Fig. 46.1
Diagrammatic representation of the diaphragm showing the different types and sites of hernias
Bochdalek hernia: The most common type of congenital diaphragmatic hernia is a posterolateral (Bochdalek hernia) hernia (Fig. 46.2).
Fig. 46.2
Diagrammatic representation of left Bochdalek hernia
Morgagni’s hernia: The Morgagni defect occurs posterior to the sternum and results from failure of sternal and costal fibers to fuse (Fig. 46.3).
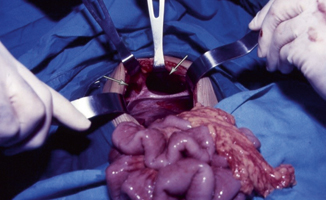
Fig. 46.3
a and b Intraoperative photograph showing bilateral Morgagni’s hernia. Note that the left one is larger than the right
Hiatal hernia: The hiatus hernia occurs through the esophageal hiatus and is divided into three types (Figs. 46.4, 46.5, 46.6, and 46.7):

Fig. 46.4
Barium enema showing the colon herniating through a Morgagni’s hernia. Note the anterior retrosternal position of the hernia

Fig. 46.5
Diagrammatic representation of a paraesophageal and sliding hernia
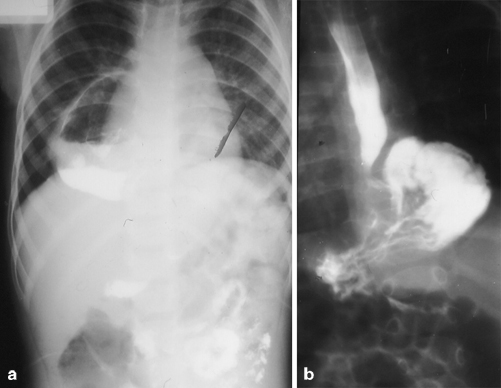
Fig. 46.6
a and b Barium meal showing paraesophageal hernia
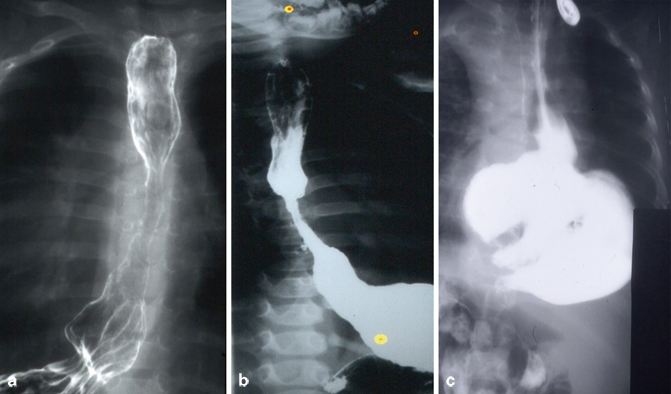
Fig. 46.7
Barium meal showing sliding hiatal hernia in the first tow and combined paraesophageal and sliding hiatal hernia in the third
Sliding
Rolling
Mixed sliding and rolling
Central tendon hernia: This hernia is a rare diaphragm defect involving the central tendinous portion of the diaphragm.
Anterolateral hernia: Occurs anterolaterally through a defect in the muscular part of the diaphragm.
Eventration of diaphragm: There is incomplete mascularization of the diaphragm. This leads to elevation of a portion or all of the intact diaphragm that is thinned as a result of incomplete muscularization (Fig. 46.8).
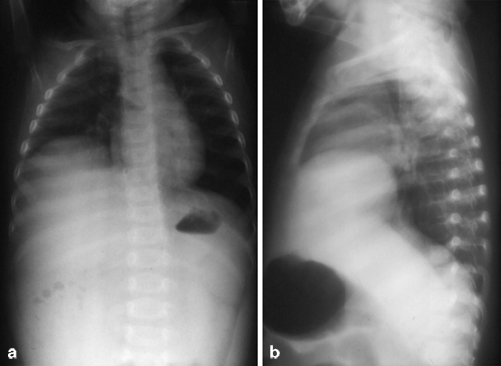
Fig. 46.8
Anteroposterior (a) and lateral (b) chest x-rays showing eventration of right diaphragm
Latrogenic diaphragmatic hernia: Occurs as a result of diaphragmatic injury during surgery.
Traumatic diaphragmatic hernia: Occurs following penetrating and blunt abdominal and thoracic trauma (Fig. 46.9):
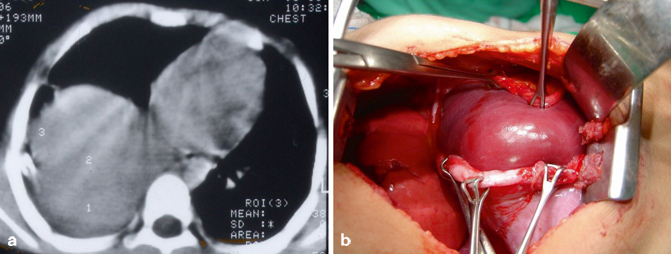
Fig. 46.9
CT-scan of the chest showing traumatic diaphragmatic hernia on the right side with herniation of the liver into the chest and intraoperative photograph showing traumatic rupture of the right diaphragm with herniation of the liver into the chest. Note the extent of the tear in the diaphragm
Congenital diaphragmatic hernia is the commonest of all types of diaphragmatic hernias occurring through a posterolateral defect in the diaphragm and ranging in size from a small defect in the diaphragm to its complete absence (agenesis of diaphragm).
Lazarus Riverius (1589–1655) in 1679 reported the first case of a congenital diaphragmatic hernia in a 24-year-old male following postmortem examination.
In 1946, Gross reported the first successful repair of a neonatal diaphragmatic hernia in the first 24 h of life.
Congenital diaphragmatic hernia occurs in 1 of every 2500–5000 live births.
Congenital diaphragmatic hernia occurs equally in males and females.
Most congenital diaphragmatic hernias occur posterolaterally through the foramen of Bochdaleck.
Approximately 85 % occur on the left side and 15 % occur on the right side.
Bilateral hernias are uncommon and are usually fatal.
The term “posterolateral” diaphragmatic hernia may be a misnomer because, frequently, much larger areas of the diaphragm defects are found and only a posterior rim of muscle can be found (Fig. 46.10).
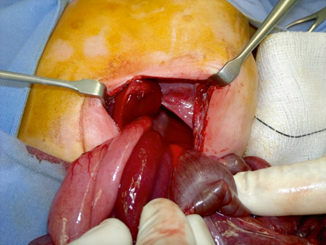
Fig. 46.10
Intraoperative photograph showing a left diaphragmatic hernia. Note the size of the defect which does not correspond to a real posterolateral defect
A hernia sac is present in 10–20 % of congenital diaphragmatic hernias (Fig. 46.11).
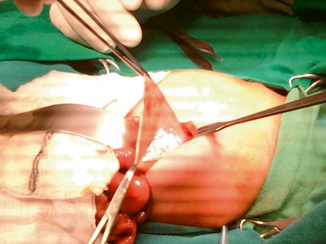
Fig. 46.11
Intraoperative photograph showing a hernia sac in a left congenital diaphragmatic hernia
Over the past 20 years, pulmonary hypertension and pulmonary hypoplasia have been recognized as the two cornerstones of the pathophysiology of congenital diaphragmatic hernia .
Although congenital diaphragmatic hernia is usually a disorder of the newborn period, about 10 % of patients may present after the newborn period and even during adulthood.
Familial congenital diaphragmatic hernia is rare (< 2 % of all cases), and both autosomal recessive and autosomal dominant patterns of inheritance have been reported.
Embryology
The diaphragm is derived from four embryonic structures:
The septum transversum
The pleuroperitoneal membranes
The mesoderm of the body wall
The esophageal mesenchyme
At around 4–5 weeks’ gestation, the septum transversum forms like a semicircular shelf, which separates the heart from the liver.
As the septum transversum develops, it separates the thoracic cavity from the peritoneal cavity but allows pericardioperitoneal canals on either side of the esophagus.
At around the fifth week of gestation, the pleuroperitoneal membranes develop along a line connecting the root of the 12th rib with the tips of the 7th to 12th ribs.
The pleuroperitoneal membranes then grow ventrally and fuse with the septum transversum and the dorsal mesentery of the esophagus.
At 6–7 weeks’ gestation, the pleuroperitoneal canals close; the left side closes after the right.
The left and right crura of the diaphragm develop from the mesentery of the esophagus.
The mesoderm of the body wall forms the outer rim of diaphragmatic muscle.
The posterolateral diaphragmatic hernia results from failure of closure of the pleuroperitoneal canals.
Some intestines and other viscera enter the thorax through this defect and lead to compression of the developing lung at the pseudoglandular stage of lung development. This occurs around the tenth week of gestation.
This will also lead to shift of the mediastinum to the contralateral side. This causes compression of the heart and the contralateral lung as well.
Lung compression results in pulmonary hypoplasia that is most severe on the side of the hernia but both lungs may be affected.
The timing of herniation of bowel into the chest is crucial. The earlier the herniation, the more severe is the pulmonary hypoplasia.
Pathophysiology
As a result of bowel herniation and compression on the developing lungs, both lungs develop abnormally. This is more severe on the affected side and the degree of pulmonary hypoplasia is variable.
The bronchi are less numerous, and the number of alveoli is reduced.
This will lead to a decreased alveolar capillary membrane for gas exchange.
The pulmonary vessels are also affected. The cross-sectional area of the pulmonary vessels is reduced and there is an increase in muscle layer (muscularization) of the pulmonary arteries and arterioles.
This will result in pulmonary hypertension which leads to right-to-left shunts at atrial and ductal levels. This persistent fetal circulation leads to right-sided heart failure. A vicious cycle of progressive hypoxemia, hypercarbia, acidosis, and pulmonary hypertension results.
Infants with congenital diaphragmatic hernias also have impairment of the pulmonary antioxidant enzyme system.
There is also defective development of the surfactant system of the lung.
In very severe cases, left ventricular hypoplasia may develop.
So the pathophysiology of congenital diaphragmatic hernia involves:
Pulmonary hypoplasia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


