Community-Acquired and Bacterial Pneumonia in Children
Stephen I. Pelton
Worldwide, community-acquired pneumonia is a leading cause of infectious morbidity and mortality in children.1 Studies that employ blood culture, serology, and polymerase chain reaction, as well as those that use pneumococcal conjugate vaccines as a probe to determine the proportion of disease due to Streptococcus pneumoniae, suggest that pneumococcus is the major pathogen in community-acquired pneumonia in children, frequently in the presence of concurrent viral respiratory infection. Several observations such as the presence of patchy perihilar infiltrates on x-ray suggests that most cases of bacterial pneumonia result from aspiration of nasopharyngeal organisms and provide the rationale that respiratory tract flora, nontypeable Haemophilus influenzae, Streptococcus pyogenes, Moraxella catahhralis, Staphylococcus aureus, and S pneumoniae are the major bacterial pathogens in pediatric pneumonia.
 EPIDEMIOLOGY
EPIDEMIOLOGY
Community-acquired pneumonia is most common in infants and toddlers. In children ages 6 months to 5 years, the incidence is 40/1000 patients/year with declining frequency with increasing age.2 Further analysis of the incidence of pneumonia in children < 5 years of age identifies a peak incidence of 52.3/1000 children/year at 2 to 5 years of age with slightly lower incidence rates in children < 24 months.3 Mortality due to community-acquired pneumonia is low—0.1/1000 patients/year in children aged < 15 years. Males are affected almost twice as commonly as females.4 Socioeconomic status and ethnicity affect pneumococcal pneumonia rates, with a greater risk of pneumonia in US children aged < 5 years of Asian, African American, or Hispanic ethnicity compared with those of Caucasian ethnicity.3 Seasonal variations show a greater frequency in the winter and spring months,2,6,7 and during peaks of respiratory syncytial virus (RSV), influenza A, and, in older children, Mycoplasma pneumoniae.2
Lower respiratory tract infections (RTIs) are both more frequent and associated with a greater mortality in developing countries. The incidence among children ages 0 to 5 years from 10 developing countries is estimated to range from 0.2 to 8.1 new episodes/100 child-weeks at risk.9 Mortality from pneumonia has become uncommon in developed countries,4,10,11 yet remains a major cause of death in developing countries.12 In 1990, respiratory infections were the third most common cause of death worldwide; 90 percent of deaths occurred in developing countries.12 Nearly 70% of deaths are in children less than 4 years old.
 MICROBIOLOGICAL ETIOLOGY
MICROBIOLOGICAL ETIOLOGY
Community-Acquired Pneumonia
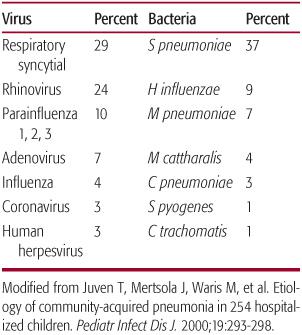
A large spectrum of pathogens have the capacity to cause community-acquired pneumonia in children (Table 240-1). In 20% to 60% of cases, no pathogen is isolated.13,14 Viruses such as respiratory syncytial virus, influenza virus, parainfluenza viruses, and adenovirus are often recovered from the upper or lower respiratory tract, especially in younger children but this does not preclude the presence of a bacterial etiology as well. Blood culture is frequently negative, and sputum or tracheal secretions are rarely obtained in the peak age ranges for pediatric pneumonia. In ambulatory children in both the United States (n = 168)15 and Finland (n = 201),16 viral pathogens were recovered from 28% to 37% of patients < age 4 and less frequently from children ages 5 to 9 (10–21%) or 9 to 16 (0–4%).
Studies of vaccine efficacy have provided important insights into the role of bacterial pathogens in the etiology of pediatric pneumonia. Following universal immunization of infants with the 7-valent pneumococcal conjugate vaccine (PCV), a decline of 40% in ambulatory pneumonia and 50% in hospitalization for pneumonia in children less than 2 years old was reported.8 Klugman and colleagues observed an approximate 40% decline in hospitalized pneumonia associated with influenza, respiratory syncytial virus, and human metapneumovirus pneumonias in South African children immunized with 9-valent PCV compared to controls, providing further support for an expanded role of S pneumonia as a pathogen in a large proportion of cases of pneumonia in children.3,17 Furthermore, experimental serologic methods provide evidence of pneumococcal infection in almost 30% of cases of pneumonia across all age groups, indicating that S pneumoniae plays an etiologic role in many young children with acutely abnormal chest x-rays and clinical symptoms or signs of respiratory tract infections that do not have concurrent bacteremia, empyema, or consolidated lobar pneumonia.15,16
Additional bacterial pathogens are also important causes of pneumonia in children. S pyo-genes is associated with rapid onset of large pleural effusions, prolonged fever, and significant toxicity. H influenzae type b (Hib), prior to the introduction of Hib conjugate vaccine and in countries where Hib vaccination has not been incorporated into national immunization programs, and possibly nontypeable (NTHi) strains, are frequent causes of pneumonia. A substantial role for NTHi is supported by results of lung aspirate studies from the Gambia and Papua New Guinea, where nontypeable strains are recovered from 25% to 53% of children with Haemophilus pneumonia18 (see eTable 240.1  ). Most recently, S aureus, specifically community-acquired methicillin-resistant (CaMRSA) isolates, have reemerged as an important cause of complicated pneumonia. On autopsy these cases frequently demonstrate microabscess and hemorrhage. Cavitation, pleural empyema, pneumatocele, bronchopleural fistula, and/or pyopneumothorax can complicate staphylococcal pneumonia. Karen and colleagues reported S aureus as the most common cause of pleural empyema in children in the decade between 1993 and 2002.19
). Most recently, S aureus, specifically community-acquired methicillin-resistant (CaMRSA) isolates, have reemerged as an important cause of complicated pneumonia. On autopsy these cases frequently demonstrate microabscess and hemorrhage. Cavitation, pleural empyema, pneumatocele, bronchopleural fistula, and/or pyopneumothorax can complicate staphylococcal pneumonia. Karen and colleagues reported S aureus as the most common cause of pleural empyema in children in the decade between 1993 and 2002.19
Table 240–1. Etiology of Childhood Community-Acquired Pneumonia
The atypical/intracellular pathogens, M pneumoniae and Chlamydophila (Chlamydia) pneumoniae, are recognized as important pathogens causing community-acquired pneumonia in children. Studies of children with ambulatory pneumonia identify M pneumoniae infection in 26.5% to 29.5% of cases and of C pneumoniae in 15.0% to 28.5% of cases. These atypical/intracellular pathogens are found most commonly in children aged > 5 years; however, they also occur in younger children as shown by a recent study in which community-acquired pneumonia in children less than age 5 years was due to Mycoplasma pneumonia in 15% of cases, and to Chlamydia pneumoniae in 9% of cases (see eTable 240.2  ).22,23 Data from a recent study did not find the proportion of children infected with M pneumonia or C pneumoniae to be age related.
).22,23 Data from a recent study did not find the proportion of children infected with M pneumonia or C pneumoniae to be age related.
