Chapter 31 Conception control
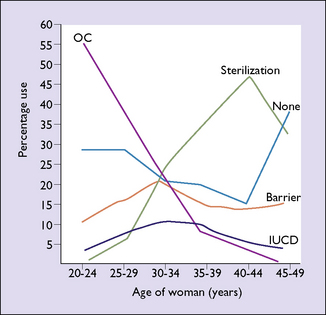
Contraceptive choices now available permit the woman, or the couple, to choose the most appropriate contraceptive for their particular circumstances. Younger women usually prefer oral contraceptives or expect their male partners to use condoms, whereas older women are more inclined to choose the intrauterine device (IUCD) or a permanent method of birth control, such as tubal ligation or a vasectomy in her partner (Fig. 31.1).
The result is expressed as the failure rate per 100 woman years (HWY).
Table 31.1 shows the effectiveness of various contraceptive methods in preventing pregnancy.
Table 31.1 Ranking of contraceptive methods by rate of effectiveness
| Failure Rates per 100 HWY | ||
|---|---|---|
| Group A | Most effective | |
| Tubal ligation/ vasectomyCombined oralContinuous progesterone | 0.005–0.04 | |
| Combined oral | 0.005–0.30 | |
| Continuous progesterone | 0.07 | |
| Group B | Highly effective | |
| IUCD | 0.5–3.5 | |
| Depot progestogen | 1.5–2.3 | |
| Diaphragm or comdom | ||
| All users | 4.0–7.0 | |
| Highly motivated | 1.5–3.0 | |
| Periodic abstinence | ||
| All users | 10.0–30.0 | |
| Highly motivated | 2.5–5.0 | |
| Group C | Less effective | |
| Coitus interruptus | 30.0–40.0 | |
| Vaginal foam or cream | 30.0–40.0 | |
| Group D | Least effective | |
| Postcoital douche | 45.0 | |
| Prolonged breastfeeding | 45.0 |
REVERSIBLE METHODS OF CONTRACEPTION USED BY THE COUPLE
Periodic abstinence
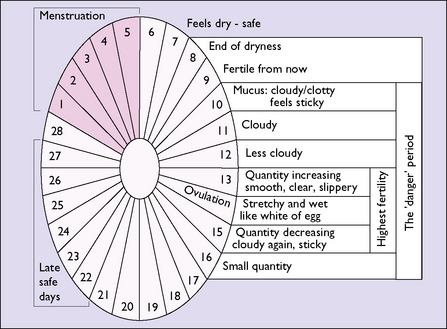
The woman is taught to detect the presence of mucus at the vaginal entrance each morning (before any sexual arousal). Three types of mucus can be detected and, from this, the days on which sexual intercourse can take place can be calculated while to some extent avoiding the chance of an unwanted pregnancy (Fig. 31.2). The compliance of the man is essential if pregnancy is to be avoided.
Coitus interruptus
Withdrawal, or coitus interruptus, is the oldest form of birth control apart from induced abortion. With the development of more modern contraceptives its frequency has declined, but it is still the preferred method in some sections of society. Its reliability for preventing pregnancy depends on the ability of the man to recognize the pre-ejaculatory phase and his agility in withdrawing his penis from the woman’s vagina before ejaculation. Because of these constraints, the efficacy of coitus interruptus in preventing an unwanted pregnancy is rather low (see Table 31.1).
REVERSIBLE METHODS OF CONTRACEPTION USED BY MEN
REVERSIBLE METHODS OF CONTRACEPTION USED BY WOMEN
Women have more choices of reversible or temporary contraception than men. They may choose: