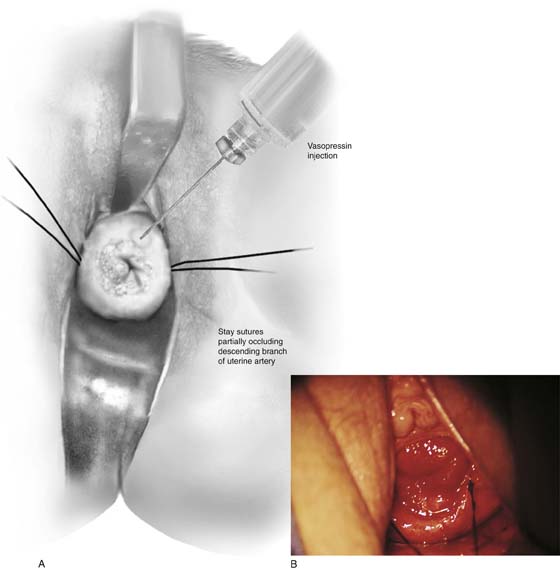
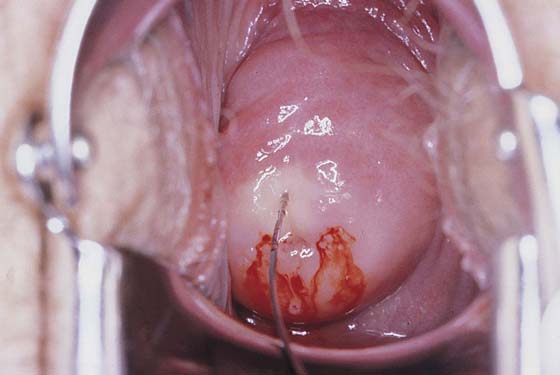
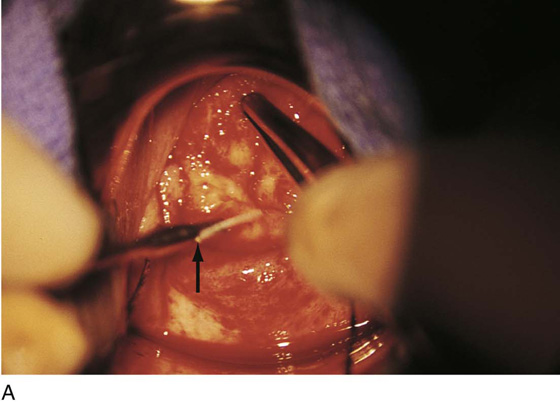
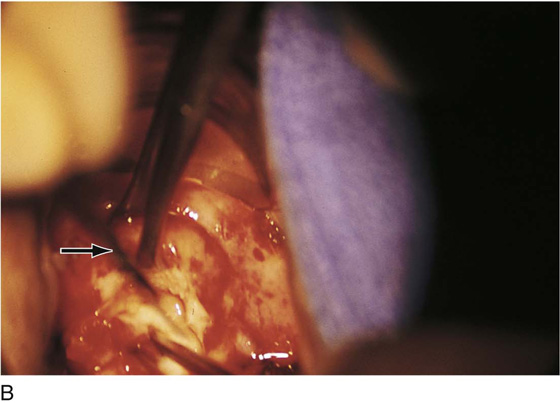
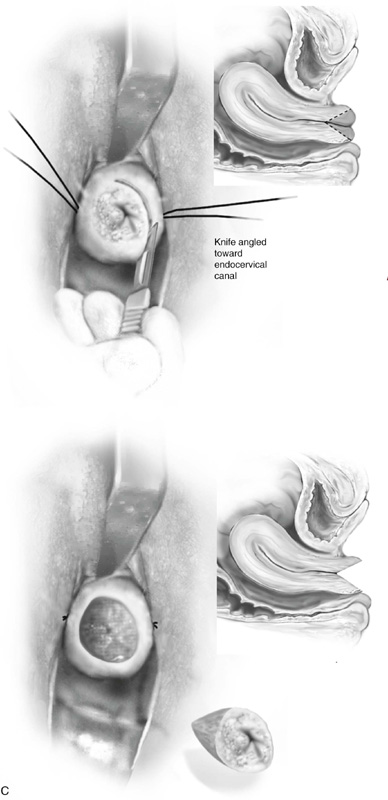
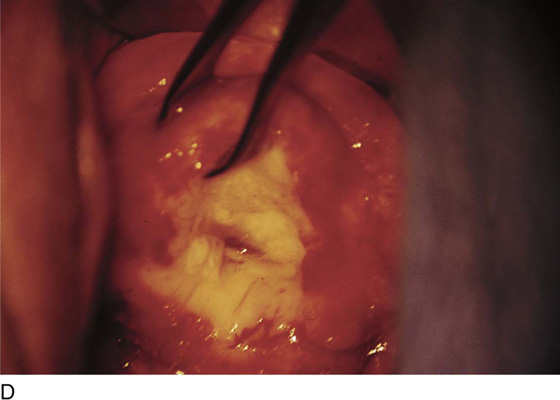
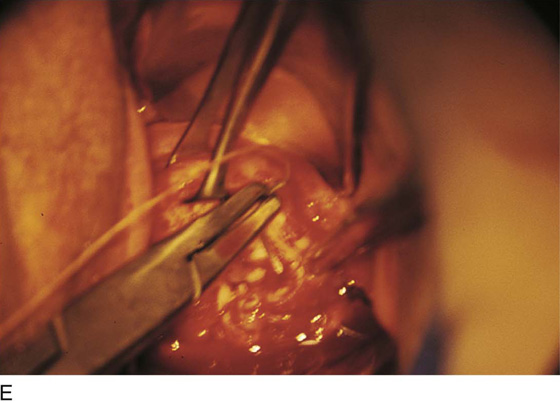
CHAPTER 46 The term cone biopsy has come to refer not only to biopsy of the geometric cone but also to cylinder and disc biopsies (loop excision of the T-zone). Over the past two decades, a great deal of research as well as discussion has focused on the specifications for conization of the cervix. Principally, the goal of the gynecologic surgeon is to obtain a clear (i.e., non-neoplastic) cell margin at the ectocervical, endocervical, lateral, and depth perimeters of the specimen. The strategy is to couple a diagnostic procedure to a therapeutic one. An additional goal of the operation should be maintenance of fertility because most patients who undergo this operation are within the reproductive age group. When performed in the pregnant patient, the procedure should not lead to pregnancy loss. With the exception of adenocarcinoma in situ, which makes up a minority of premalignant neoplastic disorders of the cervix, neoplastic cells spread by direct continuity from the squamocolumnar junction by tracking a course into the endocervical canal or outward onto the portio. The former course is by far more common. Additionally, spread onto the ectocervix is visible by colposcopy, whereas movement into the canal is not. Squamous intraepithelial neoplasia (dysplasia, cervical intraepithelial neoplasia) rarely progresses more than 1 to 1.5 cm up into the endocervical canal. Similarly, when these lesions involve plunging into the endocervical clefts (glands), they penetrate the stroma to a depth of 3 to 3.5 mm and rarely to a depth of up to 6 mm. Thus, the height of the cone should be specified at no more than 15 mm and the peripheral margin around the canal 3 to 3.5 mm. This will encompass and cure 95% of high-grade lesions, including squamous intraepithelial neoplasia stages I (moderate dysplasia) and III (severe dysplasia, carcinoma in situ). An even more conservative approach should be adopted for low-grade squamous neoplasia (mild dysplasia, condylomatous atypia, cervical intraepithelial neoplasia stage I) because its propensity to spread into the canal is less than that of high-grade disorders. Low-grade disease should be excised to a maximal height of 8 to 10 mm with a 3-mm peripheral margin at the transformation zone. On the basis of these facts, several methods can be used to perform a cone biopsy. This chapter does not describe ablative techniques because they do not provide a specimen for the pathologist (the only exception is a description of the unique combination cone). As with other biopsy and therapeutic techniques, use of the colposcope throughout cold-knife conization provides great advantage because the surgeon’s view of the field is magnified, permitting greater precision, the light is excellent and focused onto the field, and the instrument does not take up any space in the operative field. Hemostasis is a key element in the performance of a knife conization. Stay sutures of 0 Vicryl are placed into the cervix at 9 o’clock or 3 o’clock to partially occlude the descending branch of the uterine artery and to provide stabilization of the cervix (Fig. 46–1A, B). The goal is better exposure of the operative field. Injection of vasoconstrictors into the cervical substance provides additional hemostasis (see Fig. 46–1A). The most potent vasoconstrictor is vasopressin, which must be diluted. Vasopressin is supplied as a powder; when mixed with sterile water, this agent contains 20 units per milliliter. An alternative preparation when mixed with sterile water contains 10 units of vasopressin per 0.5 mL (Fig. 46–2). For injection into the cervix, vasopressin should be diluted 1 : 100 (i.e., add 99 mL of diluent to 1 mL of reconstituted vasopressin solution such that each milliliter of the diluted solution will contain 0.2 unit). Typically, 10 mL of the solution is injected into the cervix. If 1% lidocaine without epinephrine is used to dilute the vasopressin, the resultant solution provides vasoconstriction and local anesthesia simultaneously when injected into the cervix (Fig. 46–3). Before injection, however, a colposcopy should be performed, and the peripheral margins of the cone should be marked. Once the vasopressin is injected, the abnormal transformation zone (ATZ) will be difficult to see (Fig. 46–4). The colposcope is set on scanning power. A circular knife cut is made 3 mm peripheral to the AZT. The knife is angled toward the endocervical canal and cuts deeper into the stroma to a height of 1.5 cm. The endocervical margin is cut (Fig. 46–5A through E). Hemostasis is carried out with a ball electrode utilizing spray or forced coagulation at a setting of 50 W. The stay sutures are cut close to the knot (intact), and the field is inspected for hemostasis. No sponges or packs are placed in the vagina or the crater. Performance of endocervical curettage is optional. If the surgeon wishes to curette the remaining endocervical canal, this should be done at the conclusion of the conization but before hemostatic coagulation occurs. FIGURE 46–1 A. Two sutures of 0 Vicryl have been placed into the lateral aspect of the cervix at the 9 o’clock and 3 o’clock locations. These are placed to diminish bleeding and to stabilize the cervix during surgery. B. The stay sutures are pulled downward to better expose the cervix. Even with a deep retractor placed posteriorly, the vagina bulges beneath the posterior cervix. FIGURE 46–2 Vasopressin is diluted such that 1 mL (20 units) is diluted 100-fold. In the case illustrated, each 0.5 mL contains 10 units. Therefore, if 0.5 mL of this solution were mixed with 50 mL of sterile water, the resultant solution would be equivalent. FIGURE 46–3 The vasopressin mixture is injected by using a 10-mL syringe with a 1½-inch, 25-gauge needle attached. FIGURE 46–4 A very superficial needle stick is made into the cervix, and the vasopressin mixture is injected under pressure. As the vasopressin infiltrates, the tissue blanches. FIGURE 46–5 A. The knife cuts into the cervix at 6 o’clock with a margin 3 mm peripheral to the abnormal transformation zone (ATZ) (arrow at knife). B. The knife cut extends deep as traction is placed on the edge of the cut with an Allis clamp (arrow at knife
Conization of the Cervix
Cold-Knife Conization
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree