INTRODUCTION
Many problems following surgery can be avoided by the preoperative risk assessment and prevention strategies described in Chapter 39. However, despite ideal preparation, complications may still develop, and vigilance for these adverse events can help ensure successful convalescence for most patients.
POSTOPERATIVE ORDERS
These written instructions address support of each organ system, while normal function is gradually reestablished. Although orders are customized for each woman, goals are common among all surgical patients—resuscitation, pain control, and resumption of daily activities. Table 42-1 offers a template for both inpatient and outpatient postoperative orders.
| Postoperative Orders (Inpatient) | Postoperative Orders (Outpatient) |
| Admit to: recovery room/assigned hospital floor/attending physician’s name | Admit to: recovery room; transfer to DSU when cleared by anesthesia |
| Diagnosis: s/p what surgical procedure | Diagnosis: s/p what surgical procedure |
| Condition: stable | Condition: stable |
| Vital signs: q1h × 4, q2h × 2, then q4h | VS per routine |
| Activity: bed rest | Allergies: NKDA |
| Allergies: NKDA | Bed rest until A&A, then activity ad lib |
| Notify MD for: T >101°F; BP >160/110, < 90/60; P >130; RR >30, <10; UOP < 120 mL/4 hr; acute changes | NPO until A&A, then clear liquids IV fluids: LR at 125 mL/hr until tolerating PO, then D/C IV |
| Diet: NPO except ice chips IV fluids: LR at 125/hr | Notify MD for: T >101°F; BP >160/110, <90/60; P >130; RR >30, <10; acute changes |
Special:
| D/C patient home when A&A, cleared by anesthesia, taking PO, ambulating, and able to void F/U at ___________ clinic in _____ weeks Write any necessary prescriptions |
Medications:
| |
| Labs: H & H in AM (or that afternoon if necessary) |
Nearly half of the average female body’s weight is water. Two thirds of this water is contained in the intracellular compartment, and the remainder is stored extracellularly. This extracellular compartment is divided into a vascular space filled with plasma and an interstitium, which is the collection of small spaces between cells. Of extracellular fluid volume, 25 percent makes up intravascular plasma, and 75 percent fills the interstitium. This 1 to 3 ratio is relevant during fluid resuscitation. Extracellular compartment osmolarity is controlled primarily by sodium and chloride, whereas potassium, magnesium, and phosphate are the major intracellular electrolytes. Osmotic balance is maintained by the free movement of water between the intra- and extracellular spaces.
To support these fluid volumes, the daily liquid requirement for an average adult approximates 30 mL/kg/day. Urine output and insensible losses offset these requirements (Marino, 2007). Thus, postoperatively, crystalloid fluids are primarily used for maintenance and in some cases for resuscitation. Sodium chloride is the main component of these fluids. Because sodium is most abundant in the extracellular space, the fluid is uniformly distributed between the interstitial areas. With crystalloid resuscitation, the primary effect is interstitial volume expansion rather than plasma volume growth. Two of the most commonly used crystalloid fluids for resuscitation and maintenance requirements are isotonic saline and lactated Ringer solution.
Compared with plasma, isotonic saline, also colloquially called normal saline, has a higher chloride concentration (154 mEq/L versus 103 mEq/L) and lower pH (5.7 versus 7.4). Thus, if isotonic saline is infused at large volumes, it can result in a hyperchloremic metabolic acidosis (Prough, 1999). The saline-induced acidosis usually has no adverse clinical consequences, but differentiating it from lactic acidosis (a marker of tissue necrosis) can be challenging in certain settings. Gastric secretions lost during vomiting or nasogastric tube suctioning are commonly replaced by a 5-percent dextrose in 0.45-percent normal saline solution with 20 mEq/L KCl added.
