Chronic Lung Disease
DIAGNOSIS AND INDICATION
Clinical Findings
History
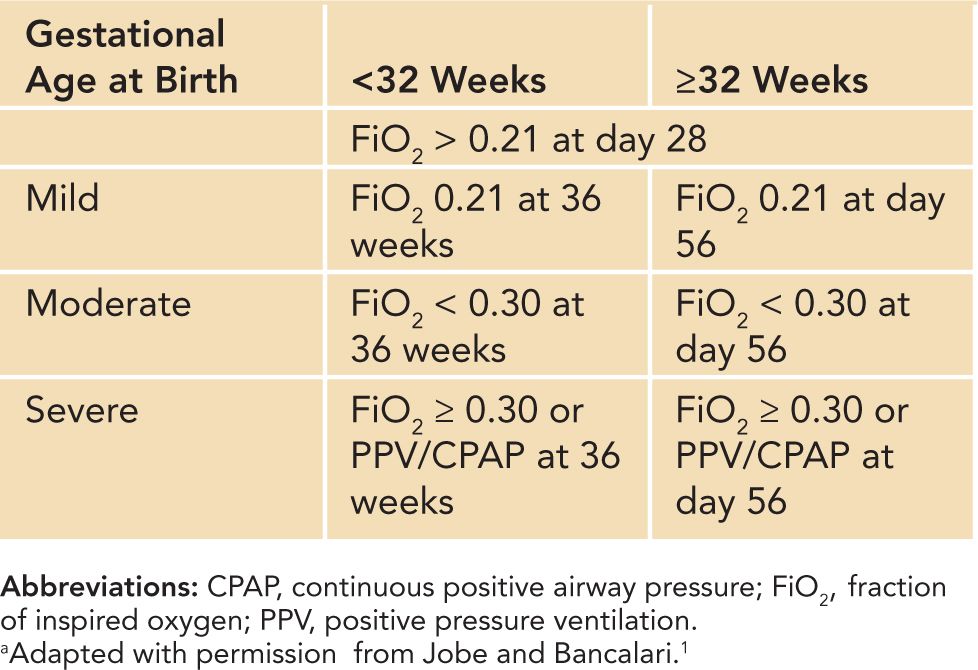
The definition of bronchopulmonary dysplasia (BPD) has been modified over the years. The initial description by Northway et al was followed by a definition of BPD that required a history of positive pressure ventilation during the first 2 weeks of life, clinical signs of respiratory compromise, and requirement for supplemental oxygen beyond 28 days of age, in addition to characteristic radiologic abnormalities. The current definition of chronic lung disease (CLD) in the newborn distinguishes between mild, moderate, and severe disease and uses O2 dependency at 36 weeks’ postconceptual age, thereby “correcting” for the degree of immaturity (Table 86-1). The disease is characterized by alveolar arrest and impaired vascular development, which is more significant at lower gestational ages.
Table 86-1 Degrees of Bronchopulmonary Dysplasiaa
Physical
Clinical signs of CLD include evidence of respiratory distress, such as tachypnea, nasal flaring, and use of accessory muscles with intercostal and substernal retractions, grunting, and cyanosis. The decrease in gas exchange surface area leads to impaired gas exchange (ie, hypoxemia with need for supplemental O2 and alveolar hypoventilation with resultant hypercapnia) as a result of ventilation and perfusion mismatch. The clinical picture can be complicated by increased pulmonary vascular resistance, typically characterized by impaired responsiveness to inhaled nitric oxide (iNO) and other vasodilators, sometimes progressing to pulmonary hypertension and right heart failure. Biventricular failure is unusual when sufficient oxygenation is maintained, and the development of severe pulmonary hypertension is avoided. Pulmonary function testing in these infants often demonstrates increased airway resistance, hyperreactive airways, and reduced compliance. Infants can present with episodic bronchoconstriction and cyanosis. Increased work of breathing contributes to impaired somatic growth and neurologic development observed in severe cases from an early stage.
