hypertension | 8 (2.3) | 23,075 (1.1) | .038 |
In univariate analyses, SCD was associated with a statistically significant increase in rates of preeclampsia, PTD, and SGA ( Figure ). Women with SCD had higher rates of both mild preeclampsia (10.2% vs 3.0%; P <.001) and severe preeclampsia (5.4% vs 0.9%); however, no difference in the rates of eclampsia were noted between women with or without SCD (0.0% vs 0.07; P =.62; data not shown). The incidence of PTD at <37 weeks of gestation was nearly 2.5 times higher in women with SCD, as compared with control subjects (25.9% vs 9.8%; P <.001). An even greater difference was seen in the incidence of PTD at <32 weeks of gestation, with rates approximately 6 times higher in the setting of SCD (7.0% vs 1.3%; P <.001). The association between SGA and SCD was significant for all percentile cutoffs that were assessed: <10th percentile (16.2% vs 6.3%; P <.001), <5th percentile (8.4% vs 2.7%; P <.001), and <3rd percentile (5.4% vs 1.6%; P <.001).
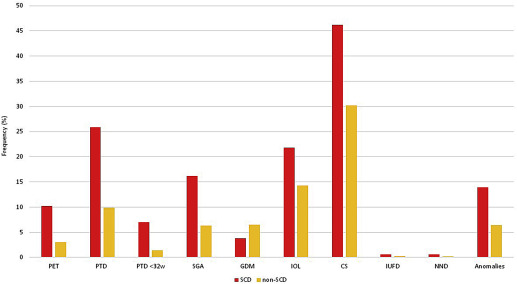
Women with SCD were less likely to have gestational diabetes mellitus, as compared with control subjects (3.8% vs 6.5%; P =.04). They were more likely to require induction of labor (21.8% vs 14.3%; P <.001) and to be delivered by cesarean section (46.2% vs 30.2%; P <.001). Of note, among multiparous women with 1 previous cesarean delivery, the rate of subsequent successful vaginal birth was significantly lower in women with SCD, as compared with control subjects (49.7% vs 70.3%; P <.001; data not shown); however, the rates of attempted trial of labor after previous cesarean delivery in each group were unavailable for analysis.
Women with SCD were significantly more likely to have a pregnancy complicated by a fetal anomaly (14.0% vs 6.4%; P <.001). Specific subsets of major anomalies were examined and demonstrated that the incidence of cardiac malformations, abdominal wall defects, and congenital lung abnormalities were increased significantly among women with SCD ( Table 2 ). However, rates of IUFD and neonatal death were not significantly different between groups. An increased risk of infant death, as defined as death within the first year of life, was noted in the SCD group (1.17% vs 0.33%; P =.007); however, this association was no longer significant after multivariable analysis. Similarly, the increased risks of oligohydramnios and placental abruption in the SCD group did not remain statistically significant after adjustment for potential confounding variables.
| Variable | Sickle cell disease (n=344), % | Control subjects (n=2,026,979), % | P value |
|---|---|---|---|
| Cardiac anomalies | 1.74 | 0.52 | .01 a |
| Abdominal wall defect | 0.58 | 0.06 | .021 a |
| Congenital lung abnormality | 0.58 | 0.05 | .013 a |
| Neural tube defects | 0 | 0.03 | .75 |
| Cleft lip/palate | 0 | 0.13 | 1.00 |
| Hypospadias | 0 | 0.21 | 1.00 |
| Any anomaly | 14.0 | 6.39 | <.001 a |
Multivariable regression analysis results are shown in Table 3 . The increased odds of multiple adverse maternal and neonatal outcomes of interest persisted after adjustment for confounding factors, with the highest adjusted odds ratios seen for severe preeclampsia and PTD <32 weeks of gestation.
| Outcome | Sickle cell disease (n=344), % | Control (n=2,026,979), % | Adjusted odds ratio | 95% Confidence interval |
|---|---|---|---|---|
| Preeclampsia | 10.2 | 3.0 | 2.07 | 1.25–3.42 a |
| Severe preeclampsia | 5.3 | 0.9 | 3.75 | 2.21–6.37 a |
| Placental abruption | 1.7 | 0.9 | 1.66 | 0.74–3.74 |
| Oligohydramnios | 4.4 | 2.6 | 1.36 | 0.79–2.33 |
| Preterm delivery | 25.9 | 9.8 | 2.50 | 1.94–3.21 a |
| Preterm delivery <32 wk | 7.0 | 1.3 | 2.99 | 1.89–4.74 a |
| Small for gestational age | ||||
| <10% | 16.2 | 6.30 | 1.96 | 1.18–3.25 a |
| <5% | 8.4 | 2.7 | 2.00 | 1.33–2.90 a |
| <3% | 5.4 | 1.6 | 1.96 | 1.18–3.25 a |
| Neonatal death | 0.6 | 0.2 | 2.10 | 0.52–8.52 |
| Infant death | 1.2 | 0.3 | 2.21 | 0.82–5.97 |
| Induction of labor | 21.8 | 14.3 | 1.63 | 1.25–2.13 a |
| Cesarean delivery | 46.2 | 31.2 | 1.93 | 1.40–2.67 a |
| Fetal anomalies | 14.0 | 6.4 | 1.73 | 1.26–2.38 a |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