Also known as Hartmann solution, lactated Ringer solution contains potassium and calcium concentrations similar to plasma, but the sodium concentration (130 mEq) is comparatively reduced to that of isotonic saline to maintain cationic neutrality. The addition of 28 mEq/L of lactate necessitates a reduction in chloride concentrations to a level similar to plasma. In sum, the hyperchloremic metabolic acidosis risk observed with large-volume isotonic saline infusion is avoided. Disadvantageously, lactated Ringer solution leads to increased calcium binding of certain drugs that limits their efficacy (Griffith, 1986). Moreover, calcium can bind the citrated anticoagulant found in blood products and promote clot formation in donor blood. Advantageously, lactated Ringer solution does not significantly change serum lactate levels because only 25 percent of the infused volume remains intravascular. Therefore lactated Ringer solution is commonly employed in cases of isotonic dehydration, such as bowel sequestration in times of obstruction.
Postoperative pain management remains undervalued, and many patients continue to experience intense pain after surgery. A survey by Apfelbaum and colleagues (2003) revealed that more than 85 percent of respondents following surgery have moderate to severe pain. Poor pain control leads to decreased satisfaction with care, prolonged recovery time, increased use of health care resources, and increased costs (Joshi, 2005; McIntosh, 2009). Options for patient analgesia may be broadly classed as opiate-based or nonopioid.
The two major classes of nonopioid therapies are acetaminophen and nonsteroidal antiinflammatory drugs (NSAIDs). Multimodal pain control postoperatively using intravenous (IV) NSAIDs and/or acetaminophen can reduce or enhance analgesia, lower narcotic needs, decrease the incidence of postoperative nausea and vomiting by as much as 30 percent, and reduce hospital length of stay (Akarsu, 2004; Chan, 1996; Khalili, 2013; Mixter, 1998; Santoso, 2014). In general, these drugs are well tolerated and carry a low risk of serious side effects. However, acetaminophen can be toxic to the liver in high doses. Thus, patients should avoid total doses exceeding 4000 mg/day and use of alcohol while taking acetaminophen-containing products (Food and Drug Administration, 2011). A list of oral NSAIDs and their dosages are found in Table 10-1.
Despite the common side effects that all opiates share—respiratory depression and nausea and vomiting—opiate therapy is the primary choice for managing moderate to severe pain. The three most common opiates prescribed after gynecologic surgeries are morphine, fentanyl, and hydromorphone. Meperidine, although commonly administered in many obstetric units, is avoided in part because of neurologic side effects associated with its active metabolite, normeperidine. Normeperidine is a cerebral irritant that can cause effects ranging from irritability and agitation to seizure.
Morphine is prescribed most frequently following gynecologic surgery and is a potent μ-opiate-receptor agonist. Action at this receptor accounts for the analgesia, euphoria, respiratory depression, and decreased gastrointestinal (GI) motility seen with morphine. Onset of action is rapid, and peak effects are seen within 20 minutes of IV administration. Its action typically lasts for 3 to 4 hours. Its active metabolite, morphine-6-glucuronide, is renally excreted and thus is well tolerated in low doses in those with liver disease.
Pruritus is common after administration, although its genesis is poorly understood. Some investigators theorize that central opiate receptors are stimulated, whereas others speculate a histamine release as evidenced by urticaria, wheals, and flushing. In these cases, changing to another pain medication is logical. For pruritus treatment, most evidence-based data derive from studies of regional analgesia. Success has been found with ondansetron, 4 mg IV (George, 2009). Antihistamines, such as diphenhydramine (Benadryl) 25 mg IV, are another option. Naloxone, an opioid antagonist, can be used but may reverse the analgesia provided by morphine.
Fentanyl, a potent synthetic opiate, is more lipophilic than morphine and displays a shorter duration of action and half-life. Peak analgesia is reached within minutes of IV administration and lasts for 30 to 60 minutes. Many conscious sedation protocols used during office gynecologic procedures combine fentanyl with a sedative such as midazolam (Versed).