Confirmation/Baseline Tests
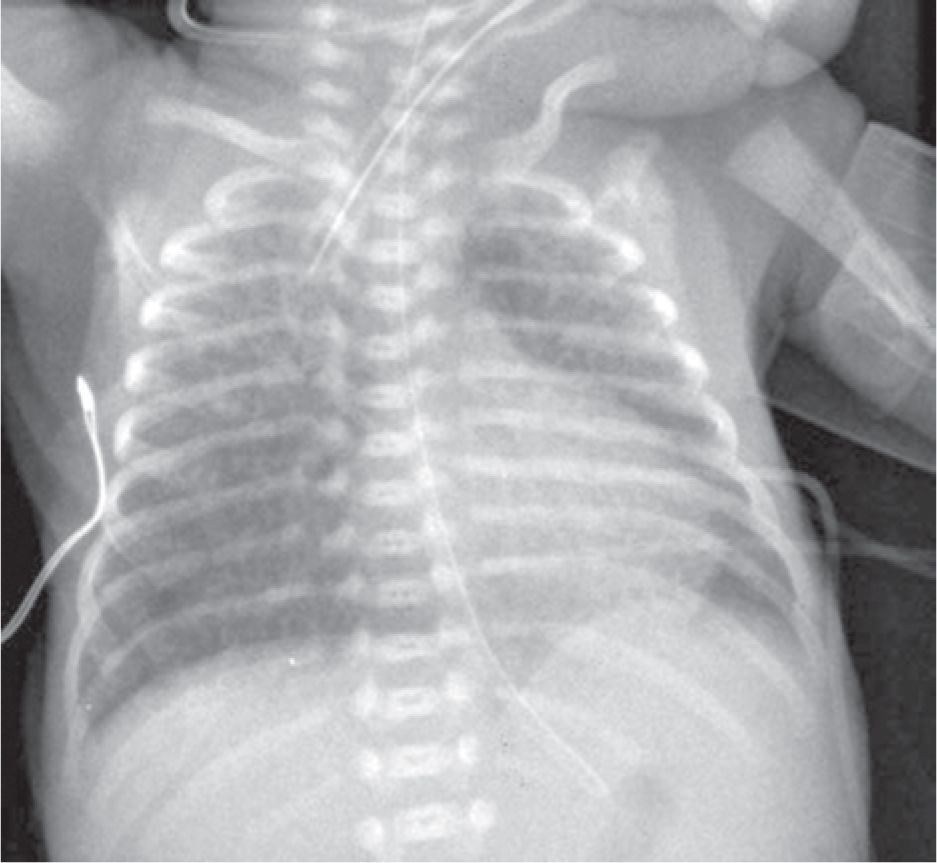
The diagnosis is defined by the need for supplemental oxygen or ventilator support to maintain oxygen saturation above 85% at 36 weeks’ postconceptual age. Blood gas analysis shows an increase in bicarbonate and partial pressure of carbon dioxide (pCO2), indicating increased ventilation-perfusion mismatch. Continuous pulse oximetry is needed to monitor oxygen saturation and control oxygen supply. Chest radiographic findings include fibrosis/interstitial markings, cystic elements, and hyperinflation starting in the first week of life, with severely affected infants showing cystic changes (Figure 86-1). High-resolution computed tomography (HRCT) demonstrates linear and reticular opacities, areas of architectural distortion, and gas trapping or hyperexpansion. Increased pulmonary vascular resistance can be tested by echocardiography or by right heart catheterization when insufficiency of the tricuspid valve is present. Severe cases can present with cor pulmonale and right heart failure.
