Main classes
Subclasses
Class I
Hypoplasia/Agenesis
(a) Vaginal
(b) Cervical
(c) Fundal
(d) Tubal
Class II
Unicornuate
(a) Communicating horn
(b) Non-communicating horn
(c) No cavity
(d) No horn
Class III
Didelphys
Class IV
Bicornuate
(a) Complete
(b) Partial
Class V
Septate
(a) Complete
(b) Partial
Class VI
Arcuate
Class VII
DES Drug related
However, it is a reality that this system is associated with the following very serious disadvantages: (1) there are reported anomalies that could not be classified with the AFS system; (2) the definitions of the system’s categories are not clear raising serious problems in the differential diagnosis between the different classes, with the more obvious one that of defining the “margins” between arcuate and partial septate; (3) class I of the AFS system seems to be a “potpourri” of patients with different clinical presentations of varying severity, including mainly cases of complex anomalies often needing difficult surgical treatment, and their ineffective categorization consists a great problem for their management and, (4) obstructive anomalies are not clearly represented in the AFS system placing them in the potpourri of the first class or in other classes of the system but without any clear distinction [16].
It seems, therefore, that the AFS classification system “could function as a framework for the description of anomalies rather than an exhaustive list of all possible anomaly types” [16, 30].
The Embryological-Clinical Classification
The embryological origin of the different elements of the genitourinary tract is selected as the basis for the development of this system [1, 2] (Table 4.2). The embryological-clinical classification has the theoretical advantage that it is closely related to the pathogenesis of the anomaly enhancing the explanation and understanding of the resulting anatomical status of the female genital organs. It has also the potential advantage that it might be more effective at classifying complex anomalies, a hypothesis that needs to be tested.
Class | Embryological defect | Clinical presentation |
|---|---|---|
1 | Agenesis or hypoplasia of a urogenital ridge | Unicornuate uterus with uterine, tubal, ovarian, and renal agenesis on the contralateral side |
2 | Mesonephric anomalies with an absence of the Wolffian duct opening to the urogenital sinus and ureteral bud sprouting (and, therefore, renal agenesis). The “inductor” function of the Wolffian duct on the Mullerian duct also fails, and there is usually uterovaginal duplicity plus blind hemivagina ipsilateral with renal agenesis | (a) Large unilateral hematocolpos |
(b) Gardner’s pseudocyst on the anterolateral wall of the vagina | ||
(c) Partial reabsorption of the intervaginal septum, seen as a “buttonhole” on the anterolateral wall of the normal vagina, which allows access to the genital organs on the renal agenesis side | ||
(d) Vaginal or complete cervico-vaginal unilateral agenesis, ipsilateral with renal agenesis, and with [1] no communication or [2] communication between both hemiuteri (communicating uteri) | ||
3 | Isolated Mullerian anomalies affecting | |
(a) Mullerian ducts | The common uterine malformations as unicornuate (generally with uterine rudimentary horn), bicornuate, septate, and didelphys uterus | |
(b) Mullerian tubercle | Cervico-vaginal atresia and segmentary anomalies, such as transverse vaginal septum | |
(c) Both Mullerian tubercle and ducts | Mayer-Rokitansky-Kuster-Hauser (uni- or bilateral) syndrome | |
4 | Anomalies of the urogenital sinus | Cloacal anomalies and others |
5 | Malformation combinations | Wolffian, Mullerian, and cloacal anomalies |
However, this system has not received wide acceptance. This seems to be due to the following reasons: (1) female genital anomalies are by definition deviations from normal anatomy and clinicians difficultly accept the shift from anatomy to embryogenesis, (2) it is quite complex classifying not only anomalies of the female genital tract by of the genitourinary tract in general which is not the requested issue for gynecologists, (3) patients’ clinical presentation, prognosis and treatment are closely related to the anatomical status and, it seems to be more functional to design the classes of a system on that basis and (4) most therapeutic interventions tend to restore anatomical deviations from the norm emphasizing the need to use anatomy per se as the basis of the system [16].
On the other hand, the contribution of this system and of its inventors to the better understanding of the pathophysiology of female genitourinary malformations could not be ignored representing a step forward in their interpretation. As a general statement, the embryological-clinical classification system could, probably, better explain pathogenesis of congenital malformation but it could not act as a functional framework for the description and treatment of the anomalies.
The VCUAM Classification System
The basic characteristic selected for the design of this proposal is also the anatomy of the female genital tract [25] (Table 4.3). However, the new and important element in the design of this system is the independent classification of each organ of the female genital tract and of the associated malformations according to the TNM classification for breast cancer. This approach has the theoretical potential of classifying the anomalies in a detailed, representative and precise way; each anomaly, even the more complex, could be theoretically described giving the clinician an accurate description of female genital tract anatomy.
