Fig. 21.1
a and b, Bile-stained vomiting in a newborn with congenital duodenal obstruction
Rarely, the vomiting is non-bilious if the obstruction is proximal to ampulla of Vater.
Features of trisomy 21 (Down’s syndrome).
Milder degree of partial duodenal obstruction as in those with duodenal diaphragm with a hole or duodenal stenosis may be recognized late in infancy or childhood (Fig. 21.2).
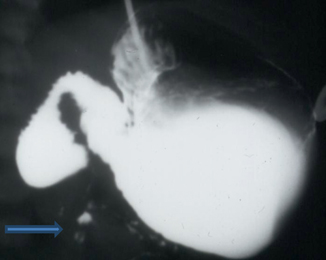
Fig. 21.2
Contrast study showing partial duodenal obstruction (duodenal diaphragm with a central hole). Note the thin contrast seen distally
Examination
Upper abdominal distension or scaphoid abdomen if the stomach is empty or the child is on nasogastric drainage.
Bilious aspirate in the nasogastric tube.
Look for evidence of Down’s syndrome, dehydration, and associated cardiac malformation.
Associated Anomalies
Trisomy 21 (Down’s syndrome) → 28.2 %
Congenital heart disease → 22.6 %
Annular pancreas → 23.1 %
Intestinal malrotation → 19.7 %
Esophageal atresia/tracheoesophageal fistula → 8.5 %
Diagnosis
A plain abdominal X-ray showing double bubble is sufficient to confirm the diagnosis of complete duodenal obstruction (Fig. 21.3). Further contrast studies are not necessary.
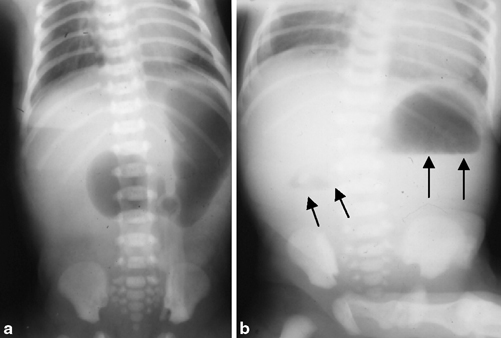
Fig. 21.3
Plain abdominal X-ray showing dilated stomach (a) and double bubble sign (b; arrows) indicative of congenital duodenal obstruction
If the plain abdominal X-ray shows distal bowel gas, the diagnosis is less certain and needs a contrast study especially to rule out the presence of malrotation (refer to algorithm in chapter on intestinal obstruction; Fig. 21.4).

Fig. 21.4
Contrast study showing complete duodenal obstruction. Note the absence of air or contrast distally
The presence of a duodenal diaphragm with a central aperture is confirmed by the incomplete duodenal obstruction in absence of malrotation (Fig. 21.5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