FIGURE 86-1 Anterior posterior chest x-ray with a score of 5; 4 for interstitial shadows in all 4 quadrants, 1 for lung expansion, and 0 for cysts. (Reproduced with permission from Greenough et al.2)
Differential Diagnosis/Diagnostic Algorithm
The absence of the typical history for BPD (eg, extreme prematurity accompanied by mechanical ventilation), a family history of (undiagnosed) pulmonary diseases, or signs of additional malformations should lead to consideration of other differential diagnoses. These include members of the family of interstitial lung diseases (ILDs) in children. Compromised lung function can also be found in association with congenital heart disease, arterial hypertensive vasculopathy, or congenital lymphatic diseases, as well as in chromosomal disorders that result in impaired pulmonary growth. Pulmonary hypoplasia, as seen in congenital diaphragmatic hernia, and surfactant dysfunction disorders should also be included in the differential diagnoses. Rare diseases, including neuroendocrine cell hyperplasia of infancy and pulmonary interstitial glycogenesis, as well as opportunistic infections in potentially immunocompromised patients also need to be considered.
PREPARATION, PRETREATMENT, AND PRE-WORKUP MANAGEMENT
Consent, Assent, and Ethical Considerations
Ethical considerations need to include long-term perspectives in patients at a high risk to develop severe BPD in association with other complications of prematurity, such as intraventricular hemorrhage (IVH), necrotizing enterocolitis (NEC), or severe infections that critically influence pulmonary as well as neurologic long-term outcome.
Monitoring for Treatment, Procedure, and Workup
Treatment monitoring has to include indicating acute and long-term outcome in this patient cohort. Need for supplemental oxygen and oxygenation, days with ventilator support, and lung function parameters define acute treatment response. Survival without BPD, abnormal lung function, clinical signs of pulmonary impairment (eg, hospitalization, infections), or even death characterize long-term therapeutic effectiveness.
Sedation/Pain Control Considerations
Sedation and pain control medication may be needed under long-term ventilation. Their interference with the ability to ventilate and oxygenate as well as their potential impact on neurologic outcome has to be considered.
Laboratory