Table 4.3
The Vagina Cervix Uterus Adnexa and associated Malformations (VCUAM) classification system [25]
Vagina (V) | 0 | Normal | Uterus (U) | 0 | Normal |
1 | (a) Partial hymenal atresia | 1 | (a) Arcuate | ||
(b) Complete hymenal atresia | (b) Septate <50 % uterine cavity | ||||
(c) Septate >50 % uterine cavity | |||||
2 | (a) Incomplete septate vagina <50 % | 2 | Bicornuate | ||
(b) Complete septate vagina | |||||
3 | Stenosis of the introitus | 3 | Hypoplastic | ||
4 | Hypoplasia | 4 | (a) Unilaterally rudimentary or aplastic | ||
5 | (a) Unilateral atresia | (b) Bilaterally rudimentary or aplastic | |||
(b) Complete atresia | |||||
S | 1. Sinus urogenitalis (deep confluence) | + | Other | ||
2. Sinus urogenitalis (middle confluence) | |||||
3. Sinus urogenitalis (high confluence) | |||||
C | Cloacae | # | Unknown | ||
+ | Other | ||||
# | Unknown | ||||
Cervix (C) | 0 | Normal | Adnexa (A) | 0 | Normal |
1 | Duplex cervix | 1 | (a) Unilateral tubal malformation, ovaries normal | ||
(b) Bilateral tubal malformation, ovaries normal | |||||
2 | (a) Unilateral atresia/aplasia | 2 | (a) Unilateral hypoplasia/gonadal streak | ||
(b) Bilateral hypoplasia/gonadal streak | |||||
(b) Bilateral atresia/aplasia | |||||
+ | Other | 3 | (a) Unilateral aplasia | ||
(b) Bilateral aplasia | |||||
# | Unknown | + | Other | ||
# | Unknown | ||||
Associated malformations (M) | 0 | None | |||
R | Renal | ||||
S | Skeleton | ||||
C | Cardiac | ||||
N | Neurologic | ||||
+ | Other | ||||
# | Unknown | ||||
However, the inventors of this system, focusing mainly in its design ignored the need to discuss in details and define the groups for each separate organ, which is extremely important for the users and the accuracy of each classification system. Furthermore, each anomaly has the same independent importance in the classification of the patients; frequency is not taken into account and extremely frequent uterine anomalies e.g. septum have the same importance as the rare ones e.g. cervical aplasia [16]. Hence, it seems that there is a non-functional overestimation of the anatomy. Moreover, patients could only be classified with the use of the system’s tables and, reversely, description of the patient’ clinical condition (e.g. “V5b, C2b, U4b, A0, MR”, which is a patient with Mayer-Rokitansky-Kuster-Hauser syndrome) could not be done without the use of those tables.
Thus, it seems that the main restriction for the acceptance of the VCUAM system is that it is not simple and user’s friendly. Thus, “although the VCUAM classification system may serve as an exhaustive list of all possible anomalies, it could not easily serve as a functional framework for describing the anomalies” [16].
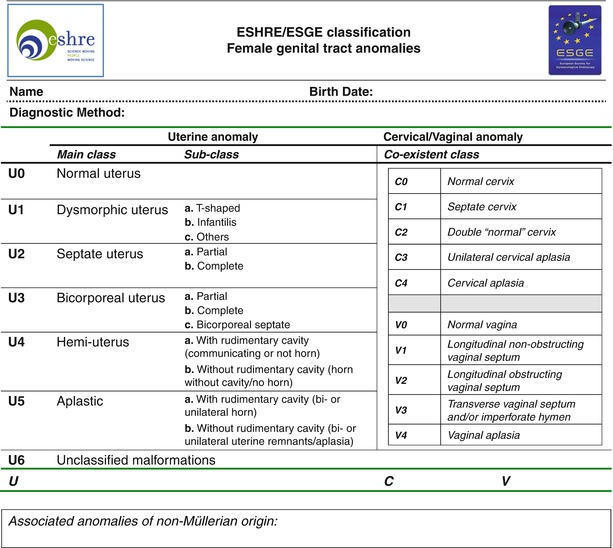
The ESHRE/ESGE Classification System
The European Society of Human Reproduction and Embryology (ESHRE) and the European Society for Gynecological Endoscopy (ESGE), has recently published the new ESHRE/ESGE classification system of female genital tract congenital anomalies [18, 19] (Fig. 4.1). This was the result of an effort based on the preparatory scientific work done within the European Academy for Gynecological Surgery (EAGS), which was adopted by the CONUTA (CONgenital Uterine Anomalies) common ESHRE/ESGE Working Group [16, 17]. The development of the new system was done using DEPLHI procedure for consensus assessment [13, 23, 35]; based on the results of the DELPHI procedure, consensus development by the CONUTA Scientific Committee was followed [18, 19].