Patterns of Congenital Abnormality
The incidence of congenital abnormalities is 10–15 per 1000 births. The commonest are congenital heart defects (8 per 1000) (see Chapter 19). Abnormalities range from a trivial birth mark to a syndrome diagnosis. The majority of congenital abnormalities are genetically determined, but some may be due a combination of genetics and environment (e.g. spina bifida) or due entirely to environment (e.g. fetal alcohol syndrome).
A syndrome is a consistent pattern of dysmorphic features seen together, and suggests a genetic origin. A sequence is where one abnormality leads to another—for example, the small mandible (micrognathia) in Pierre Robin sequence causes posterior displacement of the tongue, which prevents the palate forming correctly, leading to cleft palate. An association is a non-random collection of abnormalities (see below).
Syndromes and Associations
| Syndromes | |
| Down’s syndrome | Trisomy 21: See Chapters 8 and 63 |
| Patau’s syndrome | Trisomy 13 Midline defects, cleft lip and palate, cutis aplasia, holoprosencephaly, polydactyly, heart defects (VSD, PDA, ASD) |
| Edward’s syndrome | Trisomy 18 IUGR, polyhydramnios, rocker-bottom feet, clenched hands, prominent occiput, heart defects (VSD, PDA, ASD), apnoea |
| Turner’s syndrome | (45XO) See chapter 8. |
| Noonan’s syndrome | Phenotypically similar to Turner’s but occurs in both sexes. Short stature, oedema, pulmonary stenosis |
| Associations | |
| VACTERL | Vertebral, anal atresia, cardiac, tracheo-oesophageal fistula, renal, limb (absent radii) |
| CHARGE | Coloboma, heart defects, choanal atresia, retarded growth and development, genital hypoplasia and ear anomalies |
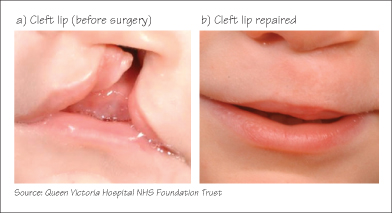
Cleft Lip and Palate
Cleft lip occurs in 1 in 1000 infants. 70% have a cleft lip as well. Cleft lip may be diagnosed antenatally, allowing the parents to receive counselling. After birth a cleft palate is confirmed by palpating and observing the defect in the palate. A submucosal cleft is palpable but not visible. Cleft palate is best managed by a multidisciplinary team including plastic surgeon, orthodontist and speech therapist. Repair of the lip is performed at 3 months and the palate at 9 months. The cosmetic appearance following plastic surgery is excellent. Showing the parents ‘before and after’ photographs (see figure) can help allay anxiety. Expected difficulties include feeding difficulty, milk aspiration, conductive hearing loss and speech and dental problems. Regular audiological assessments are essential.
Neural Tube Defects  (Spina Bifida)
(Spina Bifida)
Failure of the neural tube to close normally in early pregnancy causes spina bifida. It used to be a major cause of disability, but folic acid supplementation in early pregnancy has reduced the incidence by 75%. Antenatal ultrasound screening and selective termination has made open spina bifida a rare condition. Neural tube defects are always midline. The severity depends on the extent to which the neural tube has failed to develop:
- Anencephaly. The cranial part of the neural tube does not exist and the brain cortex does not develop. Infants die soon after birth.
- Myelomeningocele. An open lesion where the spinal cord is covered by a thin membrane of meninges. There is severe weakness of the lower limbs with bladder and anal denervation and an associated hydrocephalus. Survivors have severe disability.
- Meningocele. The spinal cord is intact but there is an exposed sac of meninges which can rupture, with the risk of meningitis.
- Spina bifida occulta. A ‘hidden’ neural tube defect where the vertebral bodies fail to fuse posteriorly. Some degree may be present in 5–10% of normal infants. The only clue may be a tuft of hair, naevus, lipoma or deep sacral pit in the midline over the lower back. A spinal ultrasound is indicated.
 Developmental Dysplasia of the Hip
Developmental Dysplasia of the Hip
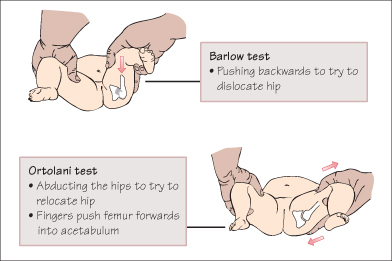
Developmental dysplasia of the hip (DDH) occurs in 1% of infants. The acetabulum is shallow and does not adequately cover the femoral head, leading to the hip joint being, dislocatable or disclocated. Risk factors are breech position, family history, female sex and impaired limb movement. There is an association with talipes. True congenital dislocation of the hip (CDH) occurs in 2 per 1000 infants. Examination includes observation of symmetrical skin creases and leg length, the Ortolani test (a dislocated hip will not abduct fully, and ‘clunks’ as it relocates into the acetabulum) and the Barlow test (feeling a clunk as a dislocatable hip slips out of the acetabulum). Babies with risk factors or abnormal examination should have an ultrasound of the hip joint before 12 weeks. Treatment involves wearing a harness or splint to hold the joint in flexion and abduction for several months.
< div class='tao-gold-member'>