Tests should include monitoring of gas exchange by arterial blood gas analysis and arterial oxygen saturation (SaO2); monitoring of pH and pCO2 by capillary blood gas analysis; lung function testing to define compliance, airway resistance, and lung volume; as well as chest radiography to exclude atelectasis as a cause of pulmonary problems. Hematocrit and electrolytes, especially while on diuretic therapy, as well as alkaline phosphatase need to be monitored. The assessment of other variables, for example, NT-proBNP may be helpful to indicate pulmonary hypertension but need further validation before routine clinical use.
Cardiac Function
Echocardiography and electrocardiography (ECG) are used to assess cardiac function for possible cor pulmonale.
Measurements
Monitoring of somatic growth 2–3 times per week, including body weight, length, and head circumference, is needed to ensure appropriate growth and to help define adequate calorie intake.
TREATMENT PROCEDURE
Prevention
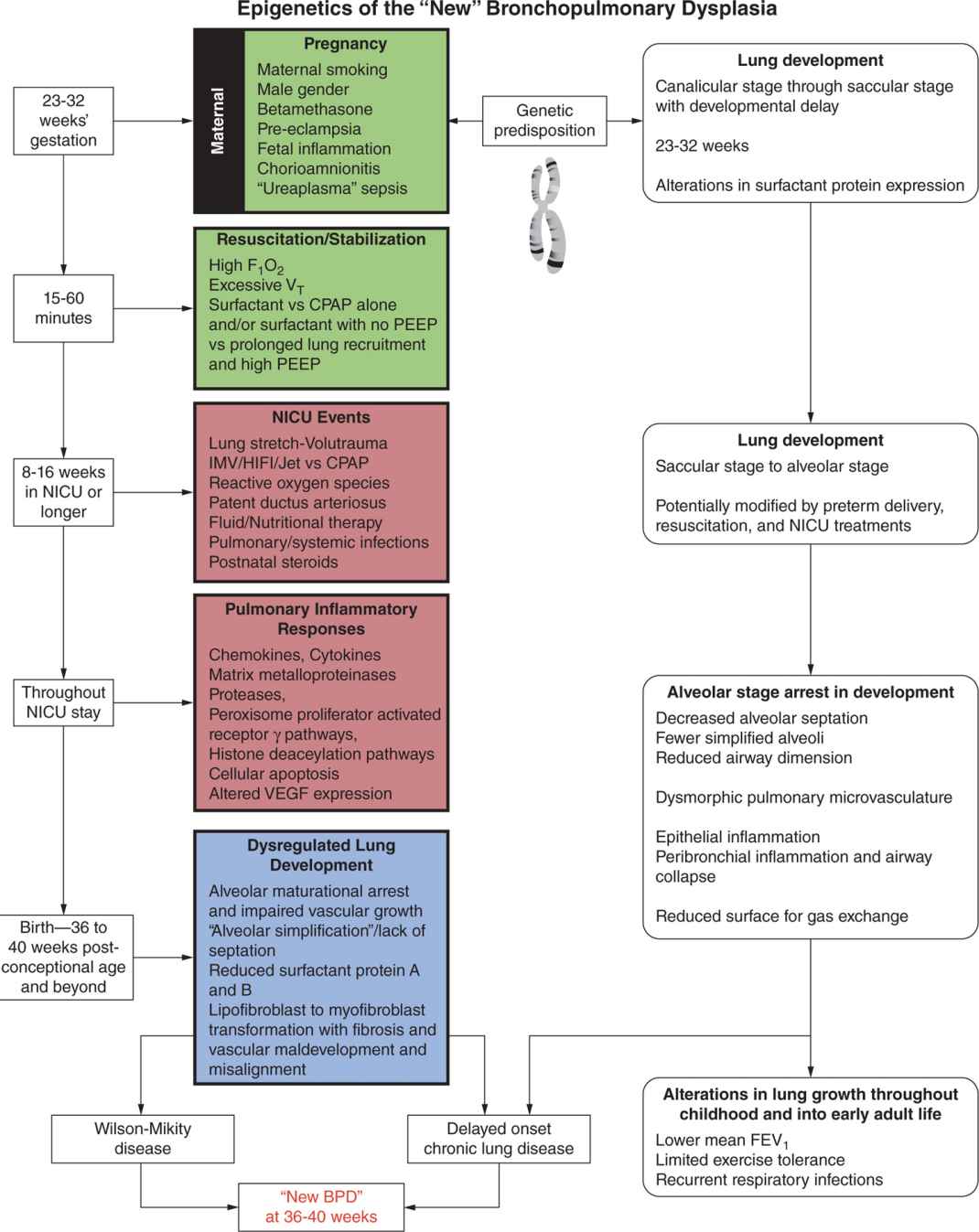
Administration of antenatal glucocorticoids and surfactant replacement therapy, routinely used in the care of premature infants, have been shown to reduce the risk for BPD. Figure 86-2 summarizes contributing factors. Most treatment strategies aim at preventing their impact in order to minimize further injury of the immature lung, thereby decreasing the risk for BPD.
FIGURE 86-2 Multiple factors contributing to the epigenetics of the “new” bronchopulmonary dysplasia (BPD) associated with lung development and gestational and postnatal developmental periods. FIO2, fraction of inspired oxygen; VT, tidal volume; CPAP, continuous positive airway pressure; PEEP, positive end-expiratory pressure; NICU, neonatal intensive care unit; IMV, invasive mechanical ventilation; HIFI, High Frequency Ventilation in Premature Infants study; VEGF, vascular endothelial growth factor; FEV1, forced expiratory volume in 1 second. (Reproduced with permission from Merritt et al.3)
Infection Management
The presence of severe prenatal infections increases the risk for preterm delivery and BPD development. Postnatally, careful and frequent evaluations to detect early signs of infection, meticulous monitoring of aseptic technique in infant handling, management of ventilator circuits and airway care, as well as early initiation of appropriate antimicrobial treatment of infection are critical issues in helping to reduce the incidence and severity of BPD. Routine use of erythromycin or azithromycin for eradication of Ureaplasma or Chlamydia species cannot be recommended thus far.