Hospitalized Children
Because hospitalized children are usually younger, have more complicated pneumonia, or are more severely ill, the microbiology in such children differs somewhat from ambulatory patients. The incidence of respiratory syncytial virus and human metapneumovirus is higher in young children, and concurrent infection with pneumococcus appears to be common based on results of studies described earlier.24,25 In children with complicated bacterial pneumonia with necrosis and/or empyema, S pneumoniae and both methicillin-sensitive and methicillin-resistant S aureus are dominant. Other less common bacterial pathogens recovered from hospitalized children with pneumonia include group A β-haemolytic streptococci, H influenzae, and M catarrhalis. Perinatally acquired Chlamydia trachomatis pneumonia, a once common etiology of pneumonia in the first 2 months of life, has been largely eliminated in developed countries through the systematic screening and treatment of pregnant women. Infection with H influenzae type b has been virtually eliminated following immunization with Hib conjugate vaccine in the United States; however, both C trachomatis (in infants) and H influenzae type b may still be significant pathogens in developing countries.26,27 Mycobacterium tuberculosis may also present as an acute pneumonia with fever, respiratory signs, and alveolar infiltrate with or without pleural effusion. Tuberculosis should be considered in children who recently immigrated to the United States, those returning to travel from countries with endemic tuberculosis, and those who have had contact with recently diagnosed individuals. Skin testing for tuberculosis should be a routine part of evaluation of children with pneumonia.
 CLINICAL PRESENTATION
CLINICAL PRESENTATION
Clinical signs and symptoms of bacterial pneumonia overlap with many aspects of viral pneumonia preventing clear discrimination between the two. Fever, frequently greater than 102°F, ill appearance, and respiratory and/or abdominal signs are found in the majority of patients with both RSV pneumonia and pneumococcal pneumonia (see eTable 240.3  ).28 Tachypnea and rales/crackles are reported in 40% to 50% of patients.29 Bacteremic pneumonia is more frequently associated with greater severity of clinical signs and symptoms such as higher fever.
).28 Tachypnea and rales/crackles are reported in 40% to 50% of patients.29 Bacteremic pneumonia is more frequently associated with greater severity of clinical signs and symptoms such as higher fever.
 RADIOLOGICAL EXAMINATION
RADIOLOGICAL EXAMINATION
Chest x-ray is often used to confirm the presence of pulmonary infiltrates/consolidation in patients with suspected pneumonia. In some studies, the presence of infiltrates was part of the definition of pneumonia.1 Several studies suggest that the presence of alveolar infiltrates is an insensitive but reasonably specific indicator of bacterial infection.28,29 More recent studies find no significant correlation between the radiological picture and the etiological agent—ie, it was not possible from the chest x-ray to conclude whether the child had viral infection, bacterial infection, or mixed infection—but rather a correlation between age and radiographic findings (see eTable 240.4  ).30
).30
Some findings on x-ray are useful for the diagnosis of bacterial pneumonia. The presence of necrotizing pneumonia (pneumatocele, loculated empyema, and/or necrotic lung tissue) are virtually diagnostic of pneumococcal or staphylococcal disease. Studies from 1990 through 2000 indicated that S pneumoniae was the more common etiology in cases with complicated pneumonia but recently the incidence of disease due to S aureus has increased.19
 LABORATORY TESTING
LABORATORY TESTING
Determination of the specific pathogen is challenging in children because bacteremia is uncommon, pleural effusion is present in only a small percentage of children, antimicrobial therapy has often been administered prior to collection of fluid, nasopharyngeal cultures are not necessarily representative of lower respiratory tract secretions, and the vast majority of children do not produce sputum.31 More aggressive procedures, such as lung puncture and bronchoalveolar lavage, may be diagnostic but are generally reserved for hospitalized patients with significant respiratory distress. Blood tests including total and differential white cell count, erythrocyte sedimentation rate, C-reactive protein, and procalcitonin weakly correlate with etiology and have poor sensitivity and specificity.32,33 Serological tests for S pneumoniae, M pneumoniae, and C pneumoniae are generally not useful in the clinical setting due to only moderate specificity, widely varied sensitivity, and a lack of standardization. Furthermore, these tests require comparison of acute and convalescent serum.34,35 Polymerase chain reaction tests for S pneumoniae, M pneumoniae, and C pneumoniae may be useful for detecting causality in non-bacteremic pneumonia in children but further evaluation of sensitivity, specificity, and reproducibility is needed.38
SPECIAL POPULATIONS
 CHILDREN WITH ASTHMA
CHILDREN WITH ASTHMA
A link between respiratory tract infections and asthma in children is well established. It has been suggested that the majority of asthma exacerbations in children are associated with viral or atypical/intracellular pathogens such as C pneumoniae and M pneumoniae.39C pneumoniae has been isolated more frequently from children with wheezing compared to controls (11.0% vs 4.9%). In addition, 9 of 12 (75.0%) children with wheezing and evidence of C pneumoniae showed clinical and laboratory improvement of the reactive airways disease after eradication of chlamydial infection with erythromycin or clarithromycin. C pneumoniae and M pneumoniae infections have also been detected more frequently in children with wheezing than in control subjects. Furthermore, a history of recurrent wheezing is more common in children with C pneumoniae or M pneumoniae infections than in those without either infection.40,41 Some investigators estimate that these organisms may trigger 5% to 30% of wheezing episodes and asthma exacerbations but further confirmation is required.
 CHILDREN WITH SICKLE CELL DISEASE
CHILDREN WITH SICKLE CELL DISEASE
Acute chest syndrome (ACS) is a common cause of hospitalization and is associated with substantial morbidity in patients with sickle cell disease (SCD) (see also Chapter 434). Recent reports indicate that pneumonia may be a common cause of ACS in children with SCD. The report from a 30-center study demonstrated that infection—especially community-acquired pneumonia—is a common cause of ACS.42 In this study, 27 different infectious pathogens as well as pulmonary fat embolism were identified as causes; C pneumoniae and M pneumoniae were the most prevalent. Infection was considered a contributing factor in 56% of deaths. The prevalence of pneumonia in children with SCD is significantly higher. By age 4, children with SCD have a 4 times greater risk of bacterial pneumonia than that of age- and sex-matched controls with normal hemoglobin genotype.43 Pneumonia in children with SCD also has a more serious clinical course compared to otherwise healthy children.44M pneumoniae and C pneumoniae appear to be common organisms involved in pneumonia and ACS associated with SCD, though other potential bacterial pathogens include S pneumoniae, S aureus, and H influenzae.45 These findings support the selection of antibiotics with activity against atypical/intracellular pathogens when selecting suitable antibacterial coverage for patients with severe ACS.
 TREATMENT
TREATMENT
Current Recommendations for Therapy
Controversy about whether to treat all children with pneumonia with antimicrobial therapy or to limit therapy to those with moderate or severe clinical symptoms and signs remains unresolved, and no official US guideline has been proposed. Because a microbiologic diagnosis is not commonly established, the selection of initial antibacterial therapy is primarily empirical. Most children with community-acquired pneumonia can be treated with oral antimicrobial agents. The treatment choice is based on age, clinical severity, and epidemiological factors. Therapy for community-acquired pneumonia should always include antibiotics against S pneumoniae, which is a common bacterial pathogen even when virus has been recovered from the respiratory tract. The British Thoracic Society has proposed guidelines for treatment that support withholding of antimicrobial therapy in young children presenting with mild symptoms of lower respiratory tract infection but do not specifically address the question of whether to treat all children diagnosed with pneumonia.14 Amoxicillin is the first choice for oral antibiotic therapy in children less than 5 years old (Table 240-2). Because β-lactam antibiotics are not active against atypical pathogens, macrolides are often recommended for children aged > 5 years or whenever infection with atypical/intracellular pathogens is suspected.31 The British Thoracic Society guidelines recommend management in the hospital for children with evidence of more severe disease (Table 240-3). In children hospitalized with severe community-acquired pneumonia, initial therapy must include coverage for S pneumoniae, including multidrug-resistant strains in the community and community-acquired methicillin-resistant S aureus (CaMRSA), especially when complicated pneumonia is present (see Chapter 284).
Table 240–2. Management of Community-Acquired Pneumonia in Children