Hydromorphone (Dilaudid), another semisynthetic analogue of morphine, is less lipophilic than fentanyl. It is available for delivery by multiple routes, including oral, intramuscular (IM), IV, rectal, and subcutaneous (SC). Hydromorphone achieves its peak analgesia 15 minutes after IV administration, and its effects last 3 to 4 hours. Although commonly used during epidural analgesia, hydromorphone is a suitable patient-controlled analgesia (PCA) alternative in patients with a morphine allergy. Table 42-2 provides a summary of various pain medications and dosage equivalents.
| Drugs | Approximate Opioid Equianalgesic Dose | Usual Starting Dose | |||||
| Adults >50 kg Body Wt | Children and Adults <50 kg | ||||||
| Parenteral (mg) | Oral (mg) | Duration (h) | Parenteral | Oral | Parenteral | Oral | |
| Morphine IR (Roxanol) | 10 | 30 | 3–4 | 10 mg | 30 mg | 0.1 mg/kg | 0.3 mg/kg |
| Morphine SR (Oramorph) (MS Contin) | — | 30 | 8–12 | — | 30 mg | — | 0.3 mg/kg |
| Meperidine (Demerol) | 75 | 300 | 2–3 | 100 mg | NR | 0.75 mg/kg | NR |
| Hydromorphone (Dilaudid) | 1.5 | 7.5 | 3–4 | 1.5 mg | 6 mg | 0.015 mg/kg | 0.06 mg/kg |
| Codeine | 130 | 200 | 3–4 | 60 mg (IM/SC) | 60 mg | NR | 1 mg/kg |
| Oxycodone IR (Roxicet) a (Percocet) a | — | 30 | 3–4 | NA | 10 mg | NA | 0.2 mg/kg |
| Oxycodone SR (OxyContin) | — | 30 | 8–12 | NA | 10 mg | NA | 0.2 mg/kg |
| Hydrocodone (Lorcet) a (Lortab) a (Vicodin) | NA | 30 | 6–8 | NA | 10 mg | NA | 0.2 mg/kg |
| Methadone (Dolophine) | 10 | 20 | 3–4 | 10 mg | 20 mg | 0.1 mg/kg | 0.2 mg/kg |
| Fentanyl (Sublimaze) (Duragesic) | 0.1 | — | 1 | 0.1 mg | — | — | — |
Some women will have significant menopausal symptoms after surgical removal of both ovaries. Symptoms can range from severe hot flashes to headaches or sudden mood swings. In these women, estrogen replacement therapy is considered for those without contraindications (Chap. 22). For women completing surgery for endometriosis, a progestin may be added for those with residual disease, as discussed in Chapter 10.
PULMONARY COMPLICATIONS
Broad definitions hinder our ability to accurately assess the incidence of postoperative pulmonary complications, but reported estimates range from 9 to 69 percent (Calligaro, 1993; Hall, 1991). Postoperative pulmonary complications include atelectasis, pulmonary embolism (PE), and less commonly, pneumonia and acute respiratory distress syndrome (ARDS). All can potentially lead to acute respiratory failure.
In the general postsurgical population, acute respiratory failure (ARF) has an incidence ranging from 0.2 to 3.0 percent and an associated mortality rate that can exceed 25 percent (Arozullah, 2000; Johnson, 2007). ARF is classically divided into four subtypes defined by inadequate exchange of oxygen or carbon dioxide or both. Type 1 lesions exchange oxygen poorly, and examples include atelectasis, pneumonia, PE, and ARDS, all discussed subsequently.
Type 2 is typified by hypercapnia. It is seen in anesthesia overdose and muscle fatigue, in which ventilation suffers and carbon dioxide (CO2) is retained. Also, increased metabolic processes such as fever, severe sepsis, overfeeding, and hyperthyroidism can generate excess CO2. As a result, ventilatory work increases as the body attempts to maintain appropriate arterial pCO2 levels. This can ultimately lead to respiratory failure.
Type 3 is similar to type 1 but merits a distinct category because of its common occurrence following anesthesia and surgery. Physiologically, general anesthesia reduces muscle tone to decrease lung volumes and airway diameters. The resulting atelectasis and airway closure can drive abnormal gas exchange and ventilation-perfusion mismatching, which creates a decrease in PaO2. This hypoxemia is further aggravated by hypoventilation from central decreases in respiratory drive, residual effects of anesthetics, lung edema, or bronchospasm (Canet, 1989). To help circumvent type 3 ARF, important considerations include early treatment of hypoxemia, multimodal approaches to pain management, and chest physiotherapy.
Type 4 stems from shock and its associated cardiopulmonary hypoperfusion. For treatment, circulatory resuscitation, discussed in Chapter 40, accompanies oxygen therapy.
This reversible closure or collapse of alveoli is seen in 90 percent of surgical patients (Lundquist, 1995). Development is associated with decreased lung compliance, gas exchange abnormalities, and increased pulmonary vascular resistance. Thus, characteristic signs are diminished breath sounds, dullness to percussion over affected lung fields, and decreased oxygenation. Pulse oximetry readings >92 percent represent adequate oxygenation, however, a PaO2 measurement by arterial blood gas will most accurately assess a patient with hypoxic respiratory failure. In addition to bedside findings, chest radiography typically shows linear densities in the lower lung fields. Classically, atelectasis is associated with low-grade fevers. However, Mavros and colleagues (2011) reviewed eight studies with a total of 998 patients and found no association between atelectasis and postoperative fever.
Prevention using lung expansion therapies is described in Chapter 39, and these can be used for treatment as well. Atelectasis is usually temporary (up to 2 days) and self-limited, and it rarely slows patient recovery or hospital discharge (Platell, 1997). Its importance mainly lies in its clinical similarity to PE and pneumonia. Thus, in women with risks for these more life-threatening complications, atelectasis may ultimately be a diagnosis of exclusion.
This is the second most common nosocomial infection in the United States and carries high associated morbidity and mortality rates (Tablan, 2004). Its incidence in surgical patients varies and ranges from 1 to 19 percent depending on surgical procedure and hospital surveyed (Kozlow, 2003). With these infections, bacterial pathogens most typically include aerobic gram-negative bacilli, such as Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, and Acinetobacter species.
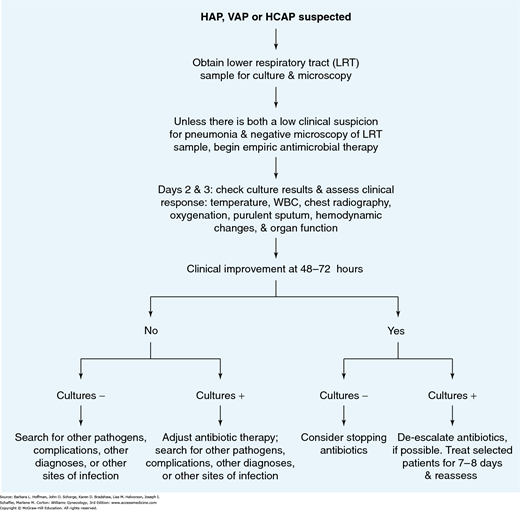
Clinically, pneumonia is diagnosed if chest radiography reveals a new or progressive radiographic infiltrate and if two of three clinical features (leukocytosis, fever >38°C, or purulent secretions) are present. Broad-spectrum antibiotic regimens are recommended for hospital-acquired pneumonia treatment (Table 42-3). If aspiration is highly suspected, specific treatment for anaerobes with metronidazole or clindamycin is considered. An algorithm supported by the American Thoracic Society is shown in Figure 42-1. Preventive steps include substituting oral endotracheal and orogastric tubes in place of nasal tubes; elevating the head of the bed 30 to 45 degrees, particularly during feeding; and removing subglottic secretions in those unable to clear these (American Thoracic Society, 2005; Ferrer, 2010).
| Regimen Options | Dosage |
| Cefepime or ceftazidime | 2 g every 8 hr |
| or | |
| Imipenem or meropenem | 1 g every 8 hr |
| or | |
| Piperacillin–tazobactam | 4.5 g every 6 hr |
| PLUS | |
| Aminoglycoside | |
| Gentamicin | 7 mg/kg/d |
| Tobramycin | 7 mg/kg/d |
| Amikacin | 20 mg/kg/d |
| or | |
| Quinolone | |
| Levofloxacin | 750 mg daily |
| Ciprofloxacin | 400 mg every 8 hr |
FIGURE 42-1
Algorithm describes management strategies for hospital-acquired pneumonia. HAP = hospital-acquired pneumonia; HCAP = health care-associated pneumonia; VAP = ventilator-associated pneumonia; WBC = white blood cells. (Reproduced with permission from American Thoracic Society: Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005 Feb 15;171(4):388–416.)
If venous thromboembolism (VTE) is suspected, evaluation begins with clinical examination and risk estimation. Wells and colleagues (1995) described one of the most widely used pretest probability assessments for DVT (Table 42-4). When indicated, duplex sonography is highly sensitive for detecting proximal leg DVTs, with a false-negative rate of 0 to 6 percent (Gottlieb, 1999).
| Major Points | Minor Points |
| Cancer Immobilization Recent major surgery Thigh or calf tenderness Calf swelling Family history of DVT | Recent trauma to symptomatic leg Unilateral edema Erythema Dilated superficial veins Hospitalized in last 6 months |
| Clinical Probability | |
| High | |
| >3 major points and no alternative diagnosis >2 major points and >2 minor points + no alternative diagnosis | |
| Low | |
| 1 major point + >2 minor points + has an alternative diagnosis 1 major point + >1 minor point + no alternative diagnosis 0 major points + >3 minor points + has an alternative diagnosis 0 major points + >2 minor points + no alternative diagnosis | |
| Moderate | |
| All other combinations | |
For PE, because symptoms may reflect other cardiopulmonary pathology, clinicians often initially elect chest radiography and electrocardiogram (ECG). The radiograph is typically abnormal but nonspecific, and findings can include atelectasis, elevated hemidiaphragm, cardiomegaly, and small pleural effusions (Worsley, 1993). ECG may display tachycardia or may reflect right heart strain by showing a large S wave in lead I, a Q wave in lead III, and inverted T wave in lead III (Stein, 1991). If suspicion for PE remains, then computed tomographic angiography (CTA) or less frequently, ventilation/perfusion (V/Q) scanning is ordered. These serve as alternatives to the invasive gold standards—pulmonary angiography or contrast venography.
Acute management of VTE involves anticoagulation with intravenous unfractionated heparin or subcutaneous low-molecular-weight heparin (Tables 42-5 and 42-6). After achieving adequate anticoagulation, oral vitamin K antagonists such as warfarin are initiated. To avoid paradoxical hypercoagulability, heparin is continued for at least 5 days after the initiation of warfarin (Houman Fekrazad, 2009). Once the international normalized ratio (INR) reaches a therapeutic range of 2 to 3, then heparin is stopped. Long term, anticoagulation therapy duration is dictated by clinical and patient circumstances. For those with a provoked first DVT or PE, anticoagulants are recommended for 3 months. Provocateurs include surgery, exogenous estrogen, or local trauma. Extended therapy is preferred for both those with unprovoked VTE or with second VTE, unless the risk of bleeding is high, in which case, treatment is halted at 3 months. For those with concurrent cancer, therapy is extended regardless of bleeding risk (Kearon, 2012).
| Initial Heparin Dose: | ||
| __ units IV push (recommended 80 units/kg rounded to nearest 100, maximum 7500 units), then | ||
| __ units/hr by infusion (recommended 18 units/kg/hr rounded to nearest 50). | ||
| Infusion Rate Adjustments—based on partial thromboplastin time (PTT): | ||
| PTT (sec) a <45 45–54 55–84 85–100 >100 | Intervention b 80 units/kg bolus 40 units/kg bolus None None Stop infusion 60 minutes | Baseline Infusion Rate Change c ↑by 4 units/kg/hr ↑by 2 units/kg/hr None ↓by 2 units/kg/hr ↓by 3 units/kg/hr |
Acute lung injury that causes a form of severe permeability pulmonary edema and ARF is termed acute respiratory distress syndrome. This is a pathophysiologic continuum from mild pulmonary insufficiency to dependence on high inspired oxygen concentrations and mechanical ventilation. The theory that multiple insults lead to postoperative ARDS offers insight into modifiable intra- and postoperative alveolar damage prevention (Litell, 2011; Warner, 2000). Intraoperative strategies minimize lung trauma by keeping airway pressure and tidal volumes within set limits and by avoiding repeated alveolar opening and closing (Hemmes, 2013). Other measures strive to prevent infection, limit IV fluid volumes, and avoid blood product transfusion (Güldner, 2013).
CARDIAC COMPLICATIONS
Postoperative myocardial infarction (MI) is rare, and its generally reported incidence ranges from nearly 1 percent to as high as 37 percent among patients with surgery within 3 months following an MI (Mangano, 1990; Tinker, 1978). Declines in oxygen supply and increased demand classically underlie this coronary ischemia. Events that decrease oxygen supply include hypotension, lowered coronary perfusion, or poor carrying capacity caused by anemia. Increased afterload, tachycardia, and increased cardiac contractility can raise myocardial oxygen demands.
Most patients with postoperative MI do not have classic symptoms of chest pain or pressure. These are in part masked by postoperative analgesics (Muir, 1991). Dyspnea is the most common complaint and may be accompanied by acute cardiac failure or hemodynamic instability. ECG changes of postoperative MI tend to be less well defined, and most demonstrate a non-Q wave variant (Badner, 1998). CK isoenzyme (CK-MB) abnormalities are seen within 6 hours, and cardiac troponin I and T are highly specific later for diagnosis of MI (Zimmerman, 1999).
Postoperative MI treatment differs from that of nonsurgical patients, and its main tenets focus on shifting the oxygen delivery and utilization balance. Special attention is given to arrhythmia correction and hemodynamic status improvement. Ideally, these patients are cared for in a unit that provides intense monitoring, cardiopulmonary support, and cardiology consultation.
This is frequently encountered both preoperatively and postoperatively. As standard definitions are lacking, the reported incidence ranges from 3 to 90 percent, depending on the thresholds set and the type of surgery. Patients with poorly controlled hypertension preoperatively tend to have more blood pressure lability compared with normotensive patients or those with well-controlled hypertension. In general, a diastolic blood pressure greater than 110 mm Hg preoperatively best predicts those who will have postoperative hypertension issues.
Several possible triggers may raise blood pressures in the first 24 hours after surgery. First, abrupt withdrawal of β-blocker or of centrally acting sympatholytic agents such as clonidine can cause rebound hypertension. Pain and bladder distention may also contribute. Later in postoperative recovery, sympathetic hyperactivity may stem from inadequate pain management or from alcohol withdrawal. Last, return of excess interstitial fluid back into the vascular space may create fluid overload and hypertension.
Two approaches have been described for blood pressure treatment: fixed thresholds and relative changes from baseline. Charlson and colleagues (1990) demonstrated increased rates of postoperative cardiac and renal complications when the mean blood pressure rose 20 percent or more compared with preoperative levels. Given the paucity of good evidence, it is reasonable to initiate treatment if mean blood pressure readings rise by this percentage. With acute blood pressure management, the mean blood pressure should not be lowered by more than 20 percent or to a level less than 160/100 mm Hg.
GASTROINTESTINAL COMPLICATIONS
This is one of the most common complaints following surgery, and its incidence ranges from 30 to 70 percent in high-risk patients (Møller, 2002). Those at risk for postoperative nausea and vomiting (PONV) include females, nonsmokers, those with prior motion sickness or prior PONV, and those with extended surgeries (Apfelbaum, 2003).
A multimodal approach to prevention is recommended (Apfel, 2004). Currently, combinations of 4 to 8 mg of dexamethasone prior to anesthesia induction are followed, toward the end of surgery, by less than 1 mg of droperidol (Inapsine) and 4 mg of ondansetron (Zofran). This pretreatment significantly reduces symptoms by 25 percent. However, if symptoms develop within 6 hours of surgery, antiemetics from a different pharmacologic class than previously administered are considered (Habib, 2004). Persistent nausea may benefit from combining agents from different classes (Table 42-7).
| Medication (Brand Name) | Usual Dosage | Route(s) |
| Antihistamines | Every 6 hr | |
| Diphenhydramine (Benadryl) | 25–50 mg | IM, IV, PO |
| Hydroxyzine (Atarax, Vistaril) | 25–100 mg | IM, PO |
| Meclizine (Antivert) | 25–50 mg | PO |
| Benzamides | Every 6 hr | |
| Metoclopramide (Reglan) | 5–15 mg | IM, IV, PO |