Mechanical Ventilation
The strategy for mechanical ventilation of premature infants should include low positive inspiratory pressure (PIP), relatively short inspiratory times, sufficient positive end-expiratory pressures (PEEP) and low tidal volumes (4–6 mL/kg), which may require higher rates of ventilation to ensure adequate minute volumes. Proper heating and humidification of the inspired gas and caution with endotracheal tube suctioning, which provokes lung collapse, are important considerations for preventing airway injury. Permissive hypercapnia, with PaCO2 as high as 55 or 60 mm Hg as long as the pH was 7.25 or greater, remains controversial and should be applied with caution. Weaning from mechanical ventilation should focus on reducing PIP and tidal volume prior to decreasing the respirator rate to avoid lung overdistention. Cessation of invasive ventilation should be considered as early as possible to reduce the incidence of supplemental oxygen therapy at 28 days as well as number of days on mechanical ventilation. Following extubation, frequent desaturations caused by apneic episodes and limited pulmonary capacity can be prevented by application of continuous positive airway pressure (CPAP) or noninvasive positive pressure ventilation (NIPPV). Treatment with caffeine should be initiated before extubation to reduce the risk of apnea and to potentially reduce the incidence of BPD.
Oxygen Therapy
Although it is important to reduce the inspired O2 concentration quickly if the oxygen saturation is greater than 96% or if the PaO2 is greater than 80 mm Hg, targeting an SpO2 of 85%–89% in immature babies was associated with slightly increased mortality rates and therefore cannot currently be recommended. Common practice to date is to maintain PaO2 above 55 mm Hg. SaO2 needs to be correlated with the PaO2, and in general SaO2 should be maintained between 90% and 95% to reach an appropriate PaO2.
Transfusion
Hematocrit should be maintained at approximately 30%–35% as long as supplemental oxygen is needed.
Nitric Oxide
In case of severe pulmonary hypertension in the early or later course of the disease, iNO can be considered. However, a treatment regimen using iNO as a rescue therapy did not reduce the incidence of BPD. Prophylactic application cannot be recommended to prevent the development of BPD. If applied, iNO treatment has to be performed under close monitoring for potential toxicities of iNO therapy, including interference with normal platelet function. Furthermore, side effects of iNO, including oxidant lung injury and loss of surfactant function resulting from the production of peroxynitrite, as well as long-term neurodevelopmental disability have to be considered prior to the institution of therapy.
Steroids
Treatment with potent anti-inflammatory steroids (eg, dexamethasone) to facilitate weaning from mechanical ventilation is currently contraindicated as it was found to be associated with an increased incidence of cerebral palsy and poor neurologic outcome.4 Current recommendations are to reserve the use of dexamethasone as a last resort in infants who cannot otherwise be weaned from mechanical ventilation. In these cases a short, low-dose regimen aimed at increasing the weaning rate in extremely low birth weight infants should be employed. Complications of dexamethasone treatment include glucose intolerance, systemic hypertension, and transient catabolic state. Total neutrophil counts and platelet counts may increase during treatment. Hypertrophic cardiomyopathy sometimes occurs, but is transient, as well as adrenal suppression. Hydrocortisone can be used in the first days of life for fluid-resistant arterial hypotension. Furthermore, short courses of hydrocortisone have been shown to significantly decrease mortality and improve survival of preterm infants with a history of chorioamnionitis without increasing the risk of BPD, suppressing adrenal function, or compromising short-term growth. Such therapy can be preceded by an ACTH (corticotropin) stimulation test (1 μg/kg test dose). Interestingly, however, low cortisol levels were not predictive of adverse long-term outcomes, and high cortisol concentrations, although predictive of short-term adverse outcomes such as IVH and periventricular leukomalacia, did also not predict adverse outcome. Inhaled steroids, as well as bronchodilators, currently cannot be recommended for treatment or prevention of BPD other than in cases of symptomatic bronchoconstriction.
Bronchoscopy
In case of stridor or persistent respiratory distress, vocal cord injury, associated with either patent ductus arteriosus (PDA) ligation or prolonged ventilation, hemangiomas, subglottic stenosis, or other structural problems need to be excluded. Bronchoscopy, or endoscopy with small devices through the nose, can facilitate the diagnosis.
Cardiovascular System
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